Abstract
Insufficient data from existing surveillance systems underlie societal tolerance of acute and slow-onset health disasters that threaten, harm, and kill vast numbers of humans, animals, and plants. Here we describe barriers to integrated “One Health” surveillance, including those related to a lack of medical services, professional divisions, incompatible vocabularies, isolated data sets, and territorial borders. We draw from publications of experts who justify broader and more integrated surveillance, education, and stewardship focused on preventing and mitigating disease emergence and re-emergence. In addition, we highlight efforts from Illinois, the United States and the broader world, pointing to examples of relevant education; ways to acquire, compile, and analyze diagnostic and syndromic data; mapping of diseases of humans and animals; and rapid communication of findings and recommendations. For the future, we propose using needed outcomes for health and sustainability to set priorities for One Health programs of education, surveillance, and stewardship. Professionals and paraprofessionals should gather, interpret, and widely communicate the implications of data, not only on infectious diseases, but also on toxic agents, malnutrition, ecological damage, the grave impacts of warfare, societal drivers underlying these problems, and the effectiveness of specific countermeasures.
Similar content being viewed by others
Introduction
Relatively few scholars would question that we live in an era of unmet One Health challenges. Humans, domestic and wild animals, and plants concurrently suffer impacts from emerging and re-emerging infections, toxicant exposures, environmental mismanagement, climate change, warfare, economic and political failings, and a lack of expertise needed to implement the needed solutions. But, many would question why societies fail to identify and counteract such phenomena earlier and more effectively. Many would ask what efforts demonstrate promise in One Health surveillance now and whether they can be applied more broadly. No doubt, a great many would inquire as to how future generations can reliably organize their systems of education, professional interactions, governance, incentives, and disincentives to create a world characterized by steady gains in One Health. Here we endeavor to offer answers to these open questions.
Methods
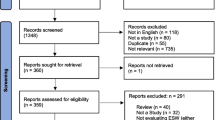
Narrative reviews have merit, particularly when they unify a wide array of perspectives on important concerns into readable documents that expand understanding, not only of problems, but also of feasible options for their management (Murphy 2012). We undertook a narrative review of a wide variety of authoritative information sources focusing on diverse stressors that undermine human, domestic animal, wildlife, plant, and ecosystem health as well as on ways by which such stressors can be better understood, quantified, and countered. In this effort, we relied upon Google Scholar, Google, PubMed, articles cited in writings found with those search tools, and citations gathered through direct communications with a range of experts. Our objectives were to examine the literature to identify important problems caused by a lack of One Health surveillance, barriers that undermine integrated surveillance, and functional multi-species surveillance programs that are overcoming such impacts and barriers around the world. Finally, we undertook a de novo synthesis of recommendations to support development of a nested system of One Health surveillance that can be adapted and refined for the near- and long-term future.
Why One Health?
One Health is a term needed to accommodate the functional inseparability of human, animal, plant, and ecosystem health (Barrett and Osofsky 2013; Mackenzie et al. 2013; Nielsen et al. 2012; Zinsstag et al. 2011; United Nations 2014; Aguirre et al. 2002, 2012; Chivian and Bernstein 2008; Norrgren and Levengood 2012). Bridging health expertise has occurred for millennia but responses to today’s unprecedented challenges necessitate more inclusive collaborations (Klauder 1958; Schwabe 1964; Beasley 1993, 2009; Zinsstag et al. 2011; Beasley and Adkesson 2012; Sleeman 2013; Rubin et al. 2014). Accordingly, a number of organizations have formally recognized shared One Health responsibilities, including the American Medical Association, American Veterinary Medical Association (AVMA), American Academy of Pediatrics, American Nurses Association, American Association of Public Health Physicians, American Society of Tropical Medicine and Hygiene, Association of American Veterinary Medical Colleges (AAVMC), U.S. Centers for Disease Control and Prevention (CDC), U.S. Department of Agriculture (USDA), and U.S. National Environmental Health Association (One Health Initiative 2014).
As described below, the high costs of today’s shared health impacts call for synchronous interventions. Beasley and Adkesson (2012) highlighted pathways toward essential One Health outcomes, including regulated atmospheric CO2, prevention of conflict, limiting human population size, prevention of chemical poisoning, sustainable food production, reduced risks of infectious diseases, and recoveries of aquatic and terrestrial biodiversity. Surveillance to quantify progress toward those outcomes is a logical first step. In this time of economically constrained resources, One Health is becoming an umbrella for coordinated surveillance, prioritized research, and targeted interventions needed to solve multiple problems at once.
Stressors that Are Often Ignored in Today’s Narrow Health Surveillance
Current surveillance systems often ignore or gloss over widespread, multi-species health stressors including warfare; overpopulated slums lacking waste, water, and food safety infrastructure; “wildlife ghettoes” where animals crowd into habitat fragments; exotic and invasive species; overharvest of wildlife; obsolete methods in plant and animal agriculture; rapid transport of pathogens; climate change; and even ubiquitous chemical contaminants.
Environmental Contaminants
Nutrient, pesticide, mining, industrial, construction-related, and vehicle-produced pollution can degrade aquatic and terrestrial—including—human life (Alexander et al. 2012). Nutrient pollution alone causes hypoxic and dead zones at the mouths of rivers around the world and is a contributor to a wide array of toxins in harmful algal blooms that affect aquatic and terrestrial species, including humans (Beasley 2011). Urban air pollution, including that from motor vehicles, is increasing in developing nations and has been estimated to account for approximately 3.7 million human deaths annually on a global basis, far more than are caused by HIV/AIDS (OECD 2014). Moreover, air pollution-associated human deaths and health problems including asthma, other lung disorders, and heart disease were estimated to have a global cost of over 3.5 trillion dollars annually. The failure to undertake systematic surveillance of contaminant emissions and concentrations in environmental media such as air and water, and to examine highly exposed and sensitive species, such as urban birds, for toxicant residues and impacts makes prioritized actions to protect their health difficult, and it prevents societies from being able to rely on them as early sentinels for threats to human health (Herrera-Dueñas et al. 2014).
An historic and ongoing example of a lack of One Health surveillance and failure to apply available countermeasures to protect multiple species is mercury. From 1932 onward, methylmercury was directly released into Minamata Bay off the coast of Japan. From 1949 through the 1960s, it killed fish, then birds, and finally cats and humans (Harada 1995). Today, mercury directly poisons communities of artisanal gold “miners” in Latin America, Asia, and Africa, and it contaminates food webs of streams where they work. Moreover, deglaciation, deforestation, and coal burning are releasing mercury into the atmosphere and aquatic ecosystems, exposing human and non-human consumers of fish and shellfish around the world. Despite these many problems, mercury surveillance remains largely an ad hoc research project-based endeavor (Schmidt 2012; Gibb and O’Leary 2014).
One Health includes research with laboratory animals to predict and avoid toxic harm to humans, domestic animals, wildlife and plants. However, only with pharmaceuticals does post-market surveillance routinely trigger rapid withdrawals of problematic formulations from the marketplace (Greener 2008). Surveillance for toxic injury to humans and especially non-humans from other types of chemicals is highly inconsistent in the developed world and largely absent in the developing world. Moreover, the effects of real-world exposures to chemical mixtures remain poorly understood and little studied, even for humans of the most advanced nations (Zeliger 2011). Because wild animals need to be in peak condition if they are to find and compete for niches, food and mates, successfully reproduce, and survive predators, infectious agents, climatic extremes, and other stressors, far more attention is needed to protecting them and their supporting ecosystems from contaminant impacts (deSwart et al. 1996; Carls et al. 1999; Rohr et al. 2008; Beasley 2011; Levengood and Beasley 2012; Di Prisco et al. 2013).
One Health Surveillance on the Risks of Warfare and Militarization
On a global basis, deaths from warfare have more than doubled since 1990 (Horton 2012; Lozano et al. 2012). The Rwandan genocide followed overpopulation, land shortages, and strife driven by a polarizing colonial legacy. Moreover, recent use of conventional and chemical weapons, e.g., in Africa and the Middle East, have cost hundreds of thousands of deaths, far more casualties, and trillions of dollars.
In the current era of high human populations and climatic instability, squandering money and human resources on militarization can contribute to high human mortality, even in the absence of overt conflict. For example, in North Korea, 0.24–3.5 million people died from malnutrition, sparked by overpopulation, wasting money and manpower on militarization, floods and droughts that harmed agriculture, food import dependency, and reductions in such imports from China due to its own shortages (Lozano et al. 2012).
Drs. Bernard Lown and Yevgeniy Chazov founded International Physicians for Prevention of Nuclear War, which used surveillance data from Japanese research following victims at Hiroshima and Nagasaki to estimate potential effects of blast force, incineration, and radiation from future nuclear wars. They were awarded the Nobel Peace Prize in 1985 after their open and compelling arguments prompted world powers to reduce their numbers of nuclear weapons and many nations to accept a “no-first-use” doctrine (Coulter 1992). Veterinarian David Waltner-Toews (1983) correctly called nuclear war suicide and stated that preventing nuclear war could do more for animal and human well-being than all the vaccinations in the world. Unfortunately, reports on the threats of nuclear warfare from medical professionals are rarely heard in today’s media, nuclear arsenals remain out of scale with any possible need in the most militarized of nations, and large numbers of nuclear weapons have been stockpiled in developing countries. A “small” nuclear war between Pakistan and India would cool the planet, damage the ozone layer, substantially reduce global food production, and potentially cause an economic depression lasting for decades. A full-scale nuclear war between Russia and the United States would block out the sun, plunge the world into sub-freezing temperatures, prevent virtually all plant growth, and result in mass starvation, and potential extinction of humans and myriad species of animals (Turco et al. 1984; Robock and Toon 2012). Quinlan (2007–8) recently described the complexity—as well as the necessity—of nuclear disarmament. An additional threat, biological warfare, potentially including agro-terrorism—targeting animal or plant health—could also devastate human, animal, and economic health (Herrmann 2012).
Surveillance on the risks and costs of warfare is an economic and moral necessity. Manpower and funding expended on avoidable wars should be redirected to such critical needs as discoveries of disease mechanisms, improvements in diets, medicines and vaccines, more efficient agriculture, and infrastructure for safe public water, sanitation, and transportation systems in concert with accelerated ecological restorations.
Surveillance as a Foundation for Restoration of Ecosystem Goods and Services
Compensating for today’s health stressors requires finding ways to restore ecosystem goods and services. Costanza et al. (1997, 2014) estimated that benefits of ecosystem goods and services roughly doubled global gross national product and stressed that environmental damage is decreasing their value. Ecological damage causes declines and extinctions of native wild species, as documented through surveillance by experts who provide data to the International Union for the Conservation of Nature (IUCN). Such losses of native plants and animals often have critically important secondary and tertiary effects on the health of other organisms (Vié et al. 2009; UNEP 2011; Ripple et al. 2014).
Ill-conceived levees, dams, channelization of rivers, wasteful forms of irrigation, and habitat losses to agriculture, monoculture forestry, urban sprawl, mining, industry, and roads undermine self-sustaining terrestrial populations of wild plants and animals. In concert with overfishing, overhunting, and chemical pollution, these phenomena deplete what were previously free and abundant, naturally produced foods that nourished myriad animal species—including humans. Among people, subsistence hunting and fishing communities are heavily impacted when such protein sources are lost, and conversion to cereal-dominated diets fails to meet nutritional needs. Inadequate animal-derived protein routinely causes malnutrition, poor health, and mortality among children in developing countries (Horton 2012; Lozano et al. 2012). The lack of animal-derived nutrients in diets of people have been linked to childhood anemia, impaired brain development, and diminished life-long stamina (Ahmed et al. 2012).
Stressors that are Often Under Today’s Rubric of One Health, and How the Vision of Related Needs is Being Broadened
Infectious Diseases: Etiologic Agents, Economic Costs, Societal Drivers, and Disease-Resilient Landscapes
Zoonotic pathogens cause most of the emerging infectious diseases (EIDs) in humans, and over 70% of them originate in wildlife (Jones et al. 2008; Conrad et al. 2009; Hill et al. 2012). Inadequate surveillance and preparedness for zoonotic disease threats contributed to the impacts of West Nile virus in the U.S. that included 37,000 human illnesses and 1500 deaths (CDC 2014); Q-fever in Europe, which sickened 2000 people and prompted culling of 40,000 goats; and Nipah virus in Malaysia that caused 100 human fatalities and culling of 1,000,000 swine (World Bank 2012). Marsh, Inc. (2008) estimated that, from 1995 to 2008, global costs of zoonotic EIDs exceeded $120 billion. Moreover, World Bank (2012) projected potential losses from one severe influenza pandemic of 71,000,000 human deaths and $3 trillion. Assessing this situation, Burgos and Slingenbergh (2011) wrote that, despite the “tectonic weight” of social and economic impacts, only negligible amounts are invested in better understanding zoonotic disease emergence.
The Global Burden of Disease study (GBD) focuses on human deaths, and it will soon feature continuously updated analyses as data become available (Horton 2012; Lozano et al. 2012). Ongoing deaths of children from respiratory infections, diarrhea, and malaria—due to crowding, lack of insect screens and vaccines, unprecedented storms and flooding potentially attributable to climate change and impoundments that increased standing water were described by GBD and Patz et al. (2003).
Between 1990 and 2010, despite anti-retroviral drugs, annual deaths from originally zoonotic HIV/AIDS increased from 0.3 to 1.5 million. Stepping back only slightly reveals the multi-species relevance of the GBD. For example, HIV/AIDS has enabled re-emergence of tuberculosis with high mortality, and tuberculosis from humans threatens endangered great apes. Moreover, multiple retroviruses circulate in people and non-human primates, and a simian immunodeficiency virus, closely related to HIV, is currently undermining highly endangered African chimpanzee populations (Rudicell et al. 2011).
To address One Health needs, the United Nations Food and Agricultural Organization (FAO), the World Health Organization (WHO), and the World Organisation for Animal Health (OIE) (2004) urged international cooperation among human and animal health sectors to detect and contain zoonotic diseases. World Bank (2012) assessed 23 nations, noting relationships between (a) competent veterinary and paraprofessional personnel and supplies of vaccines and medicines, and (b) prevention and containment of disease emergence/resurgence. To increase surveillance by animal health experts, they recommended funding from national governments (for salaries), international donors (for transparent disease reporting and financial accountability), endowments (for sustainability), and levies (on meat exports and pharmaceuticals). Moreover, the Institute of Medicine (IOM) (2007) called for active surveillance and rapid diagnoses of infectious causes of diseases of plants, animals, and humans. Going further, Burgos and Slingenbergh (2011) concluded that the only option is to expand surveillance to include societal drivers of disease outbreaks, such as human and livestock encroachment into habitats and high-risk exploitation of wildlife. To establish disease-resilient landscapes and sustainable agriculture they recommended new alliances, partnerships, and facilitated communications.
Barriers to One Health Surveillance
A recent book entitled “Zoobiquity” and related conferences point to the need to overcome professional snobbery and physical isolation that impair needed dialogs among human and animal (domestic and wild) health professionals (Natterson-Horowitz and Bowers 2013). The authors cite examples of diseases that have been recognized and managed in animal patients decades ahead of equivalent diseases in human patients. They also mention how, even now, the same conditions have entirely different names in human versus non-human animals. Below, we briefly address these and other barriers to One Health surveillance on a local to global basis, and we highlight efforts by which they are beginning to be overcome.
Underserved Populations
Lack of access to health care on the part of human and animal patients gravely undermines One Health surveillance (Stal et al. 2012). India’s physician-to-patient ratio is 6:10,000, and its rural areas that are home to 70% of its population are served by only 3% of its physician-specialists. Such communities rely on informal providers lacking training, skills, and medical supplies (Gopalakrishnan 2013). In response, non-governmental organizations (NGOs) link the informal providers to medical supply-chains, training, and telemedicine. Similarly, in many locations within developed and developing nations today, food and fiber animals are widely distributed and private veterinary services often fail economically, increasing risks to animal health and consumers of animal products.
In the US, efforts to provide greater numbers of physicians and other human health professionals to underserved populations include the educational loan repayment incentive programs of the National Health Services Corps (US Department of Health and Human Services 2014). A similar program from USDA offers significant repayment of educational loans to recently graduated veterinarians who agree to provide professional services to food animal owners in remote communities for at least 3 years (USDA National Institute of Food and Agriculture 2012). To complement and go beyond that program, the report, “Workforce Needs in Veterinary Medicine” [National Research Council (NRC) 2013], recommended deploying specially trained veterinary technicians linked via telemedicine to veterinary medical specialists. Such individuals are needed in locales around the world.
In the wildlife sector, current programs train rangers, managers, and biologists to recognize abnormalities and submit samples for diagnostic studies. For example, USDA’s Wildlife Services established the Surveillance and Emergency Response System, training 44 Wildlife Disease Biologists (WDBs) in foreign animal disease recognition, personal protective equipment, animal capture, postmortem sampling, and simulated emergency response mobilizations (USDA/APHIS/Wildlife Services 2008). Located at state USDA Wildlife Services facilities, WDBs share knowledge of diseases and risk management with federal, state, and district personnel.
Professional Divisions
Although public health practitioners, physicians, veterinarians, and wildlife/ecosystem experts are essential for One Health surveillance, mechanisms to unify their efforts are few, and instead forces drive them apart. Restrictive licensing, third-party financing rules that dictate which medical professionals can provide specific aspects of care, and disputes over methodology impair needed human health collaborations. Public health practitioners decry physicians’ “downstream” limitations, while physicians critique public health professionals’ “upstream” approach (Brandt and Gardner 2000). Barriers to joint surveillance by human and animal health experts also include isolation in different facilities, inadequate appreciation of unique knowledge and skills, and meager funding of veterinary practices, diagnostic laboratories, and research (Herrmann et al. 2011; NRC 2013). Wildlife health surveillance poses extraordinary logistical and economic challenges (Mörner and Beasley 2012). Unlike structured public and domestic animal health programs, there is comparatively very little methodological wildlife disease sampling, and reporting in most countries is required only for diseases of public health and agricultural importance (Friend 2006).
To increase critical professional collaborations, the report, “Operationalizing One Health”, recommended integration of public health with individual health: a core sector bridging humans, animals, and wildlife; collaborations among stakeholders in animal, human, and ecosystem health issues; transparent communications in rapid surveillance for emergent pathogens; co-locating schools of medicine, veterinary medicine, public health, and nursing; getting beyond biomedical confines to involve social scientists and economists; involving diverse students in zoonotic disease investigations; and piloting best management practices (CDC 2010).
Incompatible Vocabularies
Progress toward common vocabularies for One Health surveillance has begun but important deficits remain to be addressed. One system heavily relied upon by CDC is the Systematized Nomenclature of Medicine Clinical Terminology (SNOMED) (US National Library of Medicine 2014). SNOMED focuses largely on human health, is available in multiple languages, and is widely accessible free of charge. SNOMED hierarchies make sense for One Health surveillance: they include body structures, clinical findings/disorders and severity, organisms (e.g., pathogens), substances (e.g., toxicants, foods), physical objects, physical force, environmental and geographical locations, relevant events, social contexts, specimens obtained, and pharmaceutical/biological products given. The AVMA endorsed SNOMED as a “master language” for veterinary medicine, and efforts in animal health informatics, especially through SNOMED, are underway at the Veterinary Terminology Services Laboratory (VTSL) of Virginia–Maryland College of Veterinary Medicine. VTSL has worked with FDA, USDA, USGS, and veterinary practitioner organizations to enhance uses of, and additions to, SNOMED. Unfortunately, One Health surveillance is hindered because OIE has not yet embraced SNOMED. Also, SNOMED vocabularies should include more maladies of domestic and wild vertebrates, more terms for structures, physiologies, and infectious and non-infectious diseases of invertebrates, and interoperability with standard vocabularies used for plants (Obofoundry 2014). Inadequate funding currently constrains needed enhancements of SNOMED for One Health.
Sequestration of Data
Cultural, legal, and regulatory impediments prompt sequestration of human and non-human disease data, undercutting One Health surveillance. The U.S. Health Insurance Portability and Accountability Act (HIPAA) requires patient information confidentiality. Data requests from public health researchers are often denied based on HIPAA (Illinois Department of Public Health 2009). However, HIPAA actually permits disclosures of protected health information without authorization for specified public health purposes (US Department of Health and Human Services 2003). Additional challenges include private human and veterinary medical laboratories that regard disease data as proprietary, and veterinary diagnostic laboratories that constrain data on diseases, not mandatorily reported to government agencies, to animal owners or veterinarians who submit specimens. Failure to recognize One Health priorities under HIPAA and other privacy protection assertions should be countered through precedent setting under current law or new legislation. To protect patients, owners, and laboratories, data should be anonymized before being transferred to One Health databases.
Territorial Borders
In 1878, formal U.S. surveillance on human infections began identifying nations where endemic diseases or outbreaks were occurring—to deny visas, issue quarantines, and thus prevent infected persons from entering the country (CDC 2013). Such methods are still used, but rapid transit of persons incubating diseases creates potential risks, as noted with the ongoing Ebola outbreak in West Africa (CDC 2015).
Difficulties coordinating health surveillance across local, state, and national borders are partially related to fragmentation of powers under the U.S. Constitution. This is evident in the workings of CDC, which obtains disease data in multiple formats from innumerable health care providers, more than 180,000 public and private laboratories, over 3000 local and 59 state and territorial health departments, and four federal departments [IOM and NRC 2011; U.S. Government Accountability Office (GAO) 2004].
Concerns regarding economic losses in animal agriculture triggered the international surveillance efforts that enabled North American eradications of foot-and-mouth disease, classic swine fever, and screwworms, as well as global eradication of rinderpest. By contrast, present day surveillance for diseases of animals is impaired by fears of economic losses related to embargoes at state/province and national borders (Belant and Deese 2010; IOM 2007). With this need in mind, World Bank (2012) recently showcased benefits of transparency and efficiency of cross-border collaborations in surveillance and control of animal diseases using case studies from Chad to Kyrgyzstan. Cost savings came through cross-border sharing of paraprofessional veterinary front-line staffing; border control, abattoir and market inspection expertise; diagnostic laboratories; and hygiene, quarantine, and vaccination campaigns. Additional benefits included improved epidemiologic tools, more efficient diagnoses of animal diseases, and reduced risks to human health.
Examples of One Health Surveillance Efforts by Governments, International Bodies, Non-governmental Organizations, and Universities
Merging US Confirmations of High-Risk Diseases: How International Standards Have Triggered Data Sharing
CDC’s National Notifiable Diseases Surveillance System (NNDSS) collects and publishes data on approximately 65 reportable human diseases. The disease list is periodically revised considering both incidence and emergence (NNDSS 2011). Human disease reporting is mandated only at the state level, complicating nationwide comparisons. However, complying with WHO International Health Regulations, all states report diseases associated with Public Health Emergencies of International Concern (PHEIC), such as cholera, plague, and yellow fever.
The National Electronic Disease Surveillance System (NEDSS) was established to increase timeliness, standardization, accuracy, and completeness of reporting by local and state agencies to CDC (GAO 2004). NEDSS accelerates data merging, exchanges, and interpretations on localized and cross-jurisdictional outbreaks. A limitation, however, is that infections continue to spread during the time required for sampling, transport, confirmatory assays, data transfers, and epidemiologic analyses.
Similar to the response to globally mandated reporting of human diseases to PHEIC, world standards have led to uniform state reporting of certain animal diseases. USDA accepts OIE’s designated 119 reportable animal diseases, including 26 “multiple-species” diseases (USDA/FSIS 2012; OIE 2014a). Twelve zoonotic diseases must be reported to both CDC and OIE.
The National Animal Health Reporting System (NAHRS) involves multiple participating states, USDA, U.S. Animal Health Association, and the American Association of Veterinary Laboratory Diagnosticians. State veterinarians submit data to NAHRS on confirmed diseases of international importance in livestock, poultry, and aquaculture species, and monthly reports are sent to USDA for verification and compilation. USDA’s National Veterinary Services Laboratories (NVSL) are central to domestic animal health surveillance. They are the nation’s sole federal reference laboratories for domestic and foreign animal disease diagnostics, and they also serve as international reference laboratories. NVSL provide training, laboratory certification for selected diseases, tests for import and export permits, and diagnostic support for disease control and eradication programs.
The U.S. Federal Emergency Response Network (FERN) integrates data from food-testing laboratories in a nested manner, i.e., at the local, state, and federal levels (FERN 2015). FERN hastens coordinated analysis and response to emergencies related to biological, chemical, or radiological contamination of food. By reducing and preventing further exposures that lead to adverse health impacts, FERN helps restore public confidence in the safety of the food supply.
To hasten recognition of biological and chemical agents potentially used by terrorists, emerging diseases, and other health threats, the CDC, Federal Bureau of Investigation, and Association of Public Health Laboratories created the Laboratory Response Network (LRN). LRN compiles infectious and toxicological data from 126 local, state, federal, and international public health, military, food, environmental, and veterinary laboratories (GAO 2004).
US-Based Syndromic Surveillance Systems: Enabling Earlier Interventions
Less specific than traditional methods, syndromic surveillance systems monitor symptomatic frequency, enabling more timely disease recognition. U.S. public health syndromic surveillance systems include BioSense, Electronic Surveillance System for Early Notification of Community-based Epidemics (ESSENCE), and Real-time Outbreak and Disease Surveillance (RODS) (GAO 2004). To hasten detection of public health threats such as bioterrorism or disease outbreaks, BioSense aggregates data from DOD’s and Veterans Affairs’ medical facilities, national clinical laboratories, and over 10,000 pharmacies; and CDC relays interpretations to state and local public health agencies. DOD’s ESSENCE collects data from hospitals and clinics daily, and a geographic information system identifies spatial clustering of health impacts. Used by state public health officials, RODS automatically collects data from hospital clinics, identifies chief medical complaints, classifies syndromes, and points to outbreaks.
A State Example: Illinois—Innovations in Human Health Surveillance, but Greater Attention to Non-humans Needed
The Illinois Department of Public Health (IDPH) undertakes surveillance for human diseases (IDPH 2009). It monitors influenza, classifying weekly statewide and national incidence from “No Activity” through “Widespread Activity” (IDPH 2012). In-state surveillance for HIV-AIDS complies with CDC’s confidential system. Illinois’ I-NEDSS provides a secure, web-based link among health care providers, laboratories, and health departments for reporting and managing infectious diseases. However, it involves time lags, making responses to surveillance more reactive than proactive (Vaid, A., personal communication 2012). Some larger counties also use ESSENCE, and Illinois plans further statewide syndromic surveillance using BioSense.
INDICATOR is an open-source syndromic surveillance system developed by the University of Illinois’ National Center for Supercomputing Applications, Champaign-Urbana Public Health District, and Carle Hospital (Dixon 2010). It collects anonymized data from schools, hospitals, and clinics, and when its algorithm detects unusual patterns of disease, it sends alerts to team members including the public health district (Dixon 2010). INDICATOR unfortunately lacks access to veterinary diagnostic laboratory data.
Illinois’ domestic animal disease surveillance system is poorly funded. Law requires immediate reporting to Illinois Department of Agriculture (IDOA) of suspected cases of 36 animal diseases (list overlaps OIE’s reportable animal diseases) by owners, veterinarians, or others with knowledge of the disease (Joint Committee on Administrative Rules, 2006). However, mechanisms to ensure compliance are lacking. Laboratory testing focuses on infectious disease surveillance, eradication programs, health certification for competition and export, and microbial contamination and antibiotic residues in animal-derived foods. Most surveillance targets economically important animal agriculture.
Surveillance of wildlife health in Illinois appears to be an even lower priority, triggered by extreme outbreak potential (white-nose syndrome in bats), or threats to economic activity and/or public health (chronic wasting disease in deer, West Nile virus, bovine tuberculosis). For example, to protect its bovine tuberculosis-free status, Illinois tests cervids to prevent importation of Mycobacterium bovis.
In addition to concerns regarding the limited extent of animal health surveillance in the state, our inquiry revealed that Illinois’ Departments of Public Health, Agriculture, and Natural Resources and its Environmental Protection Agency lack working relationships needed for efficient tracking of shared infectious or toxicological diseases among people, domestic animals, and wildlife. To facilitate multi-species surveillance and care, University of Illinois’ Center for One Health Illinois offers training, research funding, and interdisciplinary summits. Nevertheless, Illinois has a great deal more to do if it is to establish an efficient One Health surveillance system.
The Epidemic Intelligence Service: Experiential Training of One Health Professionals
CDC’s Epidemic Intelligence Service (EIS) engages diverse One Health professionals together in 2-year programs of postgraduate service and training in epidemiology. The EIS fellows investigate and work to solve important human, animal, and multi-species health problems. EIS has trained over 228 veterinarians since 1951. Most current EIS trainees have medical, veterinary, or epidemiology degrees, but others have doctoral degrees in biological, environmental, social, behavioral, and nutritional sciences.
One Health Diagnostics and Research: Shared Laboratories and Shared Data
To accommodate One Health needs while lowering costs, Canada unified its infectious disease diagnostic and research laboratory with the Canadian Science Centre for Human and Animal Health (Health Canada 1999). The Centre contains isolation facilities, including the highest level of bio-containment, BSL-4, Canada’s only such facility.
The New Mexico Department of Health Scientific Laboratory is a unified facility that undertakes postmortem examinations and ancillary studies of both humans and animals (New Mexico Department of Health (2015). It provides tests for infectious diseases and chemical contaminants that threaten people, livestock, and wildlife.
The U.S. National Institutes of Health (NIH), National Institute of Allergy and Infectious Diseases, Centers of Excellence for Influenza Research and Surveillance (CEIRS) program has formed an integrated network of multi-disciplinary workers that interlinks surveillance research with research on immunology, viral pathogenesis, and risk factors that contribute to emergence and transmission of influenza viruses (NIAID 2015). The CEIRS program thereby provides information and public health tools to control impacts of epidemic influenza as well as to reduce the probability of future influenza pandemics. All of the collaborating CEIRS centers undertake basic and human health research, and the centers at Emory University and the nearby University of Georgia, the Icahn School of Medicine at Mount Sinai in New York, and St. Jude Children’s Research Hospital in Tennessee undertake surveillance examining a range of animal species as well. The CEIRS data are compiled and analyzed by bioinformatics specialists of Digital Infuzion, a private company in Maryland.
US-Based Wildlife Health Centers
Wildlife health centers that conduct regional, national, and international surveillance, research, and graduate and short-course training include USGS’s National Wildlife Health Center (NWHC), University of Georgia’s Southeastern Cooperative Wildlife Disease Study, and University of California-Davis’s Wildlife Health Center. Each of these groups collaborates with wildlife management agencies, thus observations of animals with abnormal behaviors and/or physical attributes by citizens, wildlife or fisheries managers or biologists trigger studies of habitats and animal specimens, enabling diagnoses of infectious, toxicological, nutritional, traumatic, and multi-factorial disorders. Much of their reporting is publicly available. For example, NWHC’s website links to active disease outbreaks and mortality events.
Species-Based One Health Programs: Humans and Endangered Primates in the Wild
Examples of One Health projects that entail coordinated surveillance and care to improve great ape and human health are Health in Harmony, Gorilla Doctors, and Conservation through Public Health. Such programs target infectious diseases, trauma, genetic, nutritional, and other stressors that impact regional great ape and human populations. Providing health and economic benefits to nearby human communities has repeatedly facilitated conservation of endangered species.
A Continent-Wide One Health Endeavor: The African Union Inter-African Bureau for Animal Resources (AU-IABR)
The AU-IABR has been supported by the European Union, U.S. Agency for International Development (USAID), WHO, FAO, and OIE with the goal of increasing expertise and quality assurance in animal health surveillance and promotion (African Union IBAR 2014). AU-IBAR focuses on domestic animals, wildlife, fisheries, and habitats. Included are national action plans to prevent pandemic influenza, programs for animal identification/traceability, and ways to reduce impacts of climate change on animal health.
Catalytic Bursts in One Health from Non-governmental Organizations
The Wildlife Conservation Society (WCS), which evolved out of the Bronx Zoo in New York has led many efforts to increase stewardship of wildlife, and this includes drawing attention to shared health risks at the wildlife, domestic animal, and human interface (Barrett and Osofsky 2013; Myers et al. 2013). Their Field Veterinary Program and broader conservation programs have consistently supported not only wildlife, but also human health and well-being. This includes work in Washington DC and around the world to develop national and international policies that underlie some of the most important One Health initiatives in the world today. The EcoHealth Alliance participates in capacity-building, One Health surveillance, and research, and moreover it synthesizes findings to bring essential perspectives to students and professional audiences (e.g., Mackenzie et al. 2013; Aguirre et al. 2002, 2012). It supports the journal, EcoHealth, and collaborates with the International Society for Ecology and Health to host international EcoHealth Summits. Both WCS and the EcoHealth Alliance have played central roles in bringing One Health to the forefront of veterinary and human health endeavors. Both of these organizations are contributing to accomplishments of the US Agency for International Development (USAID) described below.
Focusing on species in decline or threatened with extinction, the IUCN works with an array of experts in plant and wildlife population biology, genetics, health, ecology, agriculture, forestry, business, economics, and policy to help identify and implement pragmatic solutions to urgent environmental and developmental challenges (IUCN 2015). IUCN has over 1200 government and non-governmental organization members and nearly 11,000 volunteer experts who work in 160 nations. For 50 years, development and updating IUCN’s Red List of Threatened Species has brought experts from needed disciplines together with local groups whose current and future choices in regard to land, water, and biotic management will influence survival and sustainability of species—positively or negatively. IUCN’s commissions on education and communication, environmental law, ecosystem management, species survival, and protected areas have identified ways to increase appreciation of species at peril and how population recoveries can take place in concert with improved economic and food security of human populations. Its various species survival groups include a range of health specialists.
The US Agency for International Development’s Investments in One Health Surveillance and Stewardship
In 2009, USAID collaborated with CDC and USDA to launch the Emerging Pandemic Threats (EPT) program to expand surveillance for influenza and other emerging zoonoses. EPT, which involves five projects, PREDICT, RESPOND, IDENTIFY, PREVENT, and PREPARE, provides training and outbreak response. EPT has reduced risks from influenza by facilitating diagnoses and culling of infected animals, especially poultry.
Through PREDICT, the University of California-Davis partners with EcoHealth Alliance, WCS, Metabiota Inc., and workers in Latin America, Africa, and Asia (Morse et al. 2012). To avoid pandemics, PREDICT focuses attention on risk factors, including encroachment of humans and domestic animals into wildlife habitats, an active interface between humans and infected animals including wildlife, evidence of previous human infections, adaptation of pathogens to achieve efficient human-to-human transmissibility, and opportunities for rapid international transport. Monitoring relies on multiplex PCRs, microarrays, high-throughput sequencing, and metagenomics in discoveries of known and new pathogens. PREDICT emphasizes understanding human incentive/disincentive systems that promote behaviors favoring zoonotic disease transmission to humans. Its recommendations include health impact assessments before initiating actions that create opportunities for disease transmission, such as wildlife trade for food, exotic pet trade, and introduction of agriculture into areas needed by foraging bats. Essential One Health partners linked through PREDICT include national and local governments, and in-country scientists active in pathogen discovery and outbreak reporting. Of importance in regard to One Health, particularly in light of the recent and ongoing human deaths from Ebola virus (EV) infection in West Africa [which as of January 23, 2015 had caused 8675 deaths in a total of 13,602 laboratory-confirmed human cases (CDC 2015)], is the earlier work of PREDICT-affiliated scientists (Olson et al. 2012). The PREDICT team examined data from a sustained multi-species surveillance program to reveal the vital need to examine animals found dead or dying, especially by local people (18 EV positives of 55), instead of focusing attention on live-captured animals (e.g., only 13 EV positives of 5309). In particular, they stressed the importance of sampling sick and dying non-human primates (e.g., chimpanzees, gorillas, and guenons). In addition, they highlighted the value of examining bats that may be reservoir hosts of the virus. Earlier diagnoses coupled with proactive assistance to develop professional and technical capacity as well as work with communities to gain their compliance with recommendations from health professionals were critically important in stopping the spread of EV in Uganda (Burbridge 2014). While Ebola’s effects on humans in West Africa have been unprecedented since the beginning of the current outbreak in 2014, estimates indicate that, over the past 20 years, the Zaire strain of Ebola has killed approximately one-third of the world’s gorillas and chimpanzees, and these species are impacted by other Ebola strains as well (Ryan and Walsh 2011). Ebola is therefore a critically important disease, not only because of human health impacts, but also because of the need to conserve highly endangered species. A range of workers, including some allied to PREDICT, participate in surveillance as well as health care focused on wild great apes.
RESPOND relies upon collaborations among Development Alternatives, Inc., University of Minnesota, Tufts University, Training and Resources Group, and Ecology and Environment, Inc. RESPOND merges skills in animal and human health assessments of paired U.S. and developing country academic institutions to deliver comprehensive training systems for emerging disease detection and response. Through IDENTIFY, the USAID, WHO, FAO, and OIE use existing grants to strengthen laboratory networks and diagnostic capabilities in “geographic hot spots” for emerging diseases. PREVENT relies on a partnership between the Academy for Educational Development and Global Viral Forecasting, Inc. to build upon USAID’s efforts that improve communications and change behaviors thereby reducing risks of multiple zoonotic diseases including influenza. PREPARE is an International Medical Corps project that provides technical support for simulations, field testing, and refinement of local, regional, and national pandemic preparedness plans. Additional information on these and other One Health programs was provided by NRC (2013) and AVMA (2013).
Disease Mapping Programs: Developing a One Health Sense of Place
Collaborative disease mapping efforts are essential for identifying where, why, and how health threats have impacts as well as in targeting where interventions can be most effective. Disease maps can be compared to maps of human uses of land and water, plant cover, animal distributions and migrations, pollutant sources and transport, climate, and other variables. To capitalize on the strengths of different mapping programs, groups focused on broader surveillance concerns are developing collaborations involving multiple map-related data streams. For example, INDICATOR is exploring the use of IDEXX Laboratories’ United States map of case numbers and relative regional severity of canine illnesses from heartworm, Ehrlichia, Anaplasma, and Lyme disease; disease distribution maps generated from OIE’s World Animal Health Information Database; NWHC’s Recent Mortality Events Map; Wildlife Health Event Reporter from Wildlife Health Monitoring Network, which is a web-based open-source system for modular data entry, storage, analysis, reporting, and exchange; and Healthmap’s display of Global Disease Events.
Additional large-scale networked mapping efforts for health surveillance and control efforts include Canada’s Global Public Health Intelligence Network, CDC’s Global Disease Detection Program, DOD’s Global Emerging Infectious Surveillance and Response System, European Centre for Disease Prevention and Control, ProMed’s reports on HealthMap, WHO’s Global Outbreak Alert and Response Network, and WCS’s Global Avian Influenza Network for Surveillance (Morse et al. 2012). Ensuring that these various mapping systems are interlinked is a vital One Health need.
Unifying Concepts
For One Health surveillance to be truly successful, attention to infectious diseases must increase, and far more must be done to focus on avoidance of poisoning, malnutrition, climate change, exotic species invasions, and declines and extinctions of native species. In addition, to meet short- and long-term needs for human, animal, and plant health, surveillance must provide insights on ways to avoid conventional, chemical, biological, and nuclear wars. In the following section, we offer insights as to how nested One Health surveillance can be established in order to hasten needed multi-species benefits.
Recommendations
Relying on approaches and groups described below, we recommend construction, deployment, and refinement of a transparent system of nested One Health surveillance. To serve underserved populations and overcome divisions related to professional divisions, incompatible vocabularies, data sequestration, and territorial borders, collaborating groups of professionals should provide continuously updated reports on short- and long-term problems, threats, and countermeasures. Such reports should focus on specific watersheds, ecosystems, continents, oceans, and the Earth as a whole. Integration of surveillance should reveal trends toward or away from essential outcomes. Surveillance should enable risk assessments pertaining to available options, including continuing or abandoning present management, offering new biomedical interventions, and undertaking conservation activities and ecological rehabilitations. Citizens, NGOs, private enterprises, universities, religious groups, foundations, and governments should provide manpower and funding for needed efforts and products.
Actions to Optimize One Health Surveillance
-
1.
Unify vocabularies Unified vocabularies are essential for merged analyses of organisms and ecosystems of interest (e.g., humans, primates, ungulates, fishes, forests, coral reefs); proximate etiologic agents (e.g., pathogens, predation by exotic invasive species, malnutrition, toxicants, excess CO2 and methane, trauma); manifestations (e.g., lung lesions, cancers, stunting, infertility, immunosuppression, heat stress, death); high-risk circumstances to be avoided/mitigated (e.g., crowded slums, habitat fragmentation, unregulated industries, warfare); societal drivers (e.g., ignorance, bigotry, political corruption, profitability of destructive practices); and countermeasures (e.g., drugs, vaccines, improved diets, pollution controls, ecological rehabilitations, legal and ethical reforms). CDC, USDA, OIE, EPA, UNEP, and other agencies should delegate and empower motivated representatives to streamline and expand SNOMED for unified listing of organisms and ecosystems of interest, reportable etiologies, and manifestations within 1 year. Within 2 years, the representatives should add lists of high-risk circumstances, societal drivers, and countermeasures. Within 4 years, they should link such systems with vocabularies for diseases and other threats to plants. These systems should be open to continuous additions and refinements.
-
2.
Establish mandated reporting of complex One Health stressors The authority of governmental and international agencies to require reporting of spatial and temporal findings of pathogens and toxicants in people, animals, and the environment should serve as templates for required reporting of data on more species and stressors that impact their health. Reporting obligations should extend to human and animal health care providers; pharmacies; public, private, military, environmental, natural resource, and other laboratories engaged in health and environmental assessments; and state/provincial, national, and non-governmental organizations that monitor native and exotic animal and plant populations. The expertise and findings of IUCN in gathering data not only on species but also on human interests should be drawn upon and emulated in order to identify pathways by which multiple problems can be solved through unified planning, management, and refinement. Surveillance technologies should allow on-the-fly acquisition and automated uploading of data into nested One Health databases. The greater good of reduced suffering and deaths in human and animal populations justifies mandating anonymized reporting and circumventing excessive privacy protections. Chronically underfunded international agencies, such as WHO, should be generously supported by member nations, foundations, and donors. Because of the need to adjust surveillance efforts to situation-specific needs, funding should not be restricted by excessively prescriptive mandates. International agencies, governments, and universities should contribute funding to surveillance efforts while simultaneously providing training to build professional capacity.
-
3.
Provide accessible laboratory capabilities International bodies, developed and developing nations should work together until all stakeholders in human, animal, and plant health have open access to affordable regional laboratories capable of timely diagnostic assessments of specimens to meet One Health surveillance needs.
-
4.
Establish disease surveillance, disease reporting, and best management practices in animal health care as prerequisites for insurance, indemnity, and trade in animals/animal products Early disease reporting and certified use of best management practices in animal health production should become prerequisites for insurance and indemnity protection, and for marketing of animals and animal products. Specification of best management practices should draw upon updated guidelines for mammals, birds, bees, and aquatic species of the Terrestrial and Aquatic Codes of the International Standards of OIE (2014b).
-
5.
Expand surveillance to underserved communities Governmental and foundation funding should ensure that underserved populations of humans and animals have access to medical and veterinary expertise. Trusted local human health providers and veterinary technicians should be trained, provided supplies, and electronically linked to medical, veterinary, and surveillance professionals. Prioritization on “failed states” and regions of conflict, intense pollution, overharvest of wild species for food, and inefficient agriculture is warranted to identify urgent human, animal, and ecosystem health needs. Individuals living in such places should be trained and deployed in this effort. In areas of developed nations, where physicians and veterinarians are absent or too few, professionals should be deployed in part through educational debt forgiveness programs.
-
6.
Evaluate multiple sources of diagnostic and syndromic data in real-time, using supercomputers when necessary with automated reporting to individuals responsible for health protection Nested units of government, universities, consultancies, and non-governmental organizations should compete for innovations in analyzing data from One Health surveillance (Herrmann et al. 2011). Syndromic and diagnostic confirmation data should be interlinked with ecological conditions, using mapping/spatial analysis programs, to prioritize One Health investigations, planning, and stewardship interventions.
-
7.
Include in One Health surveillance expert assessments of regional drivers, probabilities, impacts, and economic costs of defense preparedness, terrorism, conventional warfare, and nuclear warfare. Ignorance, misunderstanding, mistrust, hatred, disregard, delusions, corruption, destruction, and the economic and ecological devastation of terrorism, conventional and nuclear warfare will persist until citizens recognize shared interests and demand change. Leaders in medical sciences, education, engineering, business, religions, and government—including defense—should insist upon objective, transparent data acquisition and reporting to enable wide understanding of the causes and impacts of war. Risk assessments should compare warfare to options for outreach to struggling people and nations, enforceable arms reduction agreements, and a strong world court coupled with a multi-national police force to remove despots, quell conflicts, and enable reconciliations.
-
8.
Co-train students preparing for careers in human and veterinary medicine, public health, conservation, agriculture, engineering, business, law, military service, international relations, and communications in core components of One Health, and assign One Health responsibilities to interdisciplinary teams of recent graduates Such students should be required to participate in One Health directed problem-solving courses in their final years of undergraduate work and during studies for graduate and professional degrees. New graduates should be assigned to interdisciplinary teams in government agencies and private enterprise, to participate in data gathering, mitigation, and prevention programs, addressing proximate stressors and societal drivers that undermine health and sustainability.
-
9.
Increase public recognition of One Health problems and solutions The public should be given transparent access to data sets and risk assessments on species declines/extinctions, infectious diseases, nutritional and lifestyle diseases, poisoning, climate change, warfare, and more, with links to information on underlying societal drivers, and ways to protect their families, animals, plants, communities, and ecosystems. They should be able to recognize where and when local to global human activities and interactions are forcing death and destruction, a new era with a high plane of One Health, or something in between. Researchers should determine whether the transparent reporting contributes to grassroots, business, and political support for effective One Health stewardship.
A future One Health surveillance system should unify the efficiency of public health, the depth of human medicine, the breadth of veterinary medicine, the expanse of ecology, the practicality of economics, and the wisdom of peacemaking. Straightforward language should be used to tie One Health realities to an assortment of life experiences, education levels, and core values of communities, simply because broad public awareness of devastating phenomena at work and available pathways toward needed One Health outcomes are essential to catalyze progress. Gathering and analysis of nested site-specific data on humans, domestic animals, wildlife, plants, ecosystems, and underlying societal drivers that threaten their well-being could become the foundation that underpins a distinct societal pivot toward improved health and sustainability.
References
African Union-InterAfrican Bureau for Animal Resources (2014) http://www.au-ibar.org/. Accessed March 6, 2014
Aguirre AA, Ostfeld RS, Daszak P (editors) (2012) New Directions in Conservation Medicine, Applied Cases of Ecological Health, New York: Oxford University Press
Aguirre AA, Ostfeld RS, Tabor GA, House C, Pearl MC (editors) (2002) Conservation Medicine: Ecological Health in Practice, New York: Oxford University Press
Ahmed, T, Hossain, M, Sanin, KI (2012) Global burden of maternal and child undernutrition and micronutrient deficiencies. Annals of Nutrition & Metabolism 61, supplement 1:8-17
Alexander JS, Wilson RC, Green WR (2012) A Brief History and Summary of the Effects of River Engineering and Dams on the Mississippi River System and Delta, U.S. Geological Survey Circular 1375
AVMA (2013) One Health—Academic Survey. Appendix E. The Academic Community Bringing One Health to Action. https://www.avma.org/KB/Resources/Reports/Pages/One-Health69.aspx. Accessed April 28, 2013
Barrett MA, Osofsky SA (2013) One health: interdependence of people, other species, and the planet (and online supplement pp 407(e1)–416(e10) at studentconsult.com). In: Jekel’s Epidemiology, Biostatistics, Preventive Medicine, and Public Health (4th ed.), Katz DL, Elmore JG, Wild DMG, Lucan SC (editors), Philadelphia: Elsevier/Saunders, pp 364–377
Beasley, V (2009) ‘One toxicology’, ‘ecosystem health’ and ‘One Health’. Veterinaria Italiana 45:97-110
Beasley, VR (1993) Ecotoxicology and ecosystem health: roles for veterinarians; goals of the Envirovet program. Journal of the American Veterinary Medical Association 203:617-628
Beasley, VR (2011) Pathophysiology and clinical manifestations of mycotoxin and phycotoxin poisonings. Egyptian Journal of Natural Toxins 8:104-133
Beasley VR, Adkesson AM (2012) Wildlife and ecosystem health. In: Ecology and Animal Health, Ecosystem Health and Sustainable Agriculture 2, Norrgren L, Levengood J (editors), The Baltic University Programme, Uppsala University, pp 13–26. http://www.balticuniv.uu.se/index.php/component/content/article/249-teaching-materials/692-ehsa-book-2-ecology-and-animal-health. Accessed January 29, 2014
Belant, JL, Deese, AR (2010) Importance of wildlife disease surveillance. Human-Wildlife Interactions 4 (2): 165-169
Brandt, AM, Gardner, M (2000) Antagonism and accommodation: interpreting the relationship between public health and medicine in the United States during the 20th century. American Journal of Public Health 90:707-715
Burbridge J (2014) West Africa Ebola outbreak highlights need for PREDICT program. http://gorilladoctorsblog.org/field-blog/2014/8/22/west-africa-ebola-outbreak-highlights-need-for-predict-progr.html. Accessed December 6, 2014
Burgos, S, Slingenbergh, J (2011) Thoughts on human-animal-ecosystems interface. Transboundary and Emerging Disease 58:372-373
Carls, MG, Rice, SD, Hose, JE. (1999) Sensitivity of fish embryos to weathered crude oil: Part 1. Low-level exposure during incubation causes malformations, genetic damage, and mortality in larval Pacific herring (Clupea pallasi) Environmental Toxicology and Chemistry 18:481-493
CDC (2010) Operationalizing “One Health”: A Policy Perspective—Taking Stock and Shaping an Implementation Roadmap, Meeting Overview. http://www.oie.int/fileadmin/Home/eng/Media_Center/docs/pdf/meeting-overview.pdf. Accessed February 15, 2014
CDC (2013) Division of Health Informatics and Surveillance. National Notifiable Disease Surveillance System. Disease Surveillance Search. http://wwwn.cdc.gov/NNDSS/script/SearchResults.aspx?Searchfor=. Accessed January 29, 2014
CDC (2014) West Nile virus disease cases and deaths reported to CDC by year and clinical presentation, 1999–2012. http://www.cdc.gov/westnile/resources/pdfs/cummulative/99_2012_CasesAndDeathsClinicalPresentationHumanCases.pdf. Accessed January 18, 2014
CDC (2015) 2014 Ebola Outbreak in West Africa—Case Counts. http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html. Accessed: January 25, 2015
Chivian, E, Bernstein, A (2008) Sustaining Life, How Human Health Depends on Biodiversity. New York: Oxford University Press
Conrad, PA, Mazet, JA, Clifford, D, Scott, C, Wilkes, M (2009) Evolution of a transdisciplinary ‘‘One Medicine–One Health’’ approach to global health education at the University of California, Davis. Preventive Veterinary Medicine 92:268-274
Costanza, R, d’Arge, R, de Groot, R, Farberk, S, Grasso, M, Hannon, B, Limburg, K, Naeem, S, O’Neill, RV, Paruelo, J, Raskin, RG, Sutton, P, van den Belt, M (1997) The value of the world’s ecosystem services and natural capital. Nature 387:253-260
Costanza, R, de Groot, R, Sutton, P, van der Ploeg, S, Anderson, SJ, Kubiszewski, I, Farber, S, Turner, RK (2014) Changes in the global value of ecosystem services. Global Environmental Change 26:152-158
Coulter, NA (1992) Militarism: a psychosocial disease. Medicine and War 8:7-17
deSwart, RL, Ross, PS, Vos, JG, Osterhaus, ADME (1996) Impaired immunity in harbour seals (Phoca vitulina) fed environmentally contaminated herring. Veterinary Quarterly 18:S127-S128
Di Prisco, G, Cavaliere, V, Annoscia D, Varricchio P, Caprio, E, Nazzi, F, Gargiulo, G, Pennacchio, F (2013) Neonicotinoid clothianidin adversely affects insect immunity and promotes replication of a viral pathogen in honey bees. Proceedings of the National Academy of Sciences 110:18466-18471
Dixon V (2010) Early warning system for illness outbreaks. http://archive-edu.com/page/611785/2012-11-09/http://www.ncsa.illinois.edu/News/Stories/indicator/. Accessed July 9, 2013
Federal Emergency Response Network (FERN) (2015) https://www.fernlab.org. Accessed February 16, 2015
Food and Agriculture Organization of the United Nations (FAO), World Health Organization (WHO), and World Organisation for Animal Health (OIE) (2004) Report of the WHO/FAO/OIE joint consultation on emerging zoonotic diseases. http://whqlibdoc.who.int/hq/2004/who_cds_cpe_zfk_2004.9.pdf. Accessed February 2, 2012
Friend, M (2006) Disease Emergence and Resurgence: The Wildlife-Human Connection. Reston, Virginia: U.S. Geological Survey. Circular 1285. http://www.nwhc.usgs.gov/publications/disease_emergence/. Accessed April 15, 2012
Gibb, H, O’Leary, KG (2014) Mercury exposure and health impacts among individuals in the artisanal and small-scale gold mining community: a comprehensive review. Environmental Health Perspectives 122:667-672
Gopalakrishnan G (2013) World Health Partners, Making Markets Work for the Poor. http://www.skollfoundation.org/entrepreneur/gopi-gopalakrishnan/?utm_source=Skoll+World+Forum+Email+List&utm_campaign=23daf07f27-Skoll_World_Forum_Online_1_Test_Email3_5_2013&utm_medium=email. Accessed March 7, 2013
Greener M (2008) First do no harm. Improving drug safety through legislation and independent research. Embo Reports 9:221-224
Harada, M (1995) Minamata disease: methylmercury poisoning in Japan caused by environmental pollution. Critical Reviews in Toxicology 25:1-24
Health Canada (1999) News Release: Canada opens first facility in the world combining human and animal research. http://www.collectionscanada.gc.ca/archivesweb/20071213074113/http://www.hc-sc.gc.ca/ahc-asc/media/nr-cp/1999/1999_81_e.html. Accessed January 31, 2014
Herrera-Dueñas A, Pineda J, Antonio MT, Aguirre JI (2014) Oxidative stress of House Sparrow as bioindicator of urban pollution. Ecological Indicators 42:6-9
Herrmann JA (2012) Agricultural terrorism—the US perspective. In: Ecology and Animal Health Ecosystem Health and Sustainable Agriculture 2, Norrgren L, Levengood J (editors), The Baltic University Programme, Uppsala University, pp 296–305. http://www.balticuniv.uu.se/index.php/component/content/article/249-teaching-materials/692-ehsa-book-2-ecology-and-animal-health. Accessed January 21, 2014
Herrmann, JA, Kostiuk, SL, Dworkin, MD, Johnson, YJ (2011) Temporal and spatial distribution of blastomycosis cases among humans and dogs in Illinois (2001-2007). Journal of the American Veterinary Medical Association 239:335-343
Hill WA, Petty GC, Erwin PC, Souza MJ (2012) A survey of Tennessee veterinarian and physician attitudes, knowledge, and practices regarding zoonoses prevention among animal owners with HIV infection or AIDS. Journal of the American Veterinary Medical Association 240:1432–1440
Horton, R (2012) GBD 2010: understanding disease, injury, and risk. Lancet 380:2053-2054
Illinois Department of Public Health (2009) Illinois-National Electronic Disease Surveillance System (I-NEDSS). NASCIO Recognition Award Submission. http://www.nascio.org/awards/nominations/2009/2009IL1-State%20of%20IL%20NASCIO%202009%20I-NEDSS.pdf. Accessed February 25, 2014
Illinois Department of Public Health (2012) Seasonal Influenza. 2011–2012 Flu Activity Report. http://www.idph.state.il.us/flu/fluupdate11-12.htm. Accessed May 10, 2012
Institute of Medicine (2007) Global infectious disease surveillance and detection: assessing the challenges—finding solutions. Workshop summary. Washington, DC: The National Academies Press. http://www.ncbi.nlm.nih.gov/books/NBK52867/pdf/TOC.pdf. Accessed March 8, 2012
Institute of Medicine and National Research Council (2011) BioWatch and Public Health Surveillance: Evaluating Systems for the Early Detection of Biological Threats. Abbreviated Version, Washington, DC: The National Academies Press
IUCN (2015) IUCN, International Union for the Conservation of Nature, helps the world find pragmatic solutions to our most pressing environmental and development challenges. http://www.iucn.org. Accessed January 26, 2015
Joint Committee on Administrative Rules. Administrative Code (2006) Title 8: Agriculture and Animals. Chapter I: Department of Agriculture. Subchapter b: Animals and Animal Products (Except Meat and Poultry Inspection Act Regulations). Part 85 Diseased Animals. Section 85.10 Reportable Diseases. Amended at 30 Ill. Reg. 16582, effective October 9, 2006. http://www.ilga.gov/commission/jcar/admincode/008/008000850000100R.html. Accessed May 10, 2012
Jones, KE, Patel, NG, Levy, MA, Storeygard, A, Balk, D, Gittleman, JL, Daszak, P (2008) Global trends in emerging infectious diseases. Nature 451(7181) pp. 990–999
Klauder, JV (1958) Interrelations of human and veterinary medicine — discussion of some aspects of comparative dermatology. New England Journal of Medicine 1258:170-177
Levengood, JM, Beasley, VR (2012) Ecotoxicology, In Conservation Medicine: Applied Cases of Ecological Health. Aguirre, AA, Ostfeld, RS, Daszak, P [eds.] pp. 345-358. Oxford University Press. New York, NY.
Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Barker-Collo S, Bartels DH, Bell ML, Benjamin EJ, Bennett D, Bhalla K, Bikbov B, Bin Abdulhak A, Birbeck G, Blyth F, Bolliger I, Boufous S, Bucello C, Burch M, Burney P, Carapetis J, Chen H, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahodwala N, De Leo D, Degenhardt L, Delossantos A, Denenberg J, Des Jarlais DC, Dharmaratne SD, Dorsey ER, Driscoll T, Duber H, Ebel B, Erwin PJ, Espindola P, Ezzati M, Feigin V, Flaxman AD, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabriel SE, Gakidou E, Gaspari F, Gillum RF, Gonzalez-Medina D, Halasa YA, Haring D, Harrison JE, Havmoeller R, Hay RJ, Hoen B, Hotez PJ, Hoy D, Jacobsen KH, James SL, Jasrasaria R, Jayaraman S, Johns N, Karthikeyan G, Kassebaum N, Keren A, Khoo JP, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lipnick M, Lipshultz SE, Ohno SL, Mabweijano J, MacIntyre MF, Mallinger L, March L, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGrath J, Mensah GA, Merriman TR, Michaud C, Miller M, Miller TR, Mock C, Mocumbi AO, Mokdad AA, Moran A, Mulholland K, Nair MN, Naldi L, Narayan KM, Nasseri K, Norman P, O’Donnell M, Omer SB, Ortblad K, Osborne R, Ozgediz D, Pahari B, Pandian JD, Rivero AP, Padilla RP, Perez-Ruiz F, Perico N, Phillips D, Pierce K, Pope CA 3rd, Porrini E, Pourmalek F, Raju M, Ranganathan D, Rehm JT, Rein DB, Remuzzi G, Rivara FP, Roberts T, De León FR, Rosenfeld LC, Rushton L, Sacco RL, Salomon JA, Sampson U, Sanman E, Schwebel DC, Segui-Gomez M, Shepard DS, Singh D, Singleton J, Sliwa K, Smith E, Steer A, Taylor JA, Thomas B, Tleyjeh IM, Towbin JA, Truelsen T, Undurraga EA, Venketasubramanian N, Vijayakumar L, Vos T, Wagner GR, Wang M, Wang W, Watt K, Weinstock MA, Weintraub R, Wilkinson JD, Woolf AD, Wulf S, Yeh PH, Yip P, Zabetian A, Zheng ZJ, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2095–2128
Mackenzie JS, Jeggo M, Daszak PS, Richt JA (2013) One Health: The Human-Animal-Environment Interfaces in Emerging Infectious Diseases: The Concept and Examples of a One Health Approach. Springer-Verlag. Heidelberg.
Marsh, Inc. (2008) The Economic and Social Impact of Emerging Infectious Disease: Mitigation through Detection, Research, and Response. http://www.healthcare.philips.com/main/shared/assets/documents/bioshield/ecoandsocialimpactofemerginginfectiousdisease_111208.pdf. Accessed February 25, 2014
Mörner T, Beasley V (2012) Monitoring for diseases in wildlife populations. In: Ecology and Animal Health, Ecosystem Health and Sustainable Agriculture 2, Norrgren L, Levengood J (editors), The Baltic University Programme, Uppsala University, pp 186–190. http://www.balticuniv.uu.se/index.php/component/content/article/249-teaching-materials/692-ehsa-book-2-ecology-and-animal-health. Accessed February 25, 2014
Morse, SS, Mazet, JAK, Woolhouse, M, Parrish, CR, Carroll, D, Karesh, WB, Zambraina-Torrelio, C, Lipkin, WI, Daszak P (2012) Zoonosis 3, Prediction and prevention of the next pandemic zoonosis. Lancet 380:1956-1965
Murphy, CM (2012). Writing an effective review article. Journal of Medical Toxicology 8:89-90.
Myers, SS, Gafikin, L, Golden, CD, Ostfeld, RS, Redford, KH, Rickets, TH, Turner, WR, Osofsky, SA (2013) Human health impacts of ecosystem alteration Proceedings of the National Academy of Sciences 110:18753-18760.
National Institute of Allergy and Infectious Diseases (2015) Centers of Excellence for Influenza Research and Surveillance (CEIRS). http://www.niaid.nih.gov/labsandresources/resources/ceirs/Pages/default.aspx. Accessed February 16, 2015
National Notifiable Diseases Surveillance System (2011) http://www.cdc.gov/osels/ph_surveillance/nndss/nndsshis.htm. Accessed January 25, 2012
National Research Council (2013) Workforce Needs in Veterinary Medicine. Washington, DC: The National Academies Press. http://www.nap.edu/catalog.php?record_id=13413. Accessed February 25, 2014
Natterson-Horowitz, B, Bowers, K (2013) Zoobiquity, the Astonishing Connection between Human and Animal Health. Random House, New York, New York.
New Mexico Department of Health (2015) Scientific Laboratory Division. http://nmhealth.org/about/sld/. Accessed February 16, 2015
Nielsen, NO, Waltner-Toews, D, Nishi, JS, Hunter DB (2012). Whither ecosystem health and ecological medicine in veterinary medicine and education. Canadian Veterinary Journal 53:747-753
Norrgren L, Levengood J (editors) (2012) Ecology and Animal Health, Ecosystem Health and Sustainable Agriculture 2. The Baltic University Programme, Uppsala University. http://www.balticuniv.uu.se/index.php/component/content/article/249-teaching-materials/692-ehsa-book-2-ecology-and-animal-health. Accessed February 25, 2014
Obofoundry (2014) The Open Biological and Biomedical Ontologies. http://www.obofoundry.org/. Accessed February 15, 2014
OECD (2014) The Cost of Air Pollution: Health Impacts of Road Transport, OECD Publishing. DOI:10.1787/9789264210448-en. Accessed January 23, 2015
OIE (2014a) Animal Health in the World, OIE-Listed diseases 2014. http://www.oie.int/animal-health-in-the-world/oie-listed-diseases-2012/. Accessed February 25, 2014
OIE (2014b) International Standards. http://www.oie.int/international-standard-setting/overview/. Accessed February 15, 2014
Olson SH, Reed P, Cameron KN, Ssebide BJ, Johnson CK, Morse SS, Karesh WB, Mazet JAK, Joly DO (2012) Dead or alive: animal sampling during Ebola hemorrhagic fever outbreaks in humans. Emerging Threats Journal 5:91340. DOI:10.3402/ehtj.v5i0.9134. http://www.eht-journal.net/index.php/ehtj/article/view/9134/21951. Accessed December 6, 2014
One Health Initiative (2014) One Health Initiative will unite human and veterinary medicine. http://www.onehealthinitiative.com/. Accessed February 7, 2014
Patz J, Githeko AK, McCarty JP, Hussein S, Confalonieri U, de Wet N (2003) Climate change and infectious diseases. In: Climate Change and Human Health–Risks and Responses, McMichael AJ, Campbell-Lendrum DH, Corvalán CF, Ebi KL, Githeko A, Scheraga JD, Woodward A (editors), World Health Organization, pp 103–132. http://www.who.int/globalchange/publications/cchhbook/en/. Accessed February 7, 2014
Quinlan M (2007–8) Abolishing nuclear armouries: policy or pipedream? Survival 49:7–16
Ripple, WJ, Estes, JA, Beschta, RL, Wilmers, CC, Ritchie, EJ, Hebblewhite, M, Berger, J, Elmhagen, B, Letnic, M, Nelson, MP, Schmitz, OJ, Smith, DW, Wallach, AD, Wirsing AJ (2014) Status and ecological effects of the world’s largest carnivores. Science 343:1241484
Robock A, Toon OB. (2012) Self-assured destruction: The climate impacts of nuclear war. Bulletin of the Atomic Scientists 68:66-74
Rohr, JR, Schotthoefer, AM, Raffel, TR, Carrick, HJ, Halstead, N, Hoverman, JT, Johnson, CM, Johnson, LB, Lieske, C, Piwoni, MD, Schoff, PK, Beasley, VR (2008) Agrochemicals increase trematode infections in a declining amphibian species. Nature 455:1235-1239
Rubin C, Dunham B, Sleeman J (2014) Making one health a reality—crossing bureaucratic boundaries. Microbiology Spectrum 2:OH—0016-2012. DOI:10.1128/microbiolspec.OH-0016-2012
Rudicell RS, Piel AK, Stewart F, Moore DL, Learn GH, Yingying L, Takehisa J, Pintea L, Shaw, GM, Moore, J, Sharp PM, Hahn BH (2011). High prevalence of Simian immunodeficiency virus infection in a community of savannah chimpanzees. Journal of Virology 85:9918-9928
Ryan SJ, Walsh PD (2011) Consequences of non-intervention for infectious disease in African Great Apes. PLoS ONE 6(12): e29030. DOI:10.1371/journal.pone.0029030
Schmidt, CW (2012) Quicksilver & gold, mercury pollution from artisanal and small-scale gold mining. Environmental Health Perspectives 120:A424-A429
Schwabe, CW (1964) Veterinary Medicine and Human Health. Baltimore: Williams and Wilkins
Sleeman, JM (2013) Has the time come for big science in wildlife health? Ecohealth 10:335-338.
Stal M, Hostettler D, Ammann WJ (Eds) (2012) Global Risk Forum, One Health Summit 2012, One Health—One Planet—One Future Risks and Opportunities. http://www.oie.int/doc/ged/D11468.PDF. Accessed February 15, 2014
Turco, RP, Toon, OB, Ackerman, TP, Pollack, JB, Sagan, C., (1984) The climatic effects of nuclear war. Scientific American 251:33-43
UNEP (2011) Decoupling natural resource use and environmental impacts from economic growth. In: A Report of the Working Group on Decoupling to the International Resource Panel, Fischer-Kowalski M, Swilling M, von Weizsäcker EU, Ren Y, Moriguchi Y, Crane W, Krausmann F, Eisenmenger N, Giljum S, Hennicke P, Romero Lankao P, Siriban Manalang A, Sewerin S (editors). http://www.unep.org/resourcepanel/decoupling/files/pdf/Decoupling_Report_English.pdf. Accessed January 21, 2014
United Nations (2014) United Nations Millennium Development Goals. http://www.un.org/millenniumgoals/. Accessed January 20, 2014
United States Government Accountability Office (2004) Emerging Infectious Diseases, Review of State and Federal Disease Surveillance Efforts. Report to the Chairman, Permanent Subcommittee on Investigations, Committee on Governmental Affairs, U.S. Senate. www.gao.gov/new.items/d04877.pdf. Accessed February 25, 2014
USDA/APHIS/Wildlife Services (2008) Zoonotic Diseases in Wildlife Damage Management, Safety Review. http://www.aphis.usda.gov/wildlife_damage/nwrc/Safety_Review/Program%20Safety%20Review.shtml. Accessed January 25, 2014
USDA/FSIS (2012) Reportable and Foreign Animal Diseases. http://www.fsis.usda.gov/wps/wcm/connect/2afa4f5f-e7df-479c-9058-55aecc60d145/PHVt-Reportable___Foreign_Animal_Diseases.pdf?MOD=AJPERES. Accessed February 25, 2012
USDA National Institute of Food and Agriculture (2012) USDA Loan Repayment Awards Help Deliver Veterinarian Services to Underserved Rural Communities. http://www.csrees.usda.gov/newsroom/news/2012news/02011_vmlrp.html. Accessed December 5, 2014.
US Department of Health and Human Services (2003) Office of Civil Rights. OCR HIPAA Privacy: Disclosures For Public Health Activities. 45 Code of Federal Regulations (CFR) 164.512(b)
US Department of Health and Human Services (2014) Health Resources and Services Administration, Loans & Scholarships. http://www.hrsa.gov/loanscholarships/. Accessed December 5, 2014
US National Library of Medicine (2014) Unified Medical Language System (UMLS). https://www.nlm.nih.gov/research/umls/Snomed/snomed_main.html. Accessed February 13, 2014
Vié J-C, Hilton-Taylor C, Stuart SN (editors) (2009) Wildlife in a Changing World—An Analysis of the 2008 IUCN Red List of Threatened Species, Gland: IUCN, p 180
Waltner-Toews, D (1983) An open letter to the World Veterinary Congress against nuclear war. Canadian Veterinary Journal 24:111
World Bank (2012) People, Pathogens and Our Planet, Volume 2: The Economics of One Health. Report number 69145-GLB, Washington DC: The World Bank
Zeliger H (2011) Human Toxicology of Chemical Mixtures (second edition). New York: Elsevier. 574 pp.
Zinsstag J, Schelling E, Waltner-Toews D, Tanner M (2011) From “one medicine” to “one health” and systemic approaches to health and well-being. Preventive Veterinary Medicine 101(304):148-156
Acknowledgments
We thank the Center for One Health Illinois, along with the USDA via CSREES Grant #2009-34283-20087, for funding the assistantship that made the contributions of Nathaniel Uchtmann to this work possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Uchtmann, N., Herrmann, J.A., Hahn, E.C. et al. Barriers to, Efforts in, and Optimization of Integrated One Health Surveillance: A Review and Synthesis. EcoHealth 12, 368–384 (2015). https://doi.org/10.1007/s10393-015-1022-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10393-015-1022-7