Abstract
Aim
This study investigated childhood vaccine hesitancy in two regions with different socioeconomic backgrounds in Kayseri, Turkey.
Subject and methods
The study population consisted of all people over 18 years of age admitted to two family health centers (No 65 and 103) in a city center for any reason.
Results
Participants living in the high socioeconomic status (SES) region had a significantly lower mean rating on the CVHQ (Childhood Vaccine Hesitancy Questionnaire - see below) than those living in the low SES region.
Conclusion
Vaccine hesitancy is the main reason for vaccine refusal. Therefore, authorities should provide adequate and accurate information about the significance of vaccines to raise public awareness
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vaccination is the most effective public health intervention to prevent morbidity and mortality associated with infectious diseases (Alsuwaidi et al. 2020). Vaccines contain weakened or inactive parts of a particular organism (antigen) that triggers an immune response within the body (Ergur 2020). According to the World Health Organization (WHO), vaccination saves 2 to 3 million children each year from deadly diseases. It also estimates that 1.5 million more deaths could be avoided if global vaccination coverage improved (WHO 2019).
In 1980, the WHO launched the smallpox eradication program, which was a turning point in world history. Smallpox was eradicated successfully in many countries. Given the positive effects of vaccination on child health and development, the WHO launched the Expanded Program on Immunization (EPI) in 1974 and started mass vaccination against diphtheria, pertussis, tetanus, tuberculosis, polio, and measles (Özmert 2008). There was a significant decrease in the reported number of measles cases from 257,790 in 1980 to 1.754 in 2000 in the Americas. The number of measles cases also dropped from 851,849 in 1980 to 37,421 in 2000 in Europe (WHO 2020). Turkey launched the EPI in 1981 (Özmert 2008) Having reported its last smallpox case in 1998, Turkey was certified polio-free by the WHO in 2002. The significant reductions in reported cases of diphtheria, pertussis, tetanus, measles, rubella, mumps, and chickenpox and the eradication of smallpox and polio are the ultimate proof of vaccine efficacy (Ergur 2020; Özmert 2008).
Conceptual framework
Despite all the evidence, vaccine hesitancy and vaccine refusal have been global challenges that have posed a significant threat to the acceptance of vaccines and vaccination programs, resulting in a significant reduction in childhood immunization rates worldwide (Dubé et al. 2015). The WHO defines vaccine hesitancy as “the delay in the acceptance or the refusal of vaccines despite their availability.” Vaccine hesitancy is complex and context-specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience, and confidence. People with vaccine hesitancy are a heterogeneous group between those who accept all vaccines and those who reject them all (MacDonald and SAGE Working Group on Vaccine Hesitancy 2015). The WHO established the Strategic Advisory Group of Experts on Immunization (SAGE) to identify the reasons behind the global rise of vaccine hesitancy. SAGE grouped the reasons for vaccine hesitancy under three categories: (1) contextual influences, (2) individual and group influences, and (3) vaccine/vaccination-specific issues. Contextual influences address communication and media environment, influential leaders, gatekeepers and anti- or pro-vaccination lobbies, historical influences, sociodemographic characteristics, politics/policies, geographic barriers, and the pharmaceutical industry. Individual and group influences encompass experience with past vaccination, beliefs, attitudes about health and prevention, knowledge/awareness, trust in the health system and healthcare providers, personal experiences, risk/benefit, and social norms. Vaccine/vaccination specific issues are concerned with risk/benefit (scientific evidence), the introduction of a new vaccine or new formulation, mode of administration, design of vaccination program /mode of delivery, reliability and/or source of vaccine supply, vaccination schedule, costs, and the role of healthcare professionals (MacDonald and SAGE Working Group on Vaccine Hesitancy 2015).
The WHO reported that 23 million children missed out on essential vaccines through routine immunization services in 2020 due to vaccine hesitancy and vaccine refusal, which are among the top ten global health issues (WHO 2019). Bianco et al. (2019) found that a quarter of Italian parents delayed and refused vaccinations for their children (24.6%) (Bianco et al. 2019). Alsuwaidi et al. (2020) reported that the prevalence of vaccine hesitancy among parents in the United Arab Emirates was 36% (Alsuwaidi et al. 2020). Azizi et al. (2017) determined that one in ten parents had childhood vaccine hesitancy (11.6%) (Azizi et al. 2017). Childhood vaccine hesitancy and vaccine refusal have also been a growing problem in Turkey, causing low immunization rates. In 2011, only 183 Turkish parents refused to have their children vaccinated. However, the number increased to 40 thousand in 2019 (Aygün and Tortop 2020). The Turkish Demographic and Health Survey (TNSA 2018) has reported two critical results. First, the rate of fully immunized children has dropped to 67% since 2013. Second, only one in two children 24–35 months of age has been vaccinated according to the immunization schedule (TNSA 2018).
Turkey’s childhood immunization rate is expected to fall below the critical level of 80% in 5 years unless something is done about vaccine hesitancy and vaccine refusal. Experts are concerned that epidemics will reappear, inevitably leading to child deaths that could be prevented by immunization (Nas et al. 2020). We need first to understand vaccine hesitancy and determine how widespread and effective it is to protect and improve public health and combat vaccine refusal. Moreover, if we can identify the causes of vaccine hesitancy, we can help authorities make the right decisions and introduce the right policies to fight vaccine refusal (Bianco et al. 2019; Facciolà et al. 2019).
The scope of the research and its contribution to the literature
The WHO argues that sociodemographic characteristics (age, education, income, health coverage, etc.) are the causes of vaccine hesitancy and vaccine refusal (MacDonald and SAGE Working Group on Vaccine Hesitancy 2015). The social determinants of health are gender (female), place of residence (city vs countryside), low education, low income, unemployment, and health coverage status (Braveman and Gottlieb 2014). Vaccination rates are lower, and vaccine hesitancy or refusal is higher in rural areas than in urban areas. Moreover, people living in rural areas with a low socioeconomic status (SES) are less likely to access immunization services than those living in urban areas (Al-lela et al. 2011; Awadh et al. 2014; Okafor et al. 2015). This study investigated the effect of sociodemographic characteristics (gender, education level, income, health coverage status, etc.) on childhood vaccine hesitancy. Therefore, we focused on two regions with different sociodemographic characteristics. Most research on childhood vaccine hesitancy in Turkey has recruited parents or patients (Güneş 2020; Evran and Bozkurt 2020; Kaydirak et al. 2020). However, there is limited research on childhood vaccine hesitancy in the Turkish public.
Therefore, this study sought answers to two questions: (1) What do people living in two regions with different socioeconomic backgrounds in the city center of Kayseri think about childhood vaccines? and (2) what factors affect childhood vaccine hesitancy? We believe that our results will contribute to the literature and help authorities develop optimal public health strategies to improve overall vaccination coverage.
Methods
Research purpose and type
This descriptive and cross-sectional study aimed to determine what people from two regions with different socioeconomic backgrounds in the city center of Kayseri thought about childhood vaccines and what factors affected their childhood vaccine hesitancy.
Setting, sample, and population
The study population consisted of all people over 18 years of age admitted to two family health centers (No 65 and 103) in the city center of Kayseri, Turkey. Kayseri was the city of choice because no earlier research on community-based childhood vaccine hesitancy has been conducted there. We selected FHC regions based on socioeconomic status. Family Health Center No. 65 is located in a high-SES region close to the city center (Region 1: SES=high). Family Health Center No. 103 is located in a low-SES region far from the city center (Region 2: SES=low). The two regions have similar populations (Region 1: 23,528 persons & Region 2: 21,500 persons). Family Health Center No. 65 has 12 physicians and 12 family healthcare professionals. Family Health Center No. 103 has 13 physicians and 13 family healthcare professionals. A rule of thumb for determining the sample size is recruiting an absolute minimum of ten participants per predictor variable for regression equations with six or more predictor variables. However, researchers recommend recruiting 30 participants per predictor variable for a better representation. Therefore, the target sample consisted of 500 participants [30x15 (number of variables) +50 (in case of missing data)] ( Polit and Beck 2017). We reached 557 people. A multiple regression analysis was performed for analysis. Researchers recommend recruiting 10–20 participants for each independent variable in a multiple regression analysis (Cokluk 2010). The sample was large enough for the multiple regression analysis as well.
Data collection tools
The data were collected using a personal information form and a Childhood Vaccine Hesitancy Questionnaire (Azizi et al. 2017; Bianco et al. 2019; Napolitano et al. 2018).
Personal information form
The personal information form was based on a literature review conducted by the researchers. The form consisted of 15 items on age, gender, marital status, education level, health coverage status, etc.
Childhood vaccine hesitancy questionnaire
The Childhood Vaccine Hesitancy Questionnaire (CVHQ) was developed by the researchers to identify the reasons for childhood vaccine hesitancy (Aygün and Tortop 2020; Azizi et al. 2017; Bianco et al. 2019). The questionnaire consisted of 11 positive and 16 negative items rated on a five-point Likert-type scale (5 = Strongly agree, 4 = Agree, 3 = Undecided, 2 = Disagree, 1 = Strongly Disagree). The negative items are reverse scored. The total score ranges from 27 to 135, with higher scores indicating higher levels of childhood vaccine hesitancy. Five experts with Ph.D. degrees in the department of public medical health and public health nursing checked the questionnaire for relevance and intelligibility. The experts assessed each item's necessity, intelligibility/clarity, and relevance using a four-point rating scale (1 = very relevant, 2 = relevant but needs minor alteration, 3 = in need of revision, 4 = not relevant) (Davis 1992). The content validity index (CVI) was calculated by dividing the total score of each item by the total number of experts. The minimum index value for an item to be valid is greater than 0.80 (Davis 1992). Each item had a CVI of 0.89 to 1.00. Therefore, no items were removed from the questionnaire. A pilot study was conducted with 40 participants over 18 years of age. No modification was made to the items based on the pilot study results. The questionnaire had a Cronbach’s alpha of 0.84 after the pilot study. A general rule of thumb is that robust scientific instruments should have a Cronbach's Alpha of at least 0.70 (Şencan 2005). The questionnaire had a Cronbach’s alpha of 0.87.
Data collection
Participation was voluntary. The data were collected by a pollster in FHCs No 65 and 103 between December 2021 and January 2022. The researchers informed the pollster about the research content, survey questions, and data collection strategy. Data collection lasted 5–6 minutes.
Inclusion and exclusion criteria
The inclusion criteria were (1) admitting to FHCs No 65 and 103 for a reason, (2) volunteering to participate, and (3) being over 18 years of age. Patients who failed to meet these inclusion criteria were excluded.
Research questions, dependent and independent variables, and research hypotheses
The research questions are as follows:
-
1)
What do participants think about childhood vaccination?
-
2)
What factors affect participants’ childhood vaccine hesitancy?
The independent variables were sociodemographic characteristics. The dependent variable was the total CVHQ score. The research hypothesis was as follows:
-
H0: There is no significant difference in the total CVHQ scores between participants from Regions 1 and 2.
-
H1: There is a significant difference in the total CVHQ scores between participants from Regions 1 and 2.
Data analysis
The data were analyzed using the Statistical Package for Social Sciences (SPSS, v 25.0) at a significance level of 0.05. Number, percentage, and mean were used for descriptive data. The chi-square test was used to compare the groups based on sociodemographic and introductory characteristics. The Kolmogorov–Smirnov test was used for normality testing. The results showed that the data were normally distributed. Therefore, parametric tests were used for analysis. An independent groups t-test was used to compare two groups, while one-way analysis of variance (ANOVA) was used to compare more than two groups. A Tukey's test was used for pairwise group comparisons to determine the source of differences. No missing data completion method was used. A multiple regression analysis (enter method) was performed to determine whether participants’ sociodemographic characteristics predicted their vaccine hesitancy. The categorical variables in the model were converted into dummy variables. Table 5 shows the variables coded as zero (0).
Results
Table 1 shows all participants’ sociodemographic and introductory characteristics. More than half the participants were women (64.1%) and married (79%). Less than half the participants had bachelor's degrees (44%). Half the participants had high SES (50.6%). More than half the participants had children or grandchildren younger than 5 years (76.1%). Most participants from Region 1 were women (76.4%), while almost half the participants from Region 2 were men (47.6%). Participants from Region 1 were better educated than those from Region 2. Sixteen participants from Region 1 had extended families (5.9%), whereas 36 participants from Region 2 had extended families (12.6%) (p < 0.05) (Table 1).
Table 2 shows all participants’ views on vaccines and vaccine history. Most participants stated that they knew enough about vaccines (83.7%). More than half the participants noted that they had had a flu shot (68.9%). The majority of the participants remarked that they had their children vaccinated according to the immunization calendar (82.9%). Significantly more participants from Region 1 stated that they knew enough about vaccines than those from Region 2 (p = 0.004) (Table 2).
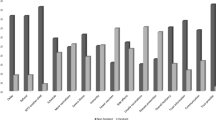
Figure 1 shows all participants’ beliefs in the necessity of childhood vaccines. More than half the participants believed that vaccines were absolutely necessary (69.1%). Less than a quarter of the participants believed that some vaccines were necessary (17.4%). Twelve participants did not believe vaccines were necessary (2.2%). Sixty-three participants had no idea (11.3%).
Table 3 shows the distribution of CVHQ scores by sociodemographic and introductory characteristics. Participants from Region 1 had a significantly lower mean CVHQ score than those from Region 2 (p ≤ 0.001). Female participants had a significantly lower mean CVHQ score than their male counterparts (p = 0.017). Participants with bachelor’s degrees had a significantly lower mean CVHQ score than those with lower degrees (p ≤ 0.001). Married participants had a significantly lower mean CVHQ score than their single counterparts (p = 0.009). Participants with healthcare professional family members had a significantly lower mean CVHQ score than those without healthcare professional family members (p ≤ 0.001). Participants with nuclear families had a significantly lower mean CVHQ score than those with extended or broken families (p = 0.030) (Table 3).
Table 4 shows the distribution of participants’ CVHQ scores by their views on vaccines and vaccination history. Participants who knew enough about vaccines had a significantly lower mean CVHQ score than those who did not (p ≤ 0.001). Participants who had had a flu shot had a significantly lower mean CVHQ score than those who had not (p ≤ 0.001). Participants who had their children vaccinated according to the immunization calendar had a significantly lower mean CVHQ score than those who had not (p ≤ 0.001). Participants who believed vaccines were necessary had a significantly lower mean CVHQ score than those who did not (p ≤ 0.001) (Table 4).
Participants had a mean CVHQ score of 61.4 ± 13.7. A multiple regression analysis (enter method) was performed to determine the effect of the independent variables on the dependent variable. Living in Region 1 (β = 0.079), having a bachelor’s degreβ = (β = 0.235), having a family member as a healthcare professional (β = 0.082), knowing enough about vaccines (β = 0.226), believing that all vaccines are necessary (β = 0.324), and having had a flu shot (β = 0.121) reduced the CVHQ scores by 2.1, 6.4, 2.5, 8.4, 9.6, and 3.6 points respectively. These variables accounted for 60% of the total variance (Table 5).
Discussion
This study investigated the prevalence of vaccine hesitancy among two regions with different socioeconomic backgrounds in Kayseri, Turkey. The sample consisted of 557 participants over 18 years of age admitted to two family health centers (No 65 and 103) in the city center for any reason. The study had two objectives: (1) determining what participants thought about childhood vaccines and (2) identifying the reasons behind vaccine hesitancy. Most participants from Region 1 were women (76.4%), while almost half the participants from Region 2 were men (47.6%). Participants from Region 1 were better educated than those from Region 2. Participants from Region 1 had a better income than those from Region 2. Both regions were similar in terms of health coverage status and the number of children/grandchildren under 5 years of age. According to the TNSA (2018), (1) health coverage is less common in rural areas than in urban areas in Turkey, (2) people living in rural areas have more children than those living in urban areas, (3) people living in urban areas have a higher income and education level than those living in rural areas. Our results showed that Turkey's rural and urban areas were similar in terms of some sociodemographic characteristics, such as education and income. More participants from Region 1 knew enough about vaccines than those from Region 2. This is probably because the former were better educated than the latter.
Gender, marital status, and family type did not affect participants' CVHQ scores. However, region and education affected their CVHQ scores. In other words, participants from Region 1 had a significantly lower mean CVHQ score than those from Region 2. Participants with bachelor’s degrees had a significantly lower mean CVHQ score than those with lower degrees (Table 5). This is probably because participants from Region 1 were better educated than those from Region 2. People with higher education levels are less hesitant to have vaccines because they are more likely to be informed about health, vaccines, and immunization. Azizi et al. (2017) found that younger parents who had no or less experience with childhood vaccination were more vaccine-hesitant (Azizi et al. 2017). However, the researchers did not detect an association between vaccine hesitancy and ethnic background, gender, and family income. Napolitano et al. (2018) determined that age and education were negatively correlated with vaccine hesitancy The differences in the results may be due to cultural differences ( Napolitano et al. 2018).
Participants who believed vaccines were necessary had a significantly lower mean CVHQ score than those who did not (Table 3). Believing that all vaccines were necessary was an important predictor of vaccine hesitancy (Table 5). Vaccines have eradicated many childhood diseases (Salmon et al. 2015). The immunization programs have been so effective that most people, especially young people, have little to no experience with vaccine-preventable diseases. In other words, some people may think that vaccines are unnecessary because vaccine-preventable diseases have been virtually eliminated from the face of the earth (Cella et al. 2020). People living in countries with high vaccination rates may think that herd immunity can be achieved even without them getting vaccinated, or they may think that they do not need to get vaccinated because nothing bad will happen to them or their children. This may affect their opinions about vaccines and vaccine acceptance (Diaz Crescitelli et al. 2020; Facciolà et al. 2019; Salmon et al. 2015). People who think they are at low risk for infectious diseases are more likely to have negative attitudes towards vaccines and refuse to get their children vaccinated. Minimizing perceived vaccine-associated risks is related to the reduced importance of herd immunity (Cella et al. 2020; Diaz Crescitelli et al. 2020). People's views on the importance and necessity of vaccines make them less or more vaccine-hesitant. Therefore, authorities should inform people about the health benefits of vaccines. Healthcare professionals and institutions should collaborate and use print and visual media effectively to raise public awareness of the necessity and importance of vaccines (Larson et al. 2014).
Participants who knew enough about vaccines had a significantly lower mean CVHQ score than those who did not (Table 3). Knowing enough about vaccines was an important predictor of vaccine hesitancy (Table 5). Research also shows that people with sufficient knowledge about vaccines are less likely to be vaccine-hesitant or anti-vaxxers (Facciolà et al. 2019; Sadaf et al. 2013). Participants who knew enough about vaccines were less vaccine-hesitant probably because they knew about vaccines' content, necessity, and safety, vaccine production and patenting, and the impact of vaccines on public health. False information travels faster on social media than fact-checking efforts can keep up. It is critical to access the right information about vaccines (Bianco et al. 2019) because misinformation and the active propaganda of anti-vaccination movements cause an increase in the number of people who deliberately refuse to have vaccinated or have their children vaccinated (Facciolà et al. 2019). People who learn about vaccines from their friends or online platforms (Diaz Crescitelli et al. 2020) and those exposed to anti-vax celebrities, television shows, magazines, and news articles are more likely to turn into either vaccine-hesitant or anti-vaxxers (Siddiqui et al. 2013). Vaccine-hesitancy is more prevalent among people who trust social media platforms more than they trust pediatricians about vaccines (Alsuwaidi et al. 2020). Moreover, the Internet is filled with anti-vax books and advertisements on complementary and alternative medicines, such as hijamat, acupuncture, organic honey, organic product, herbs, etc. (Siddiqui et al. 2013). Given that we live in an information age, authorities should put much more effort into ensuring that the public has access to the right information about vaccines and vaccination programs because people who have the right information about vaccines are more likely to accept them. Healthcare professionals should inform people about vaccines.
Participants who had family members working as healthcare professionals had a significantly lower mean CVHQ score than those who did not (Table 3). Having a family member as a healthcare professional was a significant predictor of vaccine hesitancy (Table 5). All healthcare professionals, especially primary healthcare professionals, are responsible for providing information on childhood immunizations. They also play a key role in people’s decisions about vaccinations (Omer et al. 2009). Research shows that people who trust the information they receive from healthcare professionals about vaccines are more likely to develop positive attitudes towards vaccination (Gualano et al. 2018; Kennedy et al. 2011). Napolitano et al. (2018) determined that vaccine hesitancy was less common among parents working as healthcare professionals. Therefore, healthcare professionals are responsible for informing the public, especially parents, about the health benefits of vaccines (Napolitano et al. 2018). Vaccine hesitancy is less common among people who are informed by healthcare professionals (Charron et al. 2020). Vaccine hesitancy was less common among our participants who had family members working as healthcare professionals. This is probably because those participants are in communication with their healthcare professional family members, asking them questions about vaccines and vaccination programs, and therefore, they have the chance to get direct information about issues surrounding vaccines. Healthcare professionals should inform people about childhood vaccinations, answer their questions based on scientific evidence, and receive feedback (Alsuwaidi et al. 2020). Moreover, healthcare professionals should keep pace with advances in vaccine technology and be open to communication in order to reduce the prevalence of childhood vaccine hesitancy (Alsuwaidi et al. 2020; Gualano et al. 2018; Yorulmaz and Karadeniz 2022).
Participants who had flu shots had a significantly lower mean CVHQ score than those who did not (Table 3). Having a flu shot was a significant predictor of vaccine hesitancy (Table 5). Seasonal flu is a global health problem responsible for thousands of deaths and billions of dollars of economic loss. Flu shots reduce the burden of disease, work and economic losses, and deaths. Expanding flu vaccine coverage is a global goal (Nyhan and Reifler 2015). High hesitancy to both general vaccines and flu shots is associated with low rates of flu shot coverage (Quinn et al. 2019). People who refuse to get flu shots always have more negative attitudes toward vaccines and are more suspicious about the accuracy of the information they receive from healthcare professionals (Gorman et al. 2020). People with low vaccine hesitancy are more likely to trust vaccines and get their flu shots. Authorities should inform people about vaccines to persuade them to get flu shots. Informing people about vaccines can also encourage them to get vaccines not included in the national immunization program (influenza, rotavirus, meningococcus, et.), resulting in reduced disease burden and economic losses.
More than half the participants believed that vaccines were absolutely necessary (69.1%). Less than a quarter of the participants believed that some vaccines were necessary (17.4%). Twelve participants believed vaccines were unnecessary (2.2%). Sixty-three participants had no idea (11.3%) (Fig. 1), suggesting that three in ten participants are at high risk of vaccine hesitancy and refusal. People who do not believe vaccines are necessary are more likely to refuse to get vaccinated. Epidemics may break out again (mumps, measles, etc.) if herd immunity drops below 90–95% (Lee et al. 2016), which is quite disconcerting. Therefore, authorities should inform people with vaccine hesitancy about the health benefits of vaccines in order to reduce the prevalence of vaccine hesitancy and vaccine refusal and to protect and improve public health (MacDonald and SAGE Working Group on Vaccine Hesitancy 2015; Marshall et al. 2018).
Our results indicated that the prevalence of childhood vaccine hesitancy varied from region to region, rejecting Hypothesis H0. Living in a high-SES region, having a bachelor’s degree, having a family member as a healthcare professional, knowing enough about vaccines, believing all vaccines are necessary, and having had a flu shot affected participants' CVHQ scores. Believing all vaccines are necessary, knowing enough about vaccines, and having a bachelor’s degree reduced the CVHQ scores by 9.6, 8.4, and 6.4 points respectively. Authorities should inform the public about vaccines to prevent childhood vaccine hesitancy and vaccine refusal and protect and improve public health. Therefore, healthcare professionals and educators should address the topics of the content of vaccines, the safety of vaccines, the importance and effectiveness of vaccines, the effect of vaccines on the course of infectious diseases, the discovery of vaccines, and the course of childhood infectious diseases from past to present (Larson et al. 2014).
Study limitations
This study had four limitations. First, the sample was recruited only from two FHCs in the city center of Kayseri, Turkey. Second, the results may not fully reflect the thoughts of people who are hesitant about childhood vaccinations and think that childhood vaccinations are unnecessary because anti-vaxxers probably do not seek healthcare services or would not want to participate in the study. Third, people might have been admitted to the FHCs only for emergencies due to the COVID-19 pandemic. Fourth, the results are sample-specific and cannot be generalized to the whole population.
Conclusion
This study had two objectives: (1) focusing on what people from two socioeconomically different regions of Kayseri, Turkey, thought about childhood vaccines and (2) determining the prevalence of vaccine hesitancy. The results showed that participants were moderately hesitant about childhood vaccines (mean: 61.4 ± 13.7, min: 27, max: 135). Most participants believed that childhood vaccines were necessary and knew enough about them. Believing that all vaccines are necessary, knowing enough about vaccines, having a bachelor’s degree, having a family member working as a healthcare professional, and having had a flu shot significantly reduced childhood vaccine hesitancy.
Our results are consistent with earlier research and contribute to the literature. Authorities should provide people with community-based education and information programs to prevent vaccine hesitancy and vaccine refusal. Healthcare professionals should inform people more about vaccines' effectiveness and health benefits. The Turkish Ministry of Health should use mass media and public service announcements to raise public awareness of vaccination programs. Further research should address the effect of community-based education and information programs on preventing vaccine hesitancy and vaccine refusal.
Change history
16 April 2024
A Correction to this paper has been published: https://doi.org/10.1007/s10389-024-02267-2
References
Abd Halim H, Abdul-Razak S, Yasin M, Isa MR (2020) Validation study of the Parent Attitudes About Childhood Vaccines (PACV) questionnaire: the Malay version. Human Vaccines Immunotherapeut 16(5):1040–1049. https://doi.org/10.1080/21645515.2019.1674112
Al-lela OQB, Bahari MB, Al-abbassi MG, Basher AY (2011) Development of a questionnaire on knowledge, attitude and practice about immunization among Iraqi parents. J Public Health 19:497–503. https://doi.org/10.1007/s10389-011-0411-9
Alsuwaidi AR, Elbarazi I, Al-Hamad S, Aldhaheri R, Sheek-Hussein M, Narchi H (2020) Vaccine hesitancy and its determinants among Arab parents: a cross-sectional survey in the United Arab Emirates. Human Vaccines Immunotherapeut 16(12):3163–3169. https://doi.org/10.1080/21645515.2020.1753439
Awadh AI, Hassali MA, Al-lela OQ, Bux SH, Elkalmi RM, Hadi H (2014) Immunization knowledge and practice among Malaysian parents: a questionnaire development and pilot-testing. BMC Public Health 14:1107. https://doi.org/10.1186/1471-2458-14-1107
Aygün E, Tortop HS (2020) Investigation of parents' vaccine hesitation levels and reasons of vaccine refusal. J Current Pediat 18(3):300–316
Azizi FSM, Kew Y, Moy FM (2017) Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine 35(22):2955–2961. https://doi.org/10.1016/j.vaccine.2017.04.010
Bianco A, Mascaro V, Zucco R, Pavia M (2019) Parent perspectives on childhood vaccination: how to deal with vaccine hesitancy and refusal? Vaccine 37(7):984–990. https://doi.org/10.1016/j.vaccine.2018.12.062
Braveman P, Gottlieb L (2014) The social determinants of health: it's time to consider the causes of the causes. Public Health Rep Suppl 2(Suppl 2):19–31. https://doi.org/10.1177/2F00333549141291S206
Cella P, Voglino G, Barberis I et al (2020) Resources for assessing parents’ vaccine hesitancy: A systematic review of the literature. J Prevent Med Hygiene 61(3):340–373. https://doi.org/10.15167/2F2421-4248%2Fjpmh2020.61.3.1448
Charron J, Gautier A, Jestin C (2020) Influence of information sources on vaccine hesitancy and practices. Med Mal Infect 50(8):727–733. https://doi.org/10.1016/j.medmal.2020.01.010
Cokluk O (2010) Logistic regression: concept and application. educational sciences. Theory Pract 10(3):1397–1407
Davis LL (1992) Instrument review: getting the most from a panel of experts. Appl Nurs Res 5:194–197. https://doi.org/10.1016/S0897-1897(05)80008-4
Diaz Crescitelli ME, Ghirotto L, Sisson H et al (2020) A meta-synthesis study of the key elements involved in childhood vaccine hesitancy. Public Health 180:38–45. https://doi.org/10.1016/j.puhe.2019.10.027
Dubé E, Vivion M, MacDonald NE (2015) Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: influence, impact and implications. Expert Rev Vaccines 14(1):99–117
Ergur A (2020) Social causes of vaccine rejection–vaccine indecision attitudes in the context of criticisms of modernity. Eurasian J Med 52(2):217–223. https://doi.org/10.5152/2Feurasianjmed.2020.20132
Evran M, Bozkurt HB (2020) Knowledge status and affecting factors about the current childhood vaccines of mothers of children applying to state and university hospital pediatric clinics in Kars. Kafkas J Med Sci 10(3):173–179. https://doi.org/10.5505/kjms.2020.93206
Facciolà A, Visalli G, Orlando A et al (2019) Vaccine hesitancy: an overview on parents’ opinions about vaccination and possible reasons of vaccine refusal. J Public Health Res 8(1):1436. https://doi.org/10.4081/2Fjphr.2019.1436
Gorman DR, Bielecki K, Larson HJ et al (2020) Comparing vaccination hesitancy in Polish migrant parents who accept or refuse nasal flu vaccination for their children. Vaccine 38(13):2795–2799. https://doi.org/10.1016/j.vaccine.2020.02.028
Gualano MR, Bert F, Voglino G et al (2018) Attitudes towards compulsory vaccination in Italy: results from the NAVIDAD multicentre study. Vaccine 36(23):3368–3374. https://doi.org/10.1016/j.vaccine.2018.04.029
Güneş NA (2020) Vaccine hesitations and families' perspectives on vaccine refusal in Western Turkey. J Pediatr Nurs 53:186–194
Kaydirak MM, Gumusay M, Gulec Y, Sahin NH (2020) Parental opinions and approaches about childhood vaccinations: are anti-vaccination approaches and indecisiveness parental rights? J Community Health Nurs 37(4):222–232
Kennedy A, Basket M, Sheedy K (2011) Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey. Pediatrics 127(Suppl 1):92–99. https://doi.org/10.1542/peds.2010-1722N
Larson HJ, Jarrett C, Eckersberger E et al (2014) Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine 32(19):2150–2159. https://doi.org/10.1016/j.vaccine.2014.01.081
Lee C, Whetten K, Omer S et al (2016) Hurdles to herd immunity: distrust of government and vaccine refusal in the US, 2002–2003. Vaccine 34(34):3972–3978. https://doi.org/10.1016/j.vaccine.2016.06.048
MacDonald NE, SAGE Working Group on Vaccine Hesitancy (2015) Vaccine hesitancy: definition, scope and determinants. Vaccine 33:4161–4164. https://doi.org/10.1016/j.vaccine.2015.04.036
Marshall HS, McMillan M, Koehler A et al (2018) B Part of It protocol: a cluster randomised controlled trial to assess the impact of 4CMenB vaccine on pharyngeal carriage of Neisseria meningitidis in adolescents. BMJ Open 8(7):e020988. https://doi.org/10.1136/bmjopen-2017-020988
Napolitano F, D’Alessandro A, Angelillo IF (2018) Investigating Italian parents’ vaccine hesitancy: a cross-sectional survey. Human Vaccines Immunotherapeut 14(7):1558–1565. https://doi.org/10.1080/21645515.2018.1463943
Nas MA, Atabay G, Şakiroğlu F, Cayir Y (2020) Vaccine rejection in a university’s training family health centers. Konuralp Med J 12(3):430–434. https://doi.org/10.18521/ktd.744687
Nyhan B, Reifler J (2015) Does correcting myths about the flu vaccine work? An experimental evaluation of the effects of corrective information. Vaccine 33(3):459–464
Okafor C, Hu X, Cook RL (2015) Racial/ethnic disparities in HPV vaccine uptake among a sample of college women. J Racial Ethn Health Disparities 2:311–316. https://doi.org/10.1007/s40615-014-0074-7
Omer SB, Salmon DA, Orenstein WA et al (2009) Vaccine refusal, mandatory immunization, and the risks of vaccine-preventable diseases. N Engl J Med 360:1981–1988. https://doi.org/10.1056/NEJMsa0806477
Özmert EN (2008) Progress in the national immunization practices in the world and in Turkey. J Child Health Diseases 51(3):168–175
Polit DF, Beck CT (2017) Nursing research: generating and assessing evidence for nursing practice (10th ed.). Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia, 784 pp. https://doi.org/10.1016/j.iccn.2015.01.005
Quinn SC, Jamison AM, An J et al (2019) Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: results of a national survey of White and African American adults. Vaccine 37(9):1168–1173. https://doi.org/10.1016/j.vaccine.2019.01.033
Sadaf A, Richards JL, Glanz J et al (2013) A systematic review of interventions for reducing parental vaccine refusal and vaccine hesitancy. Vaccine 31(40):4293–4304. https://doi.org/10.1016/j.vaccine.2013.07.013
Salmon DA, Dudley MZ, Glanz JM, Omer SB (2015) Vaccine hesitancy: causes, consequences, and a call to action. Vaccine 33(4):66–71. https://doi.org/10.1016/j.vaccine.2015.09.035
Şencan H (2005) Sosyal ve Davranışsal Ölçümlerde Güvenilirlik ve Geçerlilik, (First Edition). Seçkin Yayıncılık, Ankara. [Reliability and Validity in Social and Behavioral Measurements]
Siddiqui M, Salmon DA, Omer SB (2013) Epidemiology of vaccine hesitancy in the United States. Human Vaccines Immunotherapeut 9(12):2643–2648. https://doi.org/10.4161/hv.27243
Türkiye Nüfus Sağlık Araştırması (TNSA) (2018) Turkey Demographic and Health Surveys. http://www.hips.hacettepe.edu.tr/tr/nufus_ve_saglik_arastirmalari_serisi-59. Accessed 10 Apr 2022
World Health Organization (2019) Vaccination: European Commission and World Health Organization join forces to promote the benefits of vaccines. WHO, Geneva. https://www.who.int/news/item/12-09-2019-vaccination-european-commission-and-world-health-organization-join-forces-to-promote-the-benefits-of-vaccines Accessed 10 Apr 2022
World Health Organization (2020). Immunization, vaccines and biologicals. WHO, Geneva. https://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/. Accessed 10 Apr 2022
Yorulmaz DS, Karadeniz H (2022) Vaccination refusal debate on social media in Turkey: a content analysis of the comments on instagram blogs. Iran J Public Health 51(3):615–623. https://doi.org/10.18502/ijph.v51i3.8938
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by [Selma Durmuş Sarikahya], [Emel Güden] and [Deniz Sümeyye Yorulmaz]. The first draft of the manuscript was written by [Selma Durmuş Sarikahya] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical considerations
The study was approved by an ethics committee (E-18457941-050.99-31187). Permission was obtained from the FHCs (No: 93079172-703.01 & Topic: Permission for Research). All patients were informed about the research purpose and procedure. Informed consent was obtained from those who agreed to participate in the study. The research was conducted according to the ethical principles outlined by the Declaration of Helsinki.
Consent for publication
Publication permission was obtained from the participants.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to an error in the Ethical considerations section.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Durmuş Sarıkahya, S., Güden, E. & Sümeyye Yorulmaz, D. Childhood vaccine hesitancy in two regions with different socioeconomic backgrounds in Turkey. J Public Health (Berl.) 32, 737–746 (2024). https://doi.org/10.1007/s10389-023-01854-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10389-023-01854-z