Abstract
Background
Calcium (Ca)-based phosphate (P) binders, compared to non-Ca-based P binders, contribute to vascular calcification, which is associated with cardiovascular events.
Methods
The LANDMARK study is a multicenter, randomized, open-label, parallel comparative study of lanthanum carbonate (LC) and calcium carbonate (CC) in hemodialysis patients. Stable hemodialysis patients with intact parathyroid hormone ≤240 pg/mL meeting ≥1 of the following criteria (age >65 years, postmenopause, diabetes mellitus) were randomized into the LC and CC groups. LC group patients initially received LC 750 mg/day or the previously used dose and were titrated up to a maximum 2250 mg/day to achieve serum P levels of 3.5–6.0 mg/dL. CC group patients received CC 3 g/day or the previously used dose and were titrated to achieve the same P range. If the target serum P level was not achieved, non-Ca-based P binders (other than LC) could also be added. The primary endpoint is survival time free of cardiovascular events, including cardiovascular death, non-fatal myocardial infarction or stroke, and unstable angina.
Results
Overall, 2309 patients were allocated to the LC (N = 1154) or CC group (N = 1155). At baseline, the mean age was 68.4 years, 40.4 % were women, 55.9 % had diabetes, 18.3 % had a history of ischemic heart disease, and 13.9 % had cerebrovascular disease. A total of 184 patients (8.4 %) had undergone coronary intervention procedures. Baseline characteristics were well balanced between groups.
Conclusions
The LANDMARK study will determine whether LC, a non-Ca-based P binder, reduces cardiovascular mortality and morbidity in chronic hemodialysis patients.
Similar content being viewed by others
Introduction
Cardiovascular disease (CVD) is the leading cause of death among dialysis patients. Many uremia-associated factors are involved in the high cardiovascular mortality and morbidity [1]. Clinical and experimental studies showed that phosphate (P) overload plays a pivotal role in CVD development in uremic patients. In fact, hyperphosphatemia is significantly associated with mortality and cardiovascular events (CVEs) among chronic kidney disease (CKD) patients receiving or not receiving dialysis [2–4]. Vascular calcification is also a likely predictor of mortality and CVEs [5, 6]. The pathomechanism underlying vascular calcification in uremia remains obscure, but the transition of vascular smooth muscle cells into osteoblast-like cells promoted by P and calcium (Ca) overload is considered to be an important step [7, 8].
Traditionally, Ca-based P binders, including calcium carbonate (CC) and calcium acetate (CA), have been widely used in clinical settings. However, it has been indicated that Ca-based P binder use might promote vascular calcification through positive Ca balance, which might lead to increased mortality and CVEs. In a meta-analysis of 11 randomized control trials (RCTs) in hemodialysis patients, patients receiving non-Ca-based P binders had a 22 % reduction in all-cause mortality compared to those receiving Ca-based P binders [9]. However, individual RCTs have not always demonstrated clear superiority of non-Ca-based P binders over Ca-based P binders for reducing mortality and CVEs [10–20]. Thus, so far, there is no obvious evidence that non-Ca-based P binders improve mortality and CVEs in dialysis patients. Lanthanum carbonate (LC), which is a non-Ca-based P binder, has been clinically available since 2009 in Japan. LC effectively decreases serum P concentration with a lower incidence of hypercalcemia in hyperphosphatemic patients on regular hemodialysis [21, 22]. In addition, small-scale RCTs have demonstrated that LC slows progression of aortic calcification compared to that with CC in chronic hemodialysis patients [23, 24]. The LANDMARK (outcome study of lanthanum carbonate compared with calcium carbonate on cardiovascular mortality and morbidity in patients with chronic kidney disease on hemodialysis) study was planned to elucidate whether LC treatment reduces CVD mortality and morbidity compared to that with CC treatment in regular hemodialysis patients. In addition, we performed a subsidiary study (LANDMARK-SS) in which progression of coronary artery calcification (CAC) was compared between groups in enrolled patients undergoing multi-detector row computed tomography.
Materials and methods
Study design
The LANDMARK study is a multicenter, randomized, open-label, parallel comparative study conducted among outpatients on regular hemodialysis. The study protocol and informed consent form were approved by the institutional review boards of each center. Written informed consent for participation was obtained from each patient. This study is being conducted in accordance with the Declaration of Helsinki and the Ethical Guideline on Clinical Studies by the Ministry of Health, Labour and Welfare of Japan. The study has been registered with ClinicalTrials.gov (NCT01578200) and umin.ac.jp (UMIN000006815).
Study patients
The current study enrolled patients who had been on hemodialysis for at least 3 months and required P binder therapy. All patients had at least one vascular calcification risk factor [elderly (≥65 years), postmenopausal woman, or type 2 diabetes mellitus] with intact parathyroid hormone (iPTH) ≤240 pg/mL and life expectancy ≥1 year. Diabetes mellitus was defined as: (1) fasting plasma glucose level ≥126 mg/dL (7.0 mmol/L), (2) random plasma glucose level or 2-h plasma glucose value in a 75 g oral glucose tolerance test ≥200 mg/dL (11.1 mmol/L), (3) hemoglobin A1c (HbA1c, NGSP: National Glycohemoglobin Standardization Program) ≥6.5 %, or (4) the use of antidiabetes medication.
Patients were excluded if (1) they were undergoing peritoneal dialysis, (2) they had contraindications to LC or CC, swallowing disorders, severe gastrointestinal disorders, history of bowel obstruction, history of ischemic heart disease/stroke within the previous 6 months, New York Heart Association (NYHA) classification III–IV heart failure, arrhythmia requiring treatment, severe liver dysfunction, severe malnutrition, or malignancy within 5 years, (3) they were pregnant or possibly pregnant or lactating and/or planned to be pregnant within the study term, or (4) they were ineligible according to the investigator’s judgment.
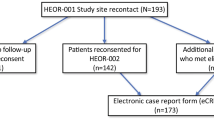
Patients were enrolled between November 2011 and June 2014 from 273 centers across the country. Although the planned enrollment period had been initially 2 years, it was extended by 8 months due to insufficient accrual of patients. Patient follow-up is ongoing and will end in June 2017. To explore the effect of LC on the coronary artery, an imaging subsidiary study focusing on coronary calcification using multidetector computed tomography (Agatston score) is concurrently in progress (UMIN000006816). The details of the subsidiary study will be reported elsewhere.
Interventions
Study drugs were administered within 14 days after registration and continued until 3 years after the last patient registration. Patients assigned to the LC group initially received an oral dose of 750 mg/day (3 times immediately after meals) or the previously used dose. To achieve P levels of 3.5–6 mg/dL, patients were titrated up to a maximum of 2250 mg/day. Titration intervals were longer than a week, and the dose increased by <750 mg/day. If the P level was not achieved with 2250 mg/day or the maximum tolerated dose, sevelamer hydrochloride or non-Ca-based P binders could be added. CC was prohibited in the LC group.
Patients assigned to the CC group received an oral dose of 3 g/day (3 times immediately after meals) or the previously used dose. To achieve the desired P levels, patients were titrated. If the P level was not achieved with the maximum tolerated dose, sevelamer hydrochloride or non-Ca-based P binders could be added. LC was prohibited in the CC group.
Outcomes
The primary endpoint is the CVE-free survival. CVEs consisted of (1) death due to CVD (myocardial infarction or stroke), including sudden cardiac death (International Classification of Diseases: ICD-10 codes R96.0/96.1), (2) non-fatal myocardial infarction, (3) non-fatal stroke, including transient ischemic attack (TIA), (4) unstable angina, (5) hospitalization for heart failure (HF), and (6) hospitalization for ventricular arrhythmia. CVE-free survival was defined as the time from the date of the first administration to the date of the first documented CVE.
The secondary endpoints include overall survival, secondary hyperparathyroidism-free survival, hip fracture-free survival, and adverse drug reactions. Adverse drug reactions (other than efficacy end-point components) are collected until 30 days after completion of the protocol treatment if the investigators cannot deny a causal relationship between the investigational drugs and the adverse events. The quality of life questionnaire (kidney disease quality of life short form: KDQOL-SF, v1.3) and bone mineral density by dual energy X-ray absorptiometry are examined at selected institutes.
Myocardial infarction is defined as chest symptoms consistent with myocardial ischemia lasting more than 30 min, suspected/definite electrocardiographic changes indicative of ischemia in at least 2 contiguous leads, and cardiac biomarker elevation. Stroke is defined by imaging (computed tomography or magnetic resonance imaging) evidence of cerebral focal ischemia in a defined vascular distribution. Strokes are classified into ischemic or hemorrhagic stroke. Transient ischemic attack is defined as a transient episode of neurological dysfunction caused by focal brain, spinal cord, or retinal ischemia without acute infarction [25]. Unstable angina is defined according to a previous report [26]. HF hospitalization is defined as an event that meets: admission with a primary diagnosis of HF, new or worsening symptoms due to HF, and diagnostic evidence, such as echocardiography. Secondary hyperparathyroidism is defined as iPTH >240 pg/mL. Hip fracture due to high-energy trauma is not an endpoint.
Sample size
Based on the Japanese Society for Dialysis Therapy, the annual crude mortality of Japanese patients on dialysis was 9.7 % in 2010 [27]. The cardiovascular mortality was 3.9 %, and the cardiovascular non-fatal event rate was estimated as 3.9 %. Therefore, estimated annual CVE rate was 7.8 %. Based on the assumptions of a hazard ratio of 0.8, two-tailed alpha of 0.05, and 80 % power, 1231 subjects were required for each group. Taking into consideration a 10 % drop-out rate, the sample size was set to be 1500 for each group and 3000 overall.
Randomization
The patients were enrolled through a web-based registration and follow-up system provided by the data center at the Translational Research Informatics Center, Kobe, Japan. After obtaining the informed consent from each patient, the primary physician was allowed to access to the system for sending the information required for enrollment. The system automatically evaluated the eligibility of each patient and randomly assigned participants to either the LC group or CC group (1:1 allocation). When allocation was performed, age (<65 years old vs. not), sex (female vs. male), diabetes (absence vs. presence), and site were dynamically balanced between the two groups.
Statistical analyses
The safety analysis comprised the data from eligible patients who received at least one dose of the study drug. The full analysis set comprised the data from patients who received at least one dose of the study drug, met all inclusion criteria, and did not meet any exclusion criterion. This will be the primary analysis set for the efficacy endpoints. The per protocol set comprised the data from patients who received at least one dose of the study drug, met all inclusion criteria, did not meet any exclusion criterion, and had no major protocol violations.
The cumulative incidences of events will be estimated using the Kaplan–Meier method. Two treatment groups will be compared using the log-rank test. As for the quality of life and the bone mineral density tests, patterns of change in each parameter over time and how the patterns differed between the two treatment groups will be investigated using linear mixed effects models. The model will include the treatment group and time as fixed effects and patient as a random effect. In the safety analysis set, incidences of adverse events will be compared between the two groups using a Fisher’s exact test. All analyses will be performed using the SAS software version 9.3 (Cary, NC, USA), and the level of significance is P < 0.05 (two-tailed).
Results
In the current study, 2309 patients in 273 participating centers were enrolled from November 2011 to June 2014. Of these, 236 patients were enrolled for the concurrent imaging subsidiary study on CAC. The 2309 patients were randomly allocated to the LC group (1154 patients) or CC group (1155 patients). However, due to ineligibility found after randomization, consent withdrawal, or overlapped registration, 18 patients in the LC group and 24 in the CC group were excluded from the study. In addition, 45 patients did not take LC in the LC group, and 38 patients did not take CC in the CC group.
The baseline characteristics of the patients are shown in Table 1. The average age of patients was 68.4 years old, and 59.6 % of the subjects were male. Almost all patients (94.8 %) had previously received P binders, and 30.8 % had previously taken LC. The primary causes of CKD were diabetes (49.5 %) and glomerulonephritis (22.8 %). A history of ischemic heart disease and cerebrovascular disease was seen in 18.3 and 13.9 % of patients, respectively.
In addition, most patients (98.1 %) underwent dialysis 3 days per week for 4 h per day (Table 2). Hemodialysis was most frequently used technique (89.7 %). Mean serum Ca, P, and iPTH concentrations were 8.9 mg/dL, 5.3 mg/dL, and 122 pg/mL, respectively. Baseline characteristics were well balanced between the two groups, except for the proportion of other P binder use.
Discussion
Observational studies have shown that an increment of P burden deteriorates mortality and the CVE frequency among dialysis patients [1, 8, 28–30]. Therefore, nephrologists have sought to achieve optimal P management. In addition to their tolerability, Ca-based P binders are inexpensive and very effective in reducing serum P concentration [31, 32]. However, administration of Ca-based P binders evokes Ca overload, which are likely to accelerate vascular calcification, thereby potentially leading to increased morality and the CVE frequency [33–36]. Although a meta-analysis suggested that non-Ca-based P binders are associated with a decreased risk of all-cause mortality compared with Ca-based P binders in CKD patients, individual study demonstrated that non-Ca-based P binders have not always been shown to improve mortality and/or to slow the progression of vascular calcification, probably because of the small numbers of study patients and outcome events [9–18, 20, 23, 30]. They reported that a statistically significant difference in mortality was confirmed between patients receiving non-Ca-based P binders and those receiving Ca-based P binders in their analysis of five clinical trials with a follow-up duration of 24 months [9]. In contrast, in six trials with a follow-up duration of <24 months, there was no significant differences in mortality between patients taking the two drugs [10, 11, 13, 18, 19, 30]. A benefit of non-Ca-based P binders might emerge over time. The duration of follow-up is set at 3 years in the LANDMARK study, which is considered to be sufficient to assess the effects of LC on cardiovascular mortality and morbidity compared to those of CC.
In a RCT, all-cause mortality was significantly lower in sevelamer treatment group compared with Ca-based P binder treatment group among elderly patients ≥65 years of age [19]. Similarly, although LC treatment compared to standard therapy did not reduce mortality in all enrolled patients, LC was significantly associated with survival benefit in elderly patients with >65 years of age [37]. The mean age (68 years) of the patients enrolled into the LANDMARK study was older than that in previous RCTs, and the mean hemodialysis duration was longer.
Although the target number of enrolled patients was set at a total of 3000 patients (1500 in each treatment arm) because of the sample size assumption, in actuality, a total of 2309 patients (1154 in LC treatment, 1155 in CC treatment) were enrolled into the LANDMARK study. Despite the smaller number of patients than initially targeted, extension of follow-up period by 8 months could contribute to preservation of the statistical power. The number of enrolled patients in this study was still larger than that in any previous RCTs comparing the effect of non-Ca-based P binders with that of Ca-based P binders on mortality among dialysis patients.
The CAC score is a useful surrogate marker for cardiovascular mortality and morbidity in CKD patients [5, 14, 30, 36]. Block et al. reported that the baseline CAC score was a significant predictor of mortality in incident hemodialysis patients [13]. Ca-based P binder use is likely to be involved not only in the progression of CAC [10, 12, 33], but also in increased mortality [13, 14, 19]. To date, there is limited information on differences in vascular calcification extent, CVE frequency, or mortality between dialysis patients receiving LC and those receiving Ca-based P binders. We will investigate whether LC improves the progression of CAC as compared with CC in the accompanying study (LANDMARK-SS).
Final results of the LANDMARK clinical trial would allow nephrologists to validly assess the clinically meaningful effects of ameliorated Ca burden by LC use on CVD mortality and morbidity in patients on hemodialysis.
References
Block GA, Hulbert-Shearon TE, Levin NW, Port FK. Association of serum phosphorus and calcium × phosphate product with mortality risk in chronic hemodialysis patients: a national study. Am J Kidney Dis. 1998;31:607–17.
Ritz E, Gross ML. Hyperphosphatemia in renal failure. Blood Purif. 2005;23:6–9.
Zoccali C, Mallamaci F, Tripepi G. Novel cardiovascular risk factors in end-stage renal disease. J Am Soc Nephrol. 2004;15(Suppl 1):S77–80.
Kestenbaum B, Sampson JN, Rudser KD, et al. Serum phosphate levels and mortality risk among people with chronic kidney disease. J Am Soc Nephrol. 2005;16:520–8.
Blacher J, Guerin AP, Pannier B, et al. Arterial calcifications, arterial stiffness, and cardiovascular risk in end-stage renal disease. Hypertension. 2001;38:938–42.
London GM, Guérin AP, Marchais SJ, et al. Arterial media calcification in end-stage renal disease: impact on all-cause and cardiovascular mortality. Nephrol Dial Transplant. 2003;18:1731–40.
Jono S, McKee MD, Murry CE, et al. Phosphate regulation of vascular smooth muscle cell calcification. Circ Res. 2000;87:E10–7.
Ogata H, Koiwa F, Kinugasa E, Akizawa T. CKD-MBD: impact on management of kidney disease. Clin Exp Nephrol. 2007;11:261–8.
Jamal SA, Vandermeer B, Raggi P, et al. Effect of calcium-based versus non-calcium-based phosphate binders on mortality in patients with chronic kidney disease: an updated systematic review and meta-analysis. Lancet. 2013;382:1268–77.
Chertow GM, Burke SK, Raggi P, Treat to Goal Working Group. Sevelamer attenuates the progression of coronary and aortic calcification in hemodialysis patients. Kidney Int. 2002;62:245–52.
Sadek T, Mazouz H, Bahloul H, et al. Sevelamer hydrochloride with or without alphacalcidol or higher dialysate calcium vs calcium carbonate in dialysis patients: an open-label, randomized study. Nephrol Dial Transplant. 2003;18:582–8.
Braun J, Asmus HG, Holzer H, et al. Long-term comparison of a calcium-free phosphate binder and calcium carbonate–phosphorus metabolism and cardiovascular calcification. Clin Nephrol. 2004;62:104–15.
Block GA, Raggi P, Bellasi A, et al. Mortality effect of coronary calcification and phosphate binder choice in incident hemodialysis patients. Kidney Int. 2007;71:438–41.
Block GA, Spiegel DM, Ehrlich J, et al. Effects of sevelamer and calcium on coronary artery calcification in patients new to hemodialysis. Kidney Int. 2005;68:1815–24.
Russo D, Miranda I, Ruocco C, et al. The progression of coronary artery calcification in predialysis patients on calcium carbonate or sevelamer. Kidney Int. 2007;72:1255–61.
Barreto DV, de Barreto FC, de Carvalho AB, et al. Phosphate binder impact on bone remodeling and coronary calcification–results from the BRIC study. Nephron Clin Pract. 2008;110:c273–83.
Borzecki AM, Lee A, Wang SW, et al. Survival in end stage renal disease: calcium carbonate vs. sevelamer. J Clin Pharm Ther. 2007;32:617–24.
Qunibi W, Moustafa M, Muenz LR, et al. A 1-year randomized trial of calcium acetate versus sevelamer on progression of coronary artery calcification in hemodialysis patients with comparable lipid control: the Calcium Acetate Renagel Evaluation-2 (CARE-2) study. Am J Kidney Dis. 2008;51:952–65.
Suki WN, Dialysis Clinical Outcomes Revisited Investigators. Effects of sevelamer and calcium-based phosphate binders on mortality in hemodialysis patients: results of a randomized clinical trial. J Ren Nutr. 2008;18:91–8.
Takei T, Otsubo S, Uchida K, et al. Effects of sevelamer on the progression of vascular calcification in patients on chronic haemodialysis. Nephron Clin Pract. 2008;108:c278–83.
Shigematsu T, Lanthanum Carbonate Group. Multicenter prospective randomized, double-blind comparative study between lanthanum carbonate and calcium carbonate as phosphate binders in Japanese hemodialysis patients with hyperphosphatemia. Clin Nephrol. 2008;70:404–10.
Shigematsu T, Lanthanum Carbonate Research Group. Three-year extension study of lanthanum carbonate therapy in Japanese hemodialysis patients. Clin Exp Nephrol. 2010;14:589–97.
Toussaint ND, Lau KK, Polkinghorne KR, Kerr PG. Attenuation of aortic calcification with lanthanum carbonate versus calcium-based phosphate binders in haemodialysis: a pilot randomized controlled trial. Nephrology (Carlton). 2011;16:290–8.
Wada K, Wada Y. Evaluation of aortic calcification with lanthanum carbonate vs. Calcium-based phosphate binders in maintenance hemodialysis patients with type 2 diabetes mellitus: an open-label randomized controlled trial. Ther Apher Dial. 2014;18:353–60.
Easton JD, Saver JL, Albers GW, et al. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40:2276–93.
Austen WG, Edwards JE, Frye RL, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975;51(4 Suppl):5–40.
Nakai S, Iseki K, Itami N, et al. An overview of regular dialysis treatment in Japan (as of 31 December 2010). Ther Apher Dial. 2012;16:483–521.
Block GA, Klassen PS, Lazarus JM, Ofsthun N, Lowrie EG, Chertow GM. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J Am Soc Nephrol. 2004;15:2208–18.
Fukagawa M, Kido R, Komaba H, et al. Abnormal mineral metabolism and mortality in hemodialysis patients with secondary hyperparathyroidism: evidence from marginal structural models used to adjust for time-dependent confounding. Am J Kidney Dis. 2014;63:979–87.
Kakuta T, Tanaka R, Hyodo T, et al. Effect of sevelamer and calcium-based phosphate binders on coronary artery calcification and accumulation of circulating advanced glycation end products in hemodialysis patients. Am J Kidney Dis. 2011;57:422–31.
Morinière P, Djerad M, Boudailliez B, et al. Control of predialytic hyperphosphatemia by oral calcium acetate and calcium carbonate. Comparable efficacy for half the dose of elemental calcium given as acetate without lower incidence of hypercalcemia. Nephron. 1992;60:6–11.
St Peter WL, Fan Q, Weinhandl E, Liu J. Economic evaluation of sevelamer versus calcium-based phosphate binders in hemodialysis patients: a secondary analysis using centers for medicare and medicaid services data. Clin J Am Soc Nephrol. 2009;4:1954–61.
Galassi A, Spiegel DM, Bellasi A, et al. Accelerated vascular calcification and relative hypoparathyroidism in incident haemodialysis diabetic patients receiving calcium binders. Nephrol Dial Transplant. 2006;21:3215–22.
Raggi P, Bommer J, Chertow GM. Valvular calcification in hemodialysis patients randomized to calcium-based phosphorus binders or sevelamer. J Heart Valve Dis. 2004;13:134–41.
Chertow GM, Raggi P, Chasan-Taber S, et al. Determinants of progressive vascular calcification in haemodialysis patients. Nephrol Dial Transplant. 2004;19:1489–96.
Goodman WG, Goldin J, Kuizon BD, et al. Coronary-artery calcification in young adults with end-stage renal disease who are undergoing dialysis. N Engl J Med. 2000;342:1478–83.
Wilson R, Zhang P, Smyth M, Pratt R. Assessment of survival in a 2-year comparative study of lanthanum carbonate versus standard therapy. Curr Med Res Opin. 2009;25:3021–8.
Acknowledgments
This investigator-initiated research study was financed by Bayer Yakuhin, Ltd., which commercializes lanthanum carbonate hydrate. However, the funders had no role in the study design, data collection, handling, evaluation or analysis, decision to publish, or preparation or writing this manuscript. The authors thank the following additional investigators in the Translational Research Informatics Center (TRI) in the Foundation for Biomedical Research and Innovation (FBRI), a public interest incorporated foundation for their helpful contributions to this trial: Mr. Satoshi Nakagawa for project management; Ms. Emiko Uno for data management; Mr. Eiji Nakatani for statistical analyses; Dr. Shinsuke Kojima, Mr. Mikio Yoshidomi, and Dr. Atsuhiko Kawamoto for manuscript writing/review and Dr. Masanori Fukushima for supervising these jobs in TRI.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
MF, HH, and TA have received honoraria from Bayer Yakuhin, Ltd. All other authors have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee at which the studies were conducted (IRB approval number 115103) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Ogata, H., Fukagawa, M., Hirakata, H. et al. Design and baseline characteristics of the LANDMARK study. Clin Exp Nephrol 21, 531–537 (2017). https://doi.org/10.1007/s10157-016-1310-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-016-1310-8