Abstract
Background
The risk of developing CKD is increased in HIV-infected patients; however, the relationship between renal function decline and lipid abnormalities currently remains unclear in these patients.
Methods
A retrospective cohort study was conducted on 661 HIV-infected patients, whose estimated glomerular filtration rates (eGFRs) were consecutively measured over 6 years. The rate of declines in eGFR per year was calculated, with decreases being evaluated using a linear mixed effect model. The distribution of decreases in eGFR ≥ 30 % from baseline during the follow-up period was compared across quartiles of non-high-density lipoprotein cholesterol (HDL-C) levels using the Cochran–Armitage test. A multivariate logistic regression model was built to examine the relationship between dyslipidemia and decreases in eGFR.
Results
The prevalence of CKD increased from 8.5 to 21.2 % during the follow-up. The average of 6 annual eGFR decline rates was 2.01 ± 0.09 ml/min/1.73 m2/year, which was more than 6-fold higher than that of age-matched controls. The distribution of decreases in eGFR significantly increased across the quartiles of non-HDL-C (p value for trend = 0.0359). Non-HDL-C levels greater than the median value of the cohort were identified as a significant risk factor for decreased eGFR [odds ratio (95 % confidence interval), 1.77 (1.07–3.00)].
Conclusion
Increased non-HDL-C levels are a risk factor for renal function decline in HIV-infected patients.
Similar content being viewed by others
Introduction
Since the longevity of patients infected with human immunodeficiency virus (HIV) has been increased by combination antiretroviral therapy (cART), kidney diseases have emerged as a significant cause of morbidity and mortality [1]. The prevalence of chronic kidney disease (CKD) was previously reported to be between 15.4 and 24 % in HIV-infected patients across several countries [1–4]; however, consecutive changes in renal function have not yet been examined over a long period of time. Some antiretroviral agents, such as indinavir (IDV), tenofovir disoproxil fumarate (TDF), and atazanavir (ATV), directly induce acute and chronic kidney diseases, while some protease inhibitors have been shown to increase the incidence of hypertension (HT), diabetes mellitus (DM), and dyslipidemia (DL). These comorbidities increase the risk of kidney disease [5–8]; therefore, HIV care experts need to consider more appropriate treatments from the viewpoint of renal safety.
Among the comorbidities described above, DL is commonly disregarded as a cause of CKD. In clinical and research settings worldwide, low-density lipoprotein (LDL)-cholesterol (C) is typically estimated using the Friedewald equation due to the lack of a direct and reliable assay for LDL-C. However, this equation is often difficult to use for HIV-infected patients due to their high triglyceride (TG) levels, particularly in a non-fasting state. Therefore, from a practical point of view, we focused on non-high-density lipoprotein-C (HDL-C) as a marker of DL in HIV-infected patients. Serum non-HDL-C levels are calculated by subtracting HDL-C levels from total cholesterol (TC) levels, and represent the sum of cholesterol included in LDL, intermediate-density lipoprotein (IDL), very low-density lipoprotein (VLDL), and other remnant lipoproteins; thus, they reflect the total amount of apolipoprotein B (apo B). Accordingly, non-HDL-C may be a better marker of atherogenicity than LDL-C alone [9], and is considered a risk factor for cerebro-cardiovascular diseases in the general population [10–16]. Regarding kidney diseases, Samuelsson et al. showed that elevated plasma concentrations of apoB, which may be similar to those of non-HDL-C, correlated with the rapid progression of renal insufficiency, even after adjustments for the presence of proteinuria in a prospective cohort study of non-diabetic patients with primary CKD [17]. Additionally, Pan et al. found that non-HDL-C correlated with urinary albumin excretion rates in 507 type 2 diabetic Chinese patients with normal renal function [18]. However, it currently remains unclear whether serum levels of non-HDL-C are involved in the development of kidney diseases in HIV-infected patients.
Therefore, we herein examined long-term changes in the estimated glomerular filtration rate (eGFR) and the impact of elevated non-HDL-C levels on future declines in renal function among HIV-infected individuals.
Materials and methods
Subjects and definitions
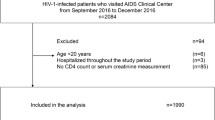
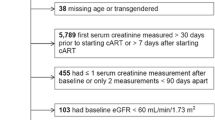
A retrospective cohort study was undertaken to investigate annual changes in eGFR. Consecutive data of eGFR over 6 years between 2008 and 2014 were obtained from 661 HIV-infected patients receiving cART (mean age, 46 ± 12 years). This cohort included 598 men (90.5 %) and 622 Japanese patients (94.1 %). This study was approved by the Institutional Review Board of Tokyo Metropolitan Komagome Hospital (approval certificate no. 1014) and was conducted in accordance with the Declaration of Helsinki Principles on Human Experimentations. Informed consent was obtained from all participants prior to enrollment. The electronic medical records of all patients in the cohort were reviewed in order to determine changes in eGFR and identify risk factors for reductions in eGFR. Decreased eGFR was defined as an eGFR decline ≥30 % from baseline during the 6-year follow-up period. Albuminuria was defined as a urinary albumin creatinine (Cr) ratio (UACR) ≥ 30 mg/g. CKD was defined as an eGFR < 60 ml/min/1.73 m2, sustained for at least 3 months. Incident CKD was defined as the new onset of eGFR < 60 ml/min/1.73 m2 among those without CKD at baseline (n = 544). HT was defined as a systolic blood pressure 140 mmHg and/or a diastolic blood pressure 90 mmHg or the use of antihypertensive agents at baseline. DM was defined as a diagnosis of DM prior to baseline or the use of oral anti-diabetic agents or insulin at baseline. Hepatitis C virus (HCV) infection was defined as a positive reactive HCV antibody test. Non-HDL-C levels were calculated by subtracting HDL-C from TC, and were used as a representative index of DL in this study.
Measurements
All patients provided blood and urine samples in a non-fasting state for analysis as part of a routine clinical visit. Blood cell count and routine laboratory data were measured using standard methods with the automated analyzer SF-3000 Sysmex (Hitachi, Tokyo, Japan). Serum Cr was measured by an enzymatic method (N-assay L Creatinine Kit; Nittobo Medical Co. Ltd., Tokyo, Japan). eGFR was calculated based on serum Cr concentrations, using the following equation: GFR (mL/min/1.73 m2) = 194 × Cr−1.094 × Age−0.287 × 0.739 (if female), which was developed for Japanese individuals by the Japanese Society of Nephrology due to inaccuracies in the modification of diet in renal disease (MDRD) equation for Asian people, including Japanese [19]. Urinary albumin was measured by a turbidimetric immunoassay and urine Cr was assayed using an enzymatic method. Total albumin urinary concentrations were standardized to urinary Cr of 1 g/L, and denoted as UACR. CD4 cell counts in HIV-infected patients were determined using a specific monoclonal antibody and flow cytometry analysis. HIV-RNA levels were measured using the Roche Amplicor HIV Monitor assay based on the reverse transcription–polymerase chain reaction (Roche Molecular Systems, Tokyo, Japan; the lower detection limit was 50 copies/mL). Anti-HCV antibodies were measured using a third-generation enzyme immunoassay test (Abbott Laboratories, Tokyo, Japan).
Statistical analysis
The date are expressed as the mean ± standard deviation (SD), unless otherwise stated. The mean ± standard error (SE) is used, when consecutive decreases in eGFR during the follow-up period are shown. The prevalences of CKD at 2008 and 2014 were compared as categorical variables using the Chi squared test. Paired differences between the baseline (2008) and subsequent annual rates of declines in eGFR were analyzed using the Student’s paired t test. All paired t-test analyses used a strict p-value cut-off of 0.00833 to account for multiple testing (six comparisons with the baseline measurement). The average of 6 annual rates of declines in eGFR was defined by ‘the annual rate of decline in eGFR’, which was evaluated using a linear mixed-effects model as an extension of the linear regression model for evaluating data collected and summarized in groups [20]. A multivariate logistic regression model was constructed to examine the relationship between an increase in non-HDL-C levels and reductions in eGFR, which was defined as an eGFR decline ≥30 % from baseline during the 6-year follow-up. The following baseline data were initially incorporated into a univariate model as covariates: age, gender, presence or absence of DM, HT, and HCV infection, UACR ≥ 30 mg/g, eGFR < 60 ml/min/1.73 m2, CD4 cell counts <200 cells/μL, HIV-RNA >50 copies/mL, cumulative exposure to either TDF, IDV or ATV, and non-HDL-C > 134 mg/dL (the median value of all HIV participants). Factors with p values less than 0.20 in the univariate model were incorporated into a multivariate model. The odds ratio (OR) with its 95 % confidence interval (CI) was calculated to evaluate the risk for each factor. The distributions of incident eGFR decline ≥30 % and incident CKD were compared across quartiles of serum non-HDL-C levels using the Cochran–Armitage test. All statistical analyses were performed using JMP 11.0.2 (SAS Institute Japan, Tokyo, Japan) and EZR, which is a graphical user interface for R, version 2.14.0 (http://www.r-project.org/) [21]. A p value less than 0.05 was considered significant in all analyses.
Results
Demographics and laboratory characteristics of HIV-infected patients
The demographic and clinical characteristics of all participants are shown in Table 1. The prevalences of HT, DM, and HCV co-infection were 18.8 % (n = 124), 6.7 % (n = 44), and 4.1 % (n = 27), respectively. The mean duration of cART use was 5 years. The number of patients on current cART was 596 patients (90.2 %) including 322 (48.7 %) receiving TDF, 4 (0.61 %) receiving IDV, and 233 (35.3 %) receiving ATV, respectively. The number of recipients on statins and fibrates were 44 (6.7 %), 48 (7.3 %), respectively. The mean UACR (log UACR), eGFR, and serum cystatin C levels at enrollment were 101 ± 596 mg/g (1.18 ± 0.61), 85.3 ± 19.6 ml/min/1.73 m2, and 0.80 ± 0.25 mg/L, respectively. The mean CD 4 cell count was 411 ± 204 cells/μL and the proportion of HIV-RNA <50 copies/mL was 81.7 %. The mean values of TC and HDL-C were 195 ± 42 and 55.3 ± 16.9 mg/dL, respectively. The mean and median (range) values of non-HDL-C were 140 ± 41 mg/dL and 134 (50–355) mg/dL, respectively.
Consecutive decreases in eGFR and progression to CKD stages 3–5
A total of 509 out of 661 HIV-infected patients (81.1 %) showed a decline in eGFR over the 6-year follow-up period: 11.8 ± 14.6 ml/min/1.73 m2 (mean ± SD) and 12.1 [−38.2 to 108] ml/min/1.73 m2 [median (range)]. The eGFR [mean ± standard error (SE)] of each year decreased over time from 2008 to 2014 (85.3 ± 0.76 ml/min/1.73 m2 in 2008, 82.2 ± 0.71 ml/min/1.73 m2 in 2009, 78.3 ± 0.68 ml/min/1.73 m2 in 2010, 77.8 ± 0.70 ml/min/1.73 m2 in 2011, 76.4 ± 0.73 ml/min/1.73 m2 in 2012, 73.8 ± 0.71 ml/min/1.73 m2 in 2013, and 73.0 ± 0.74 ml/min/1.73 m2 in 2014), as shown in Fig. 1. The average of the 6 annual rates of declines in the eGFR between 2008 and 2014 was denoted by ‘the annual rate of decline in eGFR’, which was 2.01 ± 0.09 ml/min/1.73 m2/year (mean ± SE). The prevalence of CKD in 2014 was almost 2.5-fold higher than that in 2008 (21.2 vs 8.5 %, p < 0.0001). Seventy-two (13.2 %) out of all patients with CKD stage <3 at enrollment (n = 544) progressed to CKD stage ≥3 during the 6-year follow-up period, and seven (6.0 %) out of 117 CKD stage ≥3 received chronic hemodialysis therapy. Twenty-nine patients (4.4 %) died during the study period, half of whom died of cancer.
Consecutive decreases in eGFR during the follow-up period. The figure shows consecutive decreases in eGFR during the follow-up period. Between 2008 and 2014, mean eGFR values decreased over time with a significant difference being observed between each year and 2008 (mean ± standard error: 85.3 ± 0.76 in 2008, 82.2 ± 0.71 in 2009, 78.3 ± 0.68 in 2010, 77.8 ± 0.70 in 2011, 76.4 ± 0.73 in 2012, 73.8 ± 0.71 in 2013, and 73.0 ± 0.74 ml/min/1.73 m2 in 2014). Asterisk (*) indicates a significant difference between each year and 2008
Factors associated with reductions in eGFR
Decreased eGFR was defined as an eGFR decline ≥30 % from baseline during the 6-year follow-up. Univariate and multivariate logistic regression analyses were performed in order to identify factors associated with decreased eGFR (Table 2). The multivariate logistic regression analysis identified being female [OR (95 % CI), 2.51 (1.20–5.02)], non-HDL-C ≥ 134 mg/dL [1.77 (1.07–3.00)], UACR ≥ 30 mg/g [2.21 (1.24–3.90)], and CD 4 cell counts <200 cells/μL [2.83 (1.49–5.24)] as risk factors.
Distributions of incident reductions in eGFR and incident CKD across the quartile of non-HDL-C
The distribution of incident eGFR decline ≥30 % significantly increased across the quartiles of serum non-HDL-C levels [first quartile (<111 mg/dL), 7.5 %; second quartile (111–134 mg/dL), 9.8 %; third quartile (135–164 mg/dL), 13.5 %; and fourth quartile (>165 mg/dL), 14.4 % (p value for trend = 0.0359)] (Fig. 2). The distribution of incident CKD also increased across the quartiles of serum non-HDL-C levels [first quartile, 7.9 %; second quartile, 9.9 %; third quartile, 13.4 %; and fourth quartile, 20.6 % (trend p = 0.0011)] (Fig. 3).
Increasing distribution of incident eGFR decline ≥30 % by quartiles of serum non-HDL-C levels. The figure demonstrates that the proportion of incident eGFR decline ≥30 % significantly increased across the quartiles of non-HDL-C [first quartile (<111 mg/dL), 7.5 %; second quartile (111–134 mg/dL), 9.8 %; third quartile (135–164 mg/dL), 13.5 %; and fourth quartile (>165 mg/dL), 14.4 % (trend p = 0.0359)]
Increasing distribution of incident CKD by quartiles of serum non-HDL-C levels. The figure shows that the distribution of incident CKD significantly increased across the quartiles of non HDL-C [first quartile (<111 mg/dL), 7.9 %; second quartile (111–134 mg/dL), 9.9 %; third quartile (135–164 mg/dL), 13.4 %; and fourth quartile (>165 mg/dL), 20.6 % (trend p = 0.0011)]
Discussion
Renal function decreased rapidly over time, and the prevalence of CKD increased by 2.5-fold during the 6-year follow-up period in the HIV-infected cohort. The presence of higher non-HDL-C levels was one of the significant factors associated with reductions in eGFR. These results suggest that increased non-HDL-C levels may facilitate the progression of CKD in HIV-infected individuals.
The annual rate of decline in eGFR was markedly greater in the HIV-infected patients than in the general population. Previous studies reported that this value ranged from 0.34 to 1.1 ml/min/1.73 m2/year in the non-HIV-infected population: 1.1 ml/min/1.73 m2/year (non-DM men without CKD [22]), 0.50 ml/min/1.73 m2/year (the general population younger than 69 years [23]), and 0.34 ± 0.02 ml/min/1.73 m2/year (the general Japanese population in the 40–49 years group [24]). On the other hand, the annual rate of decline in eGFR among HIV-infected patients ranged from 1.5 to 9.2 ml/min/1.73 m2/year: 2.6 ml/min/1.73 m2/year (the San Francisco-based Study of the Consequences of the Protease Inhibitor Era [25]), 9.2 ml/min/1.73 m2/year (a subset of African Americans [26]) and 1.5 ml/min/1.73 m2/year (a subset of white Caucasians [26]). The annual rate of decline in eGFR may vary among races, and the present result of 2.01 ± 0.09 ml/min/1.73 m2/year based on the Japanese HIV-infected patients appears to be similar to the value obtained for white Caucasians. Therefore, annual decreases in renal function may occur more rapidly, by 2-fold or more, in HIV-infected patients than in the general population.
The present study showed that the incidence of CKD was 13.2 % (72 out of 544 HIV-infected non-CKD patients with eGFR ≥ 60 ml/min/1.73 m2) during the 6-year follow-up period, and thus that the prevalence of CKD increased by 2.5-fold from the initiation of the study (from 8.5 to 21.7 %). The incidence of CKD in our study appears to have been higher than previous findings from Western countries. Flandre et al. showed that 349 out of 7378 HIV-infected patients (4.7 %) developed incident CKD in 4 years (median) [27]. Lucas et al. reported that 210 out of 4185 HIV-infected subjects (5.0 %) developed incident CKD during the average follow-up period of 4.5 years [28]. Although the reason why our value was almost 2-fold higher than those previously reported has not yet been determined, the relatively small patient number, high proportion of cART use, ethnic homogeneity, and longer follow-up period may have been involved. Incidentally, HIV-infected patients are more likely to progress to end-stage renal disease (ESRD) than non-infected patients because the estimated incidences of ESRD in the US and Europe in HIV-infected subjects are 3–10 per 1000 person-years [28, 29] and 0.5 per 1000 person-years [30, 31], respectively. This number is 2 to 20-fold greater than that of the general Japanese population. Accordingly, the higher incidence of ESRD may support our current results that HIV-infected patients are predisposed to rapid declines in renal function.
High non-HDL-C levels were identified as a risk factor for incident reductions in eGFR in the HIV-infected cohort. The mechanisms by which elevated non-HDL-C levels induce renal dysfunction remain unclear. Lipids per se may have direct toxicity towards glomerular tissues. Joles et al. reported that hypercholesterolemia and hypertriglyceridemia were both associated with prominent podocyte injury, proteinuria, and interstitial injury in ovariectomized albuminemic female rats [32]. As described previously in the Introduction section, non-HDL-C may be more than just a marker of atherogenicity. For example, some studies showed that non-HDL-C levels were relevant to the progression of renal insufficiency, urinary albumin excretion, and cerebro-cardiovascular disease [17, 18]. Moreover, the assessment of renal pathology at autopsy in HIV-infected CKD patients in Komagome Hosipital suggested that HIV-infected patients were predisposed to renal arteriosclerosis. Indeed, those who had elevated non-HDL-C levels were at a higher risk of advanced global glomerulosclerosis with intra-renal arteriosclerosis than those who did not, and there were no other convincing histological changes to explain the cause of CKD (unpublished data). These results prompted us to speculate that elevations in non-HDL-C levels may be linked to the progression of renal dysfunction by facilitating the process of intra-renal arteriosclerosis. The results of the present study suggest that early treatments to decrease non-HDL-C levels could be useful for HIV-infected patients from the viewpoint of renal safety.
Our study identified being female, albuminuria (UACR ≥ 30 mg/g) at baseline, and CD 4 < 200 cells/μL at baseline as risk factors for decreased eGFR. Previous studies have emphasized the clinical significance of these factors for kidney diseases in HIV-infected patients. For example, the Data on Adverse Drugs (D:A:D) study, based on 18,055 HIV-positive persons, indicated that being female and a lower CD4 nadir (CD 4 < 200 cells/μL), as well as an older age, intravenous drug use, a HCV-positive antibody status, lower baseline eGFR, HT, DM, and a previous history of cardiovascular disease need to be included in the risk score for CKD [33]. Of these risk factors, the early detection of mild albuminuria may be of the most importance for renal safety because even middle (UACR 10–19 mg/g) to high levels (UACR 20–29 mg/g) within the normal range of albuminuria have been identified as significant risks for the near-term development of overt kidney disease [34]. Furthermore, albuminuria, if identified at an early stage, is treatable by the strict control of blood pressure and blood sugar levels using inhibitors of the renin-angiotensin-aldosterone system [35].
Although precise mechanism is unclear, some previous reports showed that HIV-infected women may tend to have renal insults [5, 26, 36]. In fact, being women has the same weight in the D:A:D risk score for CKD as well as HCV positive antibody status, lower CD4 nadir, prior CVD, and HT [33]. A relatively lower muscle mass of women compared to men may be associated with a misestimation of eGFR by the MDRD equation, and differences in muscle mass between men and women might be lower in HIV-infected population because of their frequent sarcopenia [37]. The correction coefficient of the eGFR calculation for women, e.g., ×0.739, may be greater for HIV-infected women.
There was a significant relation between a decrease in eGFR and CD4 cell count <200 in this study. Some of prior studies [26, 38–40] have shown the association between renal dysfunction and lower CD4 cell counts in the HIV-infected population. In general, HIV-infected patients who never reached the infection control target, such as CD cell count >400 and undetected level of HIV-RNA titer, often have a long-term duration of HIV infection, cumulative exposure to cART and nephrotoxic drugs, such as NSAID, antifungal agents and antibiotics, and several comorbidities including DM, HT and DL. These may be concurrently responsible for the association between renal function and CD cell count.
TDF, ATV, and IDV, which are generally regarded as agents that cause nephrotoxicity [5–8, 41, 42], were not associated with decreased eGFR in this study. Since specialists for HIV medical care are very familiar with the nephrotoxicity caused by these drugs, they may avoid giving these agents to CKD patients or rapidly stop their administration with the emergence of mild renal impairments. In addition, DM was not significantly involved even though it was identified as significant in the univariate analysis. This may have been due to multicollinearity between UACR and DM because DM became a significant factor for decreased eGFR [OR, 2.43 (1.07–5.33)] when UACR ≥ 30 mg/g was excluded from the multivariate analysis.
There were several limitations to this study. Since this was a single center study on a cohort including relatively young Japanese patients who lived in an urban area, generalizability is limited to such individuals. We could not conduct a renal biopsy study to explore the cause(s) of incident CKD. Contemporary HIV-infected patients are exposed to various risk factors for kidney diseases: traditional risk factors, such as DM and HT, the use of nephrotoxic drugs including antiretroviral agents, which may cause tubulointerstitial nephritis, and co-infections with hepatitis B and C, which may cause immune-associated kidney diseases. Therefore, the accumulation of renal biopsy findings at the occurrence of renal impairments is warranted in order to confirm pathological characteristics and clarify more precise cause(s) of CKD in HIV-infected subjects.
In conclusion, the prevalence of CKD increased by approximately 2.5-fold in 6 years as eGFR rapidly decreased over time in HIV-infected patients receiving cART. In addition to known risk factors, elevated non-HDL-C levels may be a risk factor linked with rapid declines in renal function.
References
Yanagisawa N, Ando M, Ajisawa A, Imamura A, Suganuma A, Tsuchiya K, Nitta K. Clinical characteristics of kidney disease in Japanese HIV-infected patients. Nephron Clin Pract. 2011;118:c285–91.
Wyatt CM, Winston JA, Malvestutto CD, Fishbein DA, Barash I, Cohen AJ, Klotman ME, Klotman PE. Chronic kidney disease in HIV infection: an urban epidemic. AIDS. 2007;21:2101–3.
Fernando SK, Finkelstein FO, Moore BA, Weissman S. Prevalence of chronic kidney disease in an urban HIV infected population. Am J Med Sci. 2008;335:89–94.
Cheung CY, Wong KM, Lee MP, Liu YL, Kwok H, Chung R, Chau KF, Li CK, Li CS. Prevalence of chronic kidney disease in Chinese HIV-infected patients. Nephrol Dial Transplant. 2007;22:3186–90.
Mocroft A, Kirk O, Reiss P, De Wit S, Sedlacek D, Beniowski M, Gatell J, Phillips AN, Ledergerber B, Lundgren JD, EuroSIDA Study Group. Estimated glomerular filtration rate, chronic kidney disease and antiretroviral drug use in HIV-positive patients. AIDS. 2010;24:1667–78.
Mocroft A, Lundgren J, Ross M, Law M, Reiss P, Kirk O, Smith C, Wentworth D, Heuhaus J, Fux C, Moranne O, Morlat P, Johnson M, Ryom L, Date on Adverse Events (D:A:D) study group, the Royal Free Hospital Clinic Cohort and the INSIGHT study group. A clinically useful risk-score for chronic kidney disease in HIV infection. J Int AIDS Soc. 2014;17:19514.
Young J, Schafer J, Fux CA, Furrer H, Bernasconi E, Vernazza P, Calmy A, Cavassini M, Weber R, Battegay M, Bucher HC, Swiss HIV Cohort Study. Renal function in patients with HIV starting therapy with tenofovir and either efavirenz, lopinavir or atazanavir. AIDS. 2012;26:567–75.
Horberg M, Tang B, Towner W, Silverberg M, Bersoff-Matcha S, Hurley L, Chang J, Blank J, Quesenberry C Jr, Klein D. Impact of tenofovir on renal function in HIV-infected, antiretroviral-naive patients. J Acquir Immune Defic Syndr. 2010;53:62–9.
Grundy SM. Non-high-density lipoprotein cholesterol level as potential risk predictor and therapy target. Arch Intern Med. 2001;161:1379–80.
Farwell WR, Sesso HD, Buring JE, Gaziano JM. Non-high-density lipoprotein cholesterol versus low-density lipoprotein cholesterol as a risk factor for a first nonfatal myocardial infarction. Am J Cardiol. 2005;96:1129–34.
Cui Y, Blumenthal RS, Flaws JA, Whiteman MK, Langenberg P, Bachorik PS, Bush TL. Non-high-density lipoprotein cholesterol level as a predictor of cardiovascular disease mortality. Arch Intern Med. 2001;161:1413–9.
Liu J, Sempos CT, Donahue RP, Dorn J, Trevisan M, Grundy SM. Non-high-density lipoprotein and very-low-density lipoprotein cholesterol and their risk predictive values in coronary heart disease. Am J Cardiol. 2006;98:1363–8.
Ingelsson E, Schaefer EJ, Contois JH, McNamara JR, Sullivan L, Keyes MJ, Pencina MJ, Schoonmaker C, Wilson PW, D’Agostino RB, Vasan RS. Clinical utility of different lipid measures for prediction of coronary heart disease in men and women. JAMA. 2007;298:776–85.
Noda H, Iso H, Irie F, Sairenchi T, Ohtaka E, Ohta H. Association between non-high-density lipoprotein cholesterol concentrations and mortality from coronary heart disease among Japanese men and women: the Ibaraki Prefectural Health Study. J Atheroscler Thromb. 2010;17:30–6.
Mahajan N, Ference BA, Arora N, Madhavan R, Bhattacharya P, Sudhakar R, Sagar A, Wang Y, Sacks F, Afonso L. Role of non-high-density lipoprotein cholesterol in predicting cerebrovascular events in patients following myocardial infarction. Am J Cardiol. 2012;109:1694–9.
Wu J, Chen S, Liu L, Gao X, Zhou Y, Wang C, Zhang Q, Wang A, Hussain M, Sun B, Wu S, Zhao X. Non-high-density lipoprotein cholesterol vs low-density lipoprotein cholesterol as a risk factor for ischemic stroke: a result from the Kailuan study. Neurol Res. 2013;35:505–11.
Samuelsson O, Mulec H, Knight-Gibson C, Attman PO, Kron B, Larsson R, Weiss L, Wedel H, Alaupovic P. Lipoprotein abnormalities are associated with increased rate of progression of human chronic renal insufficiency. Nephrol Dial Transplant. 1997;12:1908–15.
Pan J, Gao F, Bao Y, Zhang L, Tu Y, Jia W. Non-high-density lipoprotein cholesterol is associated more closely with albuminuria in Chinese type 2 diabetic patients with normal renal function, compared with traditional lipid parameters. J Clin Lipidol. 2012;6:382–7.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators developing the Japanese equation for estimated GFR. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38:963–74.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Hemmelgarn BR, Zhang J, Manns BJ, Tonelli M, Larsen E, Ghali WA, Southern DA, McLaughlin K, Mortis G, Culleton BF. Progression of kidney dysfunction in the community-dwelling elderly. Kidney Int. 2006;69:2155–61.
Eriksen BO, Ingebretsen OC. The progression of chronic kidney disease: a 10-year population-based study of the effects of gender and age. Kidney Int. 2006;69:375–82.
Imai E, Horio M, Yamagata K, Iseki K, Hara S, Ura N, Kiyohara Y, Makino H, Hishida A, Matsuo S. Slower decline of glomerular filtration rate in the Japanese general population: a longitudinal 10-year follow-up study. Hypertens Res. 2008;31:433–41.
Choi AI, Shlipak MG, Hunt PW, Martin JN, Deeks SG. HIV-infected persons continue to lose kidney function despite successful antiretroviral therapy. AIDS. 2009;23:2143–9.
Lucas GM, Lau B, Atta MG, Fine DM, Keruly J, Moore RD. Chronic kidney disease incidence, and progression to end-stage renal disease, in HIV-infected individuals: a tale of two races. J Infect Dis. 2008;197:1548–57.
Flandre P, Pugliese P, Cuzin L, Bagnis CI, Tack I, Cabié A, Poizot-Martin I, Katlama C, Brunet-François C, Yazdanpanah Y, Dellamonica P, New AIDS Data group. Risk factors of chronic kidney disease in HIV-infected patients. Clin J Am Soc Nephrol. 2011;6:1700–7.
Lucas GM, Mehta SH, Atta MG, Kirk GD, Galai N, Vlahov D, Moore RD. End-stage renal disease and chronic kidney disease in a cohort of African-American HIV-infected and at-risk HIV-seronegative participants followed between 1988 and 2004. AIDS. 2007;21:2435–43.
Jotwani V, Li Y, Grunfeld C, Choi AI, Shlipak MG. Risk factors for ESRD in HIV-infected individuals: traditional and HIV-related factors. Am J Kidney Dis. 2012;59:628–35.
Bansi L, Hughes A, Bhagani S, Mackie NE, Leen C, Levy J, Edwards S, Connolly J, Holt SG, Hendry BM, Sabin C, Post FA, UK CHIC/ESRF study group. Clinical epidemiology of HIV-associated end-stage renal failure in the UK. AIDS. 2009;23:2517–21.
Bickel M, Marben W, Betz C, Khaykin P, Stephan C, Gute P, Haberl A, Knecht G, Wolf T, Brodt HR, Geiger H, Herrmann E, Jung O. End-stage renal disease and dialysis in HIV-positive patients: observations from a long-term cohort study with a follow-up of 22 years. HIV Med. 2013;14:127–35.
Joles JA, Kunter U, Janssen U, Kriz W, Rabelink TJ, Koomans HA, Floege J. Early mechanisms of renal injury in hypercholesterolemic or hypertriglyceridemic rats. J Am Soc Nephrol. 2000;11:669–83.
Mocroft A, Lundgren JD, Ross M, Law M, Reiss P, Kirk O, Smith C, Wentworth D, Neuhaus J, Fux CA, Moranne O, Morlat P, Johnson MA, Ryom L, D:A:D study group, Royal Free Hospital Clinic Cohort, INSIGHT study Group, SMART study group, ESPRIT study group. Development and validation of a risk score for chronic kidney disease in HIV infection using prospective cohort data from the D:A:D study. PLoS Med. 2015;12:e1001809.
Ando M, Yanagisawa N, Ajisawa A, Tsuchiya K, Nitta K. Urinary albumin excretion within the normal range is an independent risk for near-term development of kidney disease in HIV-infected patients. Nephrol Dial Transplant. 2011;26:3923–9.
Slinin Y, Ishani A, Rector T, Fitzgerald P, MacDonald R, Tacklind J, Rutks I, Wilt TJ. Management of hyperglycemia, dyslipidemia, and albuminuria in patients with diabetes and CKD: a systematic review for a KDOQI clinical practice guideline. Am J Kidney Dis. 2012;60:747–69.
Tordato F, Cozzi Lepri A, Cicconi P, De Luca A, Antinori A, Colangeli V, Castagna A, Nasta P, Ladisa N, Giacometti A, d’Arminio Monforte A, Gori A, ICONA Foundation Study Group. Evaluation of glomerular filtration rate in HIV-1-infected patients before and after combined antiretroviral therapy exposure. HIV Med. 2011;12:4–13.
Buehring B, Kirchner E, Sun Z, Calabrese L. The frequency of low muscle mass and its overlap with low bone mineral density and lipodystrophy in individuals with HIV–a pilot study using DXA total body composition analysis. J Clin Densitom. 2012;15:224–32.
Abraham AG, Althoff KN, Jing Y, Estrella MM, Kitahata MM, Wester CW, Bosch RJ, Crane H, Eron J, Gill MJ, Horberg MA, Justice AC, Klein M, Mayor AM, Moore RD, Palella FJ, Parikh CR, Silverberg MJ, Golub ET, Jacobson LP, Napravnik S, Lucas GM, North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) of the International Epidemiologic Databases to Evaluate AIDS (IeDEA). End-stage renal disease among HIV-infected adults in North America. Clin Infect Dis. 2015;60:941–9.
Szczech LA, Gupta SK, Habash R, Guasch A, Kalayjian R, Appel R, Fields TA, Svetkey LP, Flanagan KH, Klotman PE, Winston JA. The clinical epidemiology and course of the spectrum of renal diseases associated with HIV infection. Kidney Int. 2004;66:1145–52.
Krawczyk CS, Holmberg SD, Moorman AC, Gardner LI, McGwin G Jr, HIV Outpatient Study Group. Factors associated with chronic renal failure in HIV-infected ambulatory patients. AIDS. 2004;18:2171–8.
Hara M, Suganuma A, Yanagisawa N, Imamura A, Hishima T, Ando M. Atazanavir nephrotoxicity. Clin Kidney J. 2015;8:137–42.
Jao J, Wyatt CM. Antiretroviral medications: adverse effects on the kidney. Adv Chronic Kidney Dis. 2010;17:72–82.
Acknowledgments
We thank Makoto Saito, MSc at the Statistics Division in Tokyo Metropolitan Komagome Hospital for his contribution to the statistical analyses performed in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
About this article
Cite this article
Hara, M., Yanagisawa, N., Ohta, A. et al. Increased non-HDL-C level linked with a rapid rate of renal function decline in HIV-infected patients. Clin Exp Nephrol 21, 275–282 (2017). https://doi.org/10.1007/s10157-016-1281-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-016-1281-9