Abstract
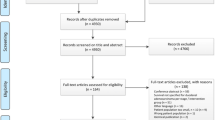
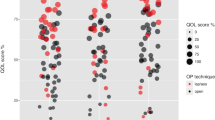
It is well known that surgery is the mainstay treatment for duodenal adenocarcinoma. However, the optimal extent of surgery is still under debate. We aimed to systematically review and perform a meta-analysis of limited resection (LR) and pancreatoduodenectomy for patients with duodenal adenocarcinoma. A systematic electronic database search of the literature was performed using PubMed and the Cochrane Library. All studies comparing LR and pancreatoduodenectomy for patients with duodenal adenocarcinoma were selected. Long-term overall survival was considered as the primary outcome, and perioperative morbidity and mortality as the secondary outcomes. Fifteen studies with a total of 3166 patients were analyzed; 995 and 1498 patients were treated with limited resection and pancreatoduodenectomy, respectively. Eight and 7 studies scored a low and intermediate risk of publication bias, respectively. The LR group had a more favorable result than the pancreatoduodenectomy group in overall morbidity (odd ratio [OR]: 0.33, 95% confidence interval [CI] 0.17–0.65) and postoperative pancreatic fistula (OR: 0.13, 95% CI 0.04–0.43). Mortality (OR: 0.96, 95% CI 0.70–1.33) and overall survival (OR: 0.61, 95% CI 0.33–1.13) were not significantly different between the two groups, although comparison of the two groups stratified by prognostic factors, such as T categories, was not possible due to a lack of detailed data. LR showed long-term outcomes equivalent to those of pancreatoduodenectomy, while the perioperative morbidity rates were lower. LR could be an option for selected duodenal adenocarcinoma patients with appropriate location or depth of invasion, although further studies are required.





Similar content being viewed by others
References
Aparicio T, Zaanan A, Mary F et al (2016) Small Bowel Adenocarcinoma. Gastroenterol Clin North Am 45(3):447–457
Buchbjerg T, Fristrup C, Mortensen MB (2015) The incidence and prognosis of true duodenal carcinomas. Surg Oncol 24(2):110–116
Meijer LL, Alberga AJ, de Bakker JK et al (2018) Outcomes and treatment options for duodenal adenocarcinoma: a systematic review and meta-analysis. Ann Surg Oncol 25(9):2681–2692
Alwmark A, Andersson A, Lasson A (1980) Primary carcinoma of the duodenum. Ann Surg 191(1):13–18
Hu JX, Miao XY, Zhong DW et al (2006) Surgical treatment of primary duodenal adenocarcinoma. Hepatogastroenterology 53(72):858–862
Joesting DR, Beart RW Jr, van Heerden JA et al (1981) Improving survival in adenocarcinoma of the duodenum. Am J Surg 141(2):228–231
Rose DM, Hochwald SN, Klimstra DS et al (1996) Primary duodenal adenocarcinoma: a ten-year experience with 79 patients. J Am Coll Surg 183(2):89–96
Barnes G Jr, Romero L, Hess KR et al (1994) Primary adenocarcinoma of the duodenum: management and survival in 67 patients. Ann Surg Oncol 1(1):73–78
Zhang S, Cui Y, Zhong B et al (2011) Clinicopathological characteristics and survival analysis of primary duodenal cancers: a 14-year experience in a tertiary centre in South China. Int J Colorectal Dis 26(2):219–226
Chung WC, Paik CN, Jung SH et al (2011) Prognostic factors associated with survival in patients with primary duodenal adenocarcinoma. Korean J Intern Med 26(1):34–40
Santoro E, Sacchi M, Scutari F et al (1997) Primary adenocarcinoma of the duodenum: treatment and survival in 89 patients. Hepatogastroenterology 44(16):1157–1163
Sohn TA, Lillemoe KD, Cameron JL et al (1998) Adenocarcinoma of the duodenum: factors influencing long-term survival. J Gastrointest Surg 2(1):79–87
Bakaeen FG, Murr MM, Sarr MG et al (2000) What prognostic factors are important in duodenal adenocarcinoma? Arch Surg. 135(6):635–641 ((discussion 41-2))
Kaklamanos IG, Bathe OF, Franceschi D et al (2000) Extent of resection in the management of duodenal adenocarcinoma. Am J Surg 179(1):37–41
Tocchi A, Mazzoni G, Puma F et al (2003) Adenocarcinoma of the third and fourth portions of the duodenum: results of surgical treatment. Arch Surg 138(1):80–85
Cecchini S, Correa-Gallego C, Desphande V et al (2012) Superior prognostic importance of perineural invasion vs. lymph node involvement after curative resection of duodenal adenocarcinoma. J Gastrointest Surg. 16(1):113–120 ((discussion 20))
Onkendi EO, Boostrom SY, Sarr MG et al (2012) 15-year experience with surgical treatment of duodenal carcinoma: a comparison of periampullary and extra-ampullary duodenal carcinomas. J Gastrointest Surg 16(4):682–691
Kato Y, Takahashi S, Kinoshita T et al (2014) Surgical procedure depending on the depth of tumor invasion in duodenal cancer. Jpn J Clin Oncol 44(3):224–231
Cloyd JM, Norton JA, Visser BC et al (2015) Does the extent of resection impact survival for duodenal adenocarcinoma? Analysis of 1,611 cases. Ann Surg Oncol 22(2):573–580
Jiang QL, Huang XH, Chen YT et al (2016) Prognostic factors and clinical characteristics of patients with primary duodenal adenocarcinoma: a single-center experience from China. Biomed Res Int 2016:6491049
Lee CHA, Shingler G, Mowbray NG et al (2018) Surgical outcomes for duodenal adenoma and adenocarcinoma: a multicentre study in Australia and the United Kingdom. ANZ J Surg 88(3):E157–E161
Rangelova E, Blomberg J, Ansorge C et al (2015) Pancreas-preserving duodenectomy is a safe alternative to high-risk pancreatoduodenectomy for premalignant duodenal lesions. J Gastrointest Surg 19(3):492–497
Kohga A, Yamamoto Y, Sano S et al (2017) Surgical strategy for T1 duodenal or ampullary carcinoma according to the depth of tumor invasion. Anticancer Res 37(9):5277–5283
DeOliveira ML, Winter JM, Schafer M et al (2006) Assessment of complications after pancreatic surgery: a novel grading system applied to 633 patients undergoing pancreaticoduodenectomy. Ann Surg. 244(6):931–937 ((discussion 7-9))
Perez A, Saltzman JR, Carr-Locke DL et al (2003) Benign nonampullary duodenal neoplasms. J Gastrointest Surg 7(4):536–541
Yan JQ, Peng CH, Yang WP et al (2010) Surgical management of benign duodenal tumours. ANZ J Surg 80(7–8):526–530
Moher D, Liberati A, Tetzlaff J et al (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341
Higgins JP, Altman DG, Gotzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928
Wells G, Shea B, O'Connell D, Peterson j, Welch V, Losos M, et al (2000) The Newcastle–Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis2000.
Zhang RC, Xu XW, Wu D et al (2013) Laparoscopic transduodenal local resection of periampullary neuroendocrine tumor: a case report. World J Gastroenterol 19(39):6693–6698
Poves I, Burdio F, Alonso S et al (2011) Laparoscopic pancreas-sparing subtotal duodenectomy. JOP 12(1):62–65
Cho A, Yamamoto H, Kainuma O et al (2012) Totally laparoscopic pancreas-sparing duodenectomy. Surg Today 42(10):1032–1035
Stauffer JA, Raimondo M, Woodward TA et al (2013) Laparoscopic partial sleeve duodenectomy (PSD) for nonampullary duodenal neoplasms: avoiding a whipple by separating the duodenum from the pancreatic head. Pancreas 42(3):461–466
Konishi M, Kinoshita T, Nakagohri T et al (2007) Pancreas-sparing duodenectomy for duodenal neoplasms including malignancies. Hepatogastroenterology 54(75):753–757
Chung RS, Church JM, vanStolk R (1995) Pancreas-sparing duodenectomy: indications, surgical technique, and results. Surgery 117(3):254–259
Huttner FJ, Fitzmaurice C, Schwarzer G et al (2016) Pylorus-preserving pancreaticoduodenectomy (pp Whipple) versus pancreaticoduodenectomy (classic Whipple) for surgical treatment of periampullary and pancreatic carcinoma. Cochrane Database Syst Rev. 2:CD006053
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Bassi C, Dervenis C, Butturini G et al (2005) Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138(1):8–13
Wente MN, Bassi C, Dervenis C et al (2007) Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 142(5):761–768
Wente MN, Veit JA, Bassi C et al (2007) Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 142(1):20–25
Poultsides GA, Huang LC, Cameron JL et al (2012) Duodenal adenocarcinoma: clinicopathologic analysis and implications for treatment. Ann Surg Oncol 19(6):1928–1935
Kim MJ, Choi SB, Han HJ et al (2014) Clinicopathological analysis and survival outcome of duodenal adenocarcinoma. Kaohsiung J Med Sci 30(5):254–259
Lee HG, You DD, Paik KY et al (2008) Prognostic factors for primary duodenal adenocarcinoma. World J Surg 32(10):2246–2252
Liang TJ, Wang BW, Liu SI et al (2012) Number of involved lymph nodes is important in the prediction of prognosis for primary duodenal adenocarcinoma. J Chin Med Assoc 75(11):573–580
Sarela AI, Brennan MF, Karpeh MS et al (2004) Adenocarcinoma of the duodenum: importance of accurate lymph node staging and similarity in outcome to gastric cancer. Ann Surg Oncol 11(4):380–386
Hurtuk MG, Devata S, Brown KM et al (2007) Should all patients with duodenal adenocarcinoma be considered for aggressive surgical resection? Am J Surg. 193(3):319–324 ((discussion 24-5))
Solaini L, Jamieson NB, Metcalfe M et al (2015) Outcome after surgical resection for duodenal adenocarcinoma in the UK. Br J Surg 102(6):676–681
Rotman N, Pezet D, Fagniez PL et al (1994) Adenocarcinoma of the duodenum: factors influencing survival. French Association for Surgical Research. Br J Surg. 81(1):83–85
Struck A, Howard T, Chiorean EG et al (2009) Non-ampullary duodenal adenocarcinoma: factors important for relapse and survival. J Surg Oncol 100(2):144–148
Ryder NM, Ko CY, Hines OJ et al (2000) Primary duodenal adenocarcinoma: a 40-year experience. Arch Surg. 135(9):1070–1074 ((discussion 4-5))
Moss WM, McCart PM, Juler G et al (1974) Primary adenocarcinoma of the duodenum. Arch Surg 108(6):805–807
Jones BA, Langer B, Taylor BR et al (1985) Periampullary tumors: which ones should be resected? Am J Surg 149(1):46–52
Ouriel K, Adams JT (1984) Adenocarcinoma of the small intestine. Am J Surg 147(1):66–71
Cortese AF, Cornell GN (1972) Carcinoma of the duodenum. Cancer 29(4):1010–1015
Lowell JA, Rossi RL, Munson JL et al (1992) Primary adenocarcinoma of third and fourth portions of duodenum. Favorable prognosis after resection. Arch Surg 127(5):557–560
Lai EC, Doty JE, Irving C et al (1988) Primary adenocarcinoma of the duodenum: analysis of survival. World J Surg 12(5):695–699
Malleo G, Tonsi A, Marchegiani G et al (2013) Postoperative morbidity is an additional prognostic factor after potentially curative pancreaticoduodenectomy for primary duodenal adenocarcinoma. Langenb Arch Surg 398(2):287–294
Sakamoto T, Saiura A, Ono Y et al (2017) Optimal lymphadenectomy for duodenal adenocarcinoma: does the number alone matter? Ann Surg Oncol 24(11):3368–3377
Acknowledgements
We would like to thank the Japan Duodenal Cancer Guideline Committee and many doctors related to this research opportunity. Japan Duodenal Cancer Guideline Committee: S. N. Souya Nunobe, S. K. Shingo Kanaji, H. E. Hidetoshi Eguchi, K. O. Ken-ichi Okada, T. F. Tsutomu Fujii, Y. N. Yuichi Nagakawa, K. K. Kengo Kanetaka, H. Y. Hiroharu Yamashita, S. Y. Suguru Yamada, S. K.Shinji Kuroda, T. A. Toru Aoyama, T. A. Takahiro Akahori, K. N. Kenji Nakagawa, R. H. Ryota Higuchi, H. Y. Hiroki Yamaue, M. S. Masayuki Sho, Y. K. Yasuhiro Kodera.
Funding
This work was supported by the Health and Labor Sciences Research Grant (Grant number H29-GANTAISAKU-IPPAN-013) and JSPS KAKENHI (Grant number 18K08632). The funders had no role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Consortia
Contributions
Study conception and design of study: RH. Duodenal Guidelines Committee, Surgery Group: SN, SK, HE, KO, TF, YN, KK, HY, SY, SK, TA, TA, KN, RH, HY, MS and YK. Organizing committee meetings and providing opportunities for making article: KO, MS and YK. Acquisition of data: SN, SK, HE, PB and RH. Analysis and interpretation of data: PB. and RH. Drafting of manuscript: PB. and RH. Critical revision of manuscript: SN, SK, HE, MY, KO, MS and YK.
Corresponding author
Ethics declarations
Conflict of interest statement
The authors have no conflicts of interest to declare.
Ethical approval
The authors have no ethical conflicts to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The members of the Japan Duodenal Cancer Guideline Committee are mentioned in “Acknowledgements” section
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Burasakarn, P., Higuchi, R., Nunobe, S. et al. Limited resection vs. pancreaticoduodenectomy for primary duodenal adenocarcinoma: a systematic review and meta-analysis. Int J Clin Oncol 26, 450–460 (2021). https://doi.org/10.1007/s10147-020-01840-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01840-5