Abstract
Background
Gravitational valves (GVs) prevent overdrainage in ventriculoperitoneal shunting (VPS). However, there are no data available on the appropriate opening pressure in the shunt system when implementing a GV. We performed a retrospective analysis of hydrocephalic patients who were successfully treated with VPS which included one or more GV.
Method
In this retrospective study in adult VPS patients with GVs, we analysed all available data, including the most recent computed tomography (CT) scans, to determine the best adjustments for alleviating any symptoms of overdrainage and underdrainage. Vertical effective opening pressure (VEOP) of the entire shunt system, including the differential pressure valve, was determined.
Results
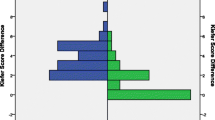
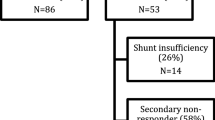
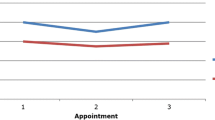
One hundred and twenty-two patients were eligible for the study. Of these, female patients revealed a higher VEOP compared with males (mean, 35.6 cmH2O [SD ± 2.46] vs 28.9 cmH2O [SD ± 0.87], respectively, p = 0.0072, t-test). In patients older than 60 years, lower VEOPs, by a mean of 6.76 cmH2O ± 2.37 (p = 0.0051), were necessary. Mean VEOP was found to be high in idiopathic intracranial hypertension (IIH; 41.6 cmH2O) and malresorptive and congenital HC (35.9 and 36.3), but low in normal pressure HC (27.5, p = 0.0229; one-way ANOVA). In the total cohort, body mass index (BMI) and height did not correlate with VEOP. Twelve patients required a VEOP of more than 40 cmH2O, and in eight of these patients this was accomplished by using multiple GVs. All but one of these eight patients were of female gender, and none of the latter were treated for normal pressure hydrocephalus (NPH) (p = 0.0044 and p = 0.0032, Fisher’s exact test).
Conclusions
In adult VPS patients, female gender increases the risk of overdrainage requiring higher VEOPs. Initial implantation of adjustable GV should be considered in female patients treated with VP shunts for pathology other than NPH.



Similar content being viewed by others
References
Allin DM, Czosnyka ZH, Czosnyka M, Richards HK, Pickard JD (2006) In vitro hydrodynamic properties of the Miethke ProGAV hydrocephalus shunt. Cerebrospinal Fluid Res 3:9
Bergsneider M, Miller C, Vespa PM, Hu X (2008) Surgical management of adult hydrocephalus. Neurosurgery 62(Suppl 2):643–660
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzer HA, Avezaat CJ, de Jong DA, Gooskens RH, Hermans J (1998) Dutch normal-pressure hydrocephalus study: randomized comparison of low- and medium-pressure shunts. J Neurosurg 88:490–495
Bouchard C, Despres JP, Mauriege P (1993) Genetic and nongenetic determinants of regional fat distribution. Endocr Rev 14:72–93
Browd SR, Gottfried ON, Ragel BT, Kestle JR (2006) Failure of cerebrospinal fluid shunts: part II: overdrainage, loculation, and abdominal complications. Pediatr Neurol 34:171–176
Buxton N, Punt J (1999) Subtemporal decompression: the treatment of noncompliant ventricle syndrome. Neurosurgery 44:513–519
Chowdhury B, Kvist H, Andersson B, Bjorntorp P, Sjostrom L (1993) CT-determined changes in adipose tissue distribution during a small weight reduction in obese males. Int J Obes Relat Metab Disord 17:685–691
Czosnyka M, Czosnyka Z, Pickard JD (2012) Programmable shunt assistant tested in Cambridge shunt evaluation laboratory. Acta Neurochir (Wein) 113:71–76
Davis SE, Levy ML, McComb JG, Sposto R (2000) The delta valve: how does its clinical performance compare with two other pressure differential valves without antisiphon control? Ped Neurosurg 33:58–63
Enzi G, Gasparo M, Biondetti PR, Fiore D, Semisa M, Zurlo F (1986) Subcutaneous and visceral fat distribution according to sex, age, and overweight, evaluated by computed tomography. Am J Clin Nutr 44:739–746
Freimann FB, Kimura T, Stockhammer F, Schulz M, Rohde V, Thomale UW (2014) In vitro performance and principles of anti-siphoning devices. Acta Neurochir (Wien) 156:2191–2199
Freimann FB, Luhdo ML, Rohde V, Vajkoczy P, Wolf S, Sprung C (2014) The Frankfurt horizontal plane as a reference for the implantation of gravitational units: a series of 376 adult patients. Acta Neurochir (Wien) 156:1351–1356
Freimann FB, Sprung C (2012) Shunting with gravitational valves—can adjustments end the era of revisions for overdrainage-related events? J Neurosurg 117:1197–1204
Freimann FB, Vajkoczy P, Sprung C (2013) Patients benefit from low-pressure settings enabled by gravitational valves in normal pressure hydrocephalus. Clin Neurol Neurosurg 115:1982–1986
Gebert AF, Schulz M, Haberl H, Thomale UW (2013) Adjustments in gravitational valves for the treatment of childhood hydrocephalus—a retrospective survey. Childs Nerv Syst 29:2019–2025
Kaestner S, Kruschat T, Nitzsche N, Deinsberger W (2009) Gravitational shunt units may cause under-drainage in bedridden patients. Acta Neurochir (Wien) 151:217–221
Kehler U, Kiefer M, Eymann R, Wagner W, Tschan CA, Langer N, Rohde V, Ludwig HC, Gliemroth J, Meier U, Lemcke J, Thomale UW, Fritsch M, Krauss JK, Mirzayan MJ, Schuhmann M, Huthmann A (2015) PROSAIKA: a prospective multicenter registry with the first programmable gravitational device for hydrocephalus shunting. Clin Neurol Neurosurg 137:132–136
Kiefer M, Antes S, Leonhardt S, Schmitt M, Orakcioglu B, Sakowitz OW, Eymann R (2012) Telemetric ICP measurement with the first CE-approved device: data from animal experiments and initial clinical experiences. Acta Neurochir (Wein) 114:111–116
Kurtom KH, Magram G (2007) Siphon regulatory devices: their role in the treatment of hydrocephalus. Neurosurg Focus 22:E5
Lemcke J, Meier U, Muller C, Fritsch MJ, Kehler U, Langer N, Kiefer M, Eymann R, Schuhmann MU, Speil A, Weber F, Remenez V, Rohde V, Ludwig HC, Stengel D (2013) Safety and efficacy of gravitational shunt valves in patients with idiopathic normal pressure hydrocephalus: a pragmatic, randomised, open label, multicentre trial (SVASONA). J Neurol Neurosurg Psychiatry 84:850–857
Lemieux S, Prud’homme D, Bouchard C, Tremblay A, Despres JP (1993) Sex differences in the relation of visceral adipose tissue accumulation to total body fatness. Am J Clin Nutr 58:463–467
Liniger P, Marchand S, Kaiser GL (2003) Flow control versus antisiphon valves: late results concerning slit ventricles and slit-ventricle syndrome. Eur J Pediatr Surg 13(Suppl 1):S3–S6
Meier U, Stengel D, Müller C, Fritsch MJ, Kehler U, Langer N, Kiefer M, Eymann R, Schuhmann M, Speil A, Weber F, Remenez V, Rohde V, Ludwig H, Lemcke J (2013) Predictors of subsequent over-drainage and clinical outcomes after ventriculo-peritoneal shunting for idiopathic normal pressure hydrocephalus. Neurosurgery 73:1054–1060
Park J, Kim GJ, Hwang SK (2007) Valve inclination influences the performance of gravity-assisted valve. Surg Neurol 68:14–18
Stockhammer F, Miethke C, Knitter T, Rohde V, Sprung C (2013) Flow-related noise in patients with ventriculoperitoneal shunt using gravitational adjustable valves. Acta Neurochir (Wien) 156:761–765
Tschan CA, Antes S, Huthmann A, Vulcu S, Oertel J, Wagner W (2014) Overcoming CSF overdrainage with the adjustable gravitational valve proSA. Acta Neurochir (Wien) 156:767–776
Wajchenberg BL (2000) Subcutaneous and visceral adipose tissue: their relation to the metabolic syndrome. Endocr Rev 21:697–738
Acknowledgments
We would like to thank to Bawarjan Schatlo for helpful comments for preparing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript. F.F., C.C., V.R. and F.S. received speaker fees from Braun-Äskulap/Miethke. C.C. received a price endowed by Braun-Äskulap/Miethke
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Additional information
Comments
In this retrospective study of hydrocephalic patients who were treated with a ventriculoperitoneal shunt (VPS) system that included gravitational valves (GV) to prevent overdrainage, the authors introduce a new parameter, the Vertical Effective Opening. Pressure (VEOP). This was calculated as the combined pressure of all valves in the shunt system that is needed to prevent overdrainage and still give a satisfactory CSF drainage. Not so unexpected, the VEOP differed significantly depending on the type of hydrocephalus, with idiopathic intracranial hypertension requiring the highest pressure and normal pressure hydrocephalus the lowest. More interesting is the finding that the female gender appears to require a higher pressure than males to avoid overdrainage. In the authors’ analyses, this gender difference was however found only in the group of patients with high Body Mass Index (BMI); in patients with normal or subnormal BMI, this difference failed to reach statistical significance.
This study may give some valuable advice when it comes to planning of VPS implantation in adults; the authors themselves conclude: “initial implantation of adjustable GVs should be considered in female patients treated with VP shunts for pathology other than NPH”.
As with all new observations, the findings presented here should however be viewed with precaution until verified by another, preferably prospective, study.
Knut Wester
Bergen, Norway
Rights and permissions
About this article
Cite this article
Diesner, N., Freimann, F., Clajus, C. et al. Female gender predisposes for cerebrospinal fluid overdrainage in ventriculoperitoneal shunting. Acta Neurochir 158, 1273–1278 (2016). https://doi.org/10.1007/s00701-016-2827-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2827-z