Abstract
Elderly patients with severe hematological malignancies may require cardiac surgery. The combined impact of cardiopulmonary bypass (CPB) and surgical trauma is a potent inflammatory activator and is increased by intraoperative and postoperative complications. To avoid the adverse effects of CPB, minimally invasive off-pump techniques may be used in these patients. The transapical off-pump mitral valve intervention with NeoChord implantation (TOP-MINI) is a minimally invasive technique for mitral valve repair, which makes it possible to avoid the risks of CPB in selected patients, such as elderly, cancer or immunosuppressive patients. We report here the case of a 78-year-old male with B-cell non-Hodgkin’s lymphoma, who presented with severe mitral regurgitation. The patient was successfully treated with the TOP-MINI procedure.
Similar content being viewed by others
Patients with a history of hematological malignancies are considered high-risk candidates for cardiac surgery, and represent only 0.38 % of all patients undergoing cardiac surgery [1]. For selected patients undergoing curative treatment for a malignancy, or who are in remission, cardiac surgery is not contraindicated, but patients who have had prior treatment for cancer are at particular risk for cardiac surgery complications such as bleeding and increased susceptibility to infection due to leukopenia [2]. Various derangements in the immune system have been described in association with cardiopulmonary bypass (CPB) [3].
The transapical off-pump mitral valve intervention with NeoChord implantation (TOP-MINI) is a minimally invasive technique which is performed under 2D/3D transesophageal echocardiography (TEE) guidance and is used on selected patients as a safe and effective alternative to open surgical repair in patients with mitral leaflet prolapse, flail, or chordae rupture [4, 5]. The case reported here is of severe mitral regurgitation (MR) due to bileaflet mitral valve (MV) disease, which was treated with the TOP-MINI procedure in a patient with non-Hodgkin’s lymphoma (NHL).
Case report
A 78-year-old male with NHL was admitted to our hospital with the complaint of breathlessness on minor exertion [New York Heart Association (NYHA) class III]. The anamnesis revealed hypertension and B-cell NHL, which had been diagnosed 3 years earlier. Chemo-radiotherapy had been terminated 6 months previously because of old age and comorbidity.
Transthoracic echocardiography (TTE) and TEE showed a severe MR with posterior leaflet prolapse (eccentric jet) (Fig. 1) [left ventricular end diastolic diameter (LVEDD) 46 mm, left ventricular end systolic diameter (LVESD) 30 mm, left ventricular ejection fraction (LVEF) 65 %, left atrial diameter (LAD) 50 mm]. Coronary angiography showed normal coronaries.
In the operating room, standard monitoring included invasive blood pressure, five-lead electrocardiography, pulse oximetry, end-tidal CO2, bispectral index, diuresis and body core temperature. External defibrillating pads were applied before the surgical drape placement. Left sided ultrasound-assisted thoracic paravertebral block (TPVB) was applied at T3–T6 levels before induction of anesthesia. After TPVB, the patient was placed in a supine position with the left upper trunk elevated. After the induction of anesthesia, the patient was tracheally intubated with a 37 F right-sided double-lumen endotracheal tube. Anesthesia was maintained with 50 % air and 5–6 % desflurane in oxygen with positive pressure ventilation in a circle system. Before the thoracotomy was performed, one lung ventilation (OLV) was initiated and ventilator settings were adjusted to keep peak pressure below 25 cmH2O.
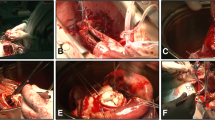
A left anterolateral mini-thoracotomy was performed in the 5th intercostal space. A dose of 100 IU/kg heparin was given to achieve an activated clotting time of at least 300 s. The NeoChord DS1000 (NeoChord, Inc., Eden Praire, MN) device which was loaded with expanded polytetrafluoroethylene (ePTFE) suture was pushed forward towards the MV under 2D X-plane imaging [mid-esophageal long-axis (ME LAX) and mitral commissure (MC) views] (Fig. 2) TEE guidance through an apical ventriculotomy. After the device was inserted through the MV into the left atrium, the echocardiographic imaging was switched to full online 3D and the device was shifted towards the prolapsing segment under 3D TEE imaging (Fig. 3). The prolapsing segment of the posterior leaflet was grasped with the instrument’s jaws, and was confirmed on the 4-fiberoptic monitor when the lights turned from red to white. The neochord was implanted and the device was retracted. Under 2D ME LAX TEE color Doppler, the neochord was properly tensioned to achieve a correct MV function (Fig. 4). A total of 3 neochords were implanted in the same way.
During the procedure, the central venous pressure was maintained above 10 mmHg with crystalloids or colloids and the mean arterial pressure was maintained above 60 mmHg. A cell-saver was used for continuous auto-transfusion for efficient blood salvage and 620 ml of blood was salvaged. Homologous blood transfusion and inotropic support was not used during the procedure. Sudden hemodynamic deterioration and serious arrhythmias were not observed during the procedure. The procedural time was 140 min (skin to skin) and no complication occurred.
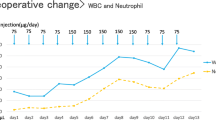
After surgery, the patient was transferred to the intensive care unit (ICU).
The patient was transferred from ICU to the cardiovascular surgery ward at the postoperative 20th h and was discharged on the postoperative 5th day.
Discussion
Malignancies of the hematopoietic system such as chronic lymphocytic leukemia and lymphoma mainly affect elderly patients. Similarly, the incidence of cardiac disease is increased in elderly patients. For example, the prevalence of MR increases from 2.4 % in patients aged 60–69 years to 11.2 % in patients aged 70–83 years [6]. The operative risk of patients with malignant hematological disorders is increased, as this may include coagulation defects, changes in blood viscosity, immune suppression and bone marrow insufficiency [7]. Surgical trauma and CPB have the potential risk of increasing hematological problems because the immune systems in these patients are depressed [8]. There have been limited studies about the influence of hematopoietic disorders and their treatment on the results of cardiac surgery. In a study by Sommer et al. of 56 patients, it was indicated that the results of cardiac surgery in patients with a history of a malignant hematologic disorder were acceptable but a higher complication and mortality rate could be expected [9]. Guler et al. reported that cardiac surgery in patients with hematological malignancies could be performed with acceptable early postoperative outcomes [10]. Similar results were also stated in studies by Fecher and Potapov [1, 11]. Kucukarslan et al. prospectively compared 98 patients who had undergone coronary artery bypass surgery (CABG) with malignancy in remission and without any malignancy and reported that CABG in patients with comorbid malignancy was as safe as in other patients [12].
Avoidance of CPB in cardiac surgery with the use of off-pump techniques may reduce some of the risks. Brandon et al. reported that the off-pump coronary artery bypass (OPCAB) strategy was safe and reliable in very high-risk patients, reducing multi-organ failure [13].
The advantages of TOP-MINI are the avoidance of sternotomy and the risks of CPB, in addition to improved patient satisfaction and cosmesis. After a left anterolateral mini-thoracotomy, the apex of the left ventricle is gently palpated with a finger to determine the access site under 2D TEE monitoring multiplane imaging (X-plane) at 0° and 90°. A NeoChord DS1000 device loaded with ePTFE suture is inserted in the left ventricle (LV) and advanced towards the flailing segment of the prolapsed MV leaflet under the X-plane imaging (ME LAX and MC views). After the device is inserted through the MV into the left atrium, the device is shifted towards the prolapsing segment under 3D transechocardiographic imaging. The flailing segment is grasped by the jaws of the device, a neochord is implanted and the device is removed from the heart. The neochord is tensioned until MR is significantly reduced under 2D TEE imaging color Doppler. The correct amount of stretched neochord is fixed by passing a pledget over the ventriculotomy. If an additional neochord is required, the procedure is repeated [14]. Although no long-term results of the TOP-MINI procedure have been published, the early results have been seen to be favorable [15, 16].
The TOP-MINI procedure necessitates complex anesthetic management. 2D and 3D TEE guidance is used in all stages (device insertion, leaflet grasping, tension, evaluation of result) of the procedure. OLV, fluid administration, avoidance of hypothermia and pain management are the basis for anesthetic management [17].
During the entire procedure, the anesthesiologist must be prepared for sudden hemodynamic deterioration, which may require blood transfusion, inotropic support or emergency CPB. When the device enters the LV through the transapical ventriculotomy, excessive blood leakage may occur if the apical purse-strings are not tightened well, and this results in hemodynamic deterioration. A plastic pocket is attached under the site of the skin incision to collect blood loss. Excessive blood loss is gathered by a cell-saver system.
Arrhythmias occur due to movement of the device inside the heart and they are usually temporary. Serious arrhythmias such as ventricular fibrillation may be observed during the procedure. Because the small incision of the thoracotomy limits the use of internal cardiac defibrillation paddles, external defibrillator pads must be applied before the surgical drape placement.
In conclusion, hematological malignancies such as chronic lymphocytic leukemia and lymphoma with cardiac surgery are commonly seen in elderly patients. The use of minimally invasive techniques can be attempted to avoid the undesirable impact of CPB in these patients. TOP-MINI can be used as an alternative method in this patient group.
References
Fecher AM, Birdas TJ, Haybron D, Papasavas PK, Evers D, Caushaj PF. Cardiac operations in patients with hematologic malignancies. Eur J Cardiothorac Surg. 2004;25:537–40.
Chan J, Rosenfeldt F, Chaudhuri K, Marasco S. Cardiac surgery in patients with a history of malignancy: increased complication rate but similar mortality. Heart Lung Circ. 2012;21:255–9.
Holmannova D, Kolackova M, Mandak J, Kunes P, Holubcova Z, Krejsek J, Vlaskova D, Andrys C. Inhibitory CD200R and proapoptotic CD95/CD95L molecules on innate immunity cells are modulated by cardiac surgery. Perfusion. 2015;30:543–55.
Rucinskas K, Janusauskas V, Zakarkaite D, Aidietiene S, Samalavicius R, Speziali G, Aidietis A. Off-pump transapical implantation of artificial chordae to correct mitral regurgitation: early results of a single-center experience. J Thorac Cardiovasc Surg. 2014;147:95–9.
Colli A, Manzan E, Rucinskas K, Janusauskas V, Zucchetta F, Zakarkaitė D, Aidietis A, Gerosa G. Acute safety and efficacy of the NeoChord procedure. Interact Cardiovasc Thorac Surg. 2015;20:575–80 (discussion 580–1).
Singh JP, Evans JC, Levy D, Larson MG, Freed LA, Fuller DL, Lehman B, Benjamin EJ. Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (The Framingham Heart Study). Am J Cardiol. 1999;83:897–902.
Christiansen S, Schmid C, Löher A, Scheld HH. Impact of malignant hematological disorders on cardiac surgery. Cardiovasc Surg. 2000;8:149–52.
Borde D, Gandhe U, Hargave N, Pandey K. Management of patients with hematological malignancies undergoing coronary artery bypass grafting. Ann Cardiac Anaesth. 2013;16:47–50.
Sommer SP, Lange V, Yildirim C, Schimmer C, Aleksic I, Wagner C, Schuster C, Leyh RG. Cardiac surgery and hematologic malignancies: a retrospective single-center analysis of 56 consecutive patients. Eur J Cardiothorac Surg. 2011;40:173–8.
Guler A, Sahin MA, Cingoz F, Ozal E, Demirkilic U, Arslan M. Can cardiac surgery be performed safely on patients with haematological malignancies. Cardiovasc J Afr. 2012;23:194–6.
Potapov EV, Zurbrügg HR, Herzke C, Srock S, Riess H, Sodian R, Hübler S, Hetzer R. Impact of cardiac surgery using cardiopulmonary bypass on course of chronic lymphatic leukemia: a case-control study. Ann Thorac Surg. 2002;74:384–9.
Kucukarslan N, Tatar T, Uzun M, Yavuz I, Ozal E, Tatar H. Coronary artery bypass surgery in patients with malignancy: a single-center study with comparison to patients without malignancy. J Card Surg. 2009;24:151–5.
Barandon L, Richebé P, Munos E, Calderon J, Lafitte M, Lafitte S, Couffinhal T, Roques X. Off-pump coronary artery bypass surgery in very high-risk patients: adjustment and preliminary results. Interact CardioVasc Thorac Surg. 2008;7:789–93.
Colli A, Zucchetta F, Torregrossa G, Manzan E, Bizzotto E, Besola L, Bellu R, Sarais C, Pittarello D, Gerosa G. Transapical off-pump mitral valve repair with NeoChord implantation (TOP-MINI): step-by-step guide. Ann Cardiothorac Surg. 2015;4:295–7.
Rucinskas K, Janusauskas V, Zakarkaite D. Off-pump transapical implantation of artificial chordae to correct mitral regurgitation: early results of a single-center experience. J Thorac Cardiovasc Surg. 2014;147:95–9.
Colli A, Manzan E, Zucchetta F. Transapical off-pump mitral valve repair with NeoChord implantation: early clinical results. Int J Cardiol. 2016;204:23–8.
Kavakli AS, Kavrut Ozturk N, Ayoglu RU, Emmiler M, Ozyurek L, Inanoglu K, Ozmen S. Anesthetic management of transapical off-pump mitral valve repair with NeoChord implantation. J Cardiothorac Vasc Anesth (in press).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors of this manuscript have a conflict of interest to declare.
Funding
Departmental resources were used.
About this article
Cite this article
Kavakli, A.S., Ayoglu, R.U., Kavrut Ozturk, N. et al. Mitral valve repair facilitated with transapical beating heart NeoChord implantation in a non-Hodgkin’s lymphoma patient. J Anesth 30, 1056–1059 (2016). https://doi.org/10.1007/s00540-016-2251-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-016-2251-9