Abstract
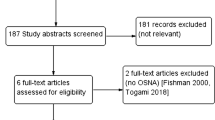
Sentinel lymph node (SN) biopsy is part of the staging procedure in breast cancer patients. In this study, we compared an intraoperative tool named one-step nucleic acid amplification (OSNA) to our routine histological investigation. OSNA consists of a short homogenization step followed by amplification of cytokeratin (CK) 19 mRNA directly from the lysate. To evaluate the performance of OSNA in comparison to histology, analysis of 343 axillary lymph nodes (ALN) from 93 breast cancer patients was performed with both methods. Discordant samples were subjected to other methods. If these tests supported the OSNA results, these samples were excluded from the study. The concordance rate was 91.8%, sensitivity 98.1%, and specificity 90.8% before and 95.5%, 100%, and 95.6%, respectively, after discordant case investigation. Our results show that OSNA is an excellent method for the detection of metastases in lymph nodes and can be applied as an intraoperative diagnostic approach.
Similar content being viewed by others
Introduction
The sentinel lymph node (SN) is the first lymph node to receive lymph drainage from the tumor area and is highly predictive for the status of the remaining axillary lymph nodes (ALN) [1]. Since SN biopsy is a minimally invasive technique, it spares the patient from the unpleasant side effects as well as morbidity associated with axillary clearance [2] and has readily evolved into the up-to-date standard staging procedure in clinically node-negative breast cancer patients [3–6].
Intraoperative detection of tumor deposits in SN is conventionally achieved by frozen sections, touch imprints, and cytological smears. In case tumor deposits are detected in the SN, adjuvant ALN dissection (ALND) is directly performed. Unfortunately, these techniques suffer from a rather low sensitivity, and the degree of tumor spread into the lymph nodes is often underestimated [7–10]. If postoperative in-depth histological examination [11] proves to be positive, the patient is subjected to ALND in a second surgery. Besides additional costs and discomfort for the patient associated with a second surgical intervention, the investigation of permanent sections is subject to a variety of protocols with regard to the degree of SN sectioning, staining procedure, and antibody used [12]. In addition, the evaluation of tissue sections by the pathologist might be influenced by a subjective interpretation [13]. As a consequence, there is a need for a standardized and reproducible method with a high predictive value which can be applied intraoperatively.
Molecular methods based on reverse-transcriptase polymerase chain reaction (RT-PCR) were employed for the detection of metastatic deposits in lymph nodes of breast cancer patients [14–16] and indicated usefulness as a molecular staging tool [17] and prognostic factor [18]. Despite these promising investigations, on the condition that nucleic acids have to be isolated beforehand, these assays are too time-consuming for routine diagnosis within a defined time frame.
An intraoperative molecular test system for the detection of metastases in the SN of breast cancer patients was provided and showed a sensitivity of 87.6% and specificity of 94.2%. Discordant results were thought to be partly due to the fact that different tissue sections were used for this molecular assay and histology [19].
A different commercially available, molecular method for intraoperative diagnosis of lymph node metastases in breast cancer patients called one-step nucleic acid amplification (OSNA) was previously presented [20, 21]. The semiautomated OSNA assay (Sysmex, Kobe, Japan) consists of a short sample preparation step and real-time amplification of CK19 mRNA directly from the homogenate, without any RNA purification steps. The time to perform the assay takes 30–40 min for 3–4 LN. This quantitative molecular assessment allows the distinction of the size of the metastasis [20]. Also, in patients with colorectal cancer, the OSNA method with CK19 as a marker in tandem with frozen section histology increased intraoperative sensitivity when compared to frozen sections alone [22].
The aim of this study was to find out whether the performance of the OSNA assay was comparable to extensive histologic work-up: staining with hematoxylin and eosin (H&E) as well as a pan-cytokeratin antibody. Accordingly, 343 ALN from 93 German breast cancer patients were investigated with both approaches.
Material and methods
Patient samples
ALN samples, 343, from 93 breast cancer patients were included in this study. Patient characteristics are presented in Table 1. They were derived from complete axillary dissection which had been performed due to a previously positive SN or a clinically positive lymph node. The specimens were collected at the two participating German institutes in this study, University Clinic of Schleswig-Holstein in Kiel, and the Albertinen Hospital in Hamburg, Germany. The 93 patients were fully informed about the study and had given written consent before surgery in compliance with the regulations of the local ethical committees of the University of Kiel and Albertinen Hospital.
Study design
The 343 lymph node samples were longitudinally cut into four nearly equal slices (a, b, c, d) with a special cutting tool consisting of three blades being either 1 or 2 mm apart, as depicted elsewhere [20]. ALN were categorized into groups according to their size: ALN with a minor axis smaller than 0.4 cm were excluded from the study; lymph nodes with a minor axis between 0.4 and 0.6 cm (group 1) were centrally cut into four slices with the 1–mm cutting tool; ALN between 0.6 and 1.0 cm (group 2) were centrally cut into four slices with a 2-mm cutting tool. Lymph nodes with a minor axis larger than 1.0 cm (group 3) were either halved or cut into several pieces, and each piece, depending on its size, was treated in a similar fashion as described for groups 1 and 2. Alternate slices were allocated to the OSNA method (a&c) and to histological work-up (b&d) at five levels. The slices used for OSNA (a&c) were shock frozen in liquid nitrogen and stored at −80°C before the analysis. Histological analysis was performed for slices b&d as outlined in a different section. Concordance and sensitivity were determined based on the comparison of these two methods in 343 ALN samples. All histological investigations were done without knowing the results of the OSNA method and vice versa. The first 120 histologically negative out of the 343 lymph node samples, as determined by five-level histology, were cut into further levels until no remnants remained. Specificity was calculated based on the extended investigation of these 120 samples in order to avoid sampling errors caused by uninvestigated material.
If discordant results between the OSNA assay and five-level histological examination occurred, the histological work-up of these cases was also extended until no tissue remained in the paraffin blocks. In addition, the homogenates of these discordant cases were also analysed by Western Blot and quantitative RT-PCR (QRT-PCR) as depicted in a different section. Provided that these supplemental analyses gave the same result as the OSNA assay, these samples were excluded from the study cohort because an uneven distribution of the metastases within pieces a, b, c, and d (tissue allocation bias) was likely to be the case.
One-step nucleic acid amplification
OSNA with CK19 mRNA as the marker was previously described in-depth [20]. In short, the lymph node slices a&c were homogenized together in 4 ml of homogenizing buffer Lynorhag, pH 3.5, (Sysmex, Kobe, Japan) on ice. Twenty microliters of this homogenate were further used for automated amplification of CK19 mRNA via reverse transcription loop-mediated isothermal amplification (RT-LAMP) [23]. Real-time amplification was accomplished with the Lynoamp Kit (Sysmex, Kobe, Japan) on the RD-100i (Sysmex, Kobe, Japan). Four lymph nodes can be analyzed in one run. The degree of amplification was detected via a by-product of the reaction, pyrophosphate [24]. The resulting change in turbidity, upon precipitation of magnesium pyrophosphate, was in turn correlated to CK19 mRNA copy number/μL of the original lysate via a standard curve which was established beforehand with three calibrators containing different CK19 mRNA copy numbers. Since no isolation or purification of RNA was required for OSNA, results were available after a total of 30–40 min. The lymph node lysates were stored at −80°C until further use.
If the CK19 mRNA copy number/μL lysate was less than 250 copies/μL, the result was regarded as (−); copy numbers between 250 and 5,000/μL were regarded as (+), and copy numbers larger than 5,000/μL as (++).
Histologic work-up
Lymph node slices b&d were fixed with neutral buffered formaldehyde and embedded in the same paraffin block. Each slice was identified by color coding.
Two initial H&E sections (representing frozen sections of SN), one initial level, and four additional levels with a 0.1-mm skip space were cut from the 343 blocks. Each level consisted of four 4 μm sections: one was used for H&E staining, one for immunohistochemistry (IHC) with the pan anticytokeratin antibody LU5 (T-1302, Dianova, Germany), one for CK19 IHC (M0888, clone RCK 108, DAKO, Germany), and one spare section. For the specificity study, the paraffin blocks of 120 histologically negative samples, as judged by five-level histological work-up, were cut into further levels until no remnants remained. IHC was performed according to a standard protocol. Shortly, deparaffinised sections were cooked in a pressure cooker in Tris–ethylenediaminetetraacetic acid–sodium citrate buffer, pH 7.8, for 4 min. After blocking, incubation with the primary antibody was performed for 40 min and with the secondary antibody for 30 min. Visualization was done with diaminobenzidine tetrahydrochloride (Vector, Burlingame, CA, USA). Staining with the LU5 antibody was done using the NEXES staining automat and the I-View-Kit (Ventana, Illkirch, France).
Metastatic deposits were recorded, according to the TNM classification of UICC 6th and AJCC 6th edition [25, 26] as isolated tumor cells (ITC) if their largest diameter was smaller than 0.2 mm, as micrometastases if they were larger than 0.2 mm but not larger than 2 mm in diameter, and as macrometastases if they were larger than 2 mm in diameter. In concordance with the TNM designation of ITC as pN0(i+), lymph node samples were only regarded as positive if at least one micrometastasis or macrometastasis was found. Consequently, lymph nodes with ITC were considered as negative in this study.
Western Blot as part of discordant case investigation
Twenty microliters of the homogenate of discordant specimens were analyzed by Western Blot for CK19. The procedure was recently described in detail [20]. In short, the lysate was mixed with 10 μL loading buffer containing 150 mM Tris–HCl, 300 mM dithiothreitol, 6% sodium dodecyl sulfate (SDS), 0.3% bromophenol blue, and 30% glycerol. The solution was boiled and subjected to electrophoresis on a 7% (w/v) polyacrylamide gel in the presence of SDS (PAG Mini; Daiichi Pure Chemicals, Tokyo, Japan). Proteins were transferred to an Immobilon-FL polyvinylidene fluoride (PVDF) membrane (Millipore, Billierica, MA, USA). After the blocking procedure, the blot was incubated with the primary anticytokeratin 19 antibody A53-B/A2 (Santa Cruz Biotechnology, Santa Cruz, CA, USA) and developed with the ECL-Advance detection kit (GE Healthcare, Chalfont St. Giles, UK). CK19 protein concentrations of the lysate, as expressed in nanograms per microliter of the original lysate, were determined on the basis of a previously performed standard curve created with four calibrators of known CK19 protein concentration (Biodesign, Saco, ME). The cutoff value for CK19 protein expression of 0.13 ng/μL (mean + 3 standard deviations = SD) was assigned as previously presented [20].
QRT-PCR as part of DCI
Total RNA was extracted with the RNeasy Mini Kit (QIAGEN, Valencia, CA, USA) from 200 μL of each discordant sample lysate. The quality of the isolated RNA was controlled by performing QRT-PCR of the housekeeping gene beta-actin. QRT-PCR was carried out with CK19 and two breast cancer-specific markers, SPDEF (SAM pointed domain containing ETS transcription factor), and FOXA1 (forkhead box A1).
QRT-PCR was performed on the ABI Prism 7700 detector in duplicates (Applied Biosystems, Foster City, CA, USA). Two microliters of RNA was subjected to one-step QRT-PCR with QuantiTest SYBR Green (QIAGEN, Hilden, Germany) as described by the manufacturer. Primer sequences for CK19, SPDEF, FOXA1, and beta-actin amplification are listed elsewhere [20, 21].
The cutoff levels for each marker as expressed in threshold cycles (ct) were assigned in reference to data obtained with several histologically negative and positive lymph nodes, respectively. The cutoff levels were as follows: 24 for beta-actin, 31.5 for CK19, 33.8 for FOXA1, and 31.6 for SPDEF.
Results
OSNA versus histology
In this study, 343 ALN samples from 93 breast cancer patients were investigated by both OSNA and histological methods (Table 2). Two hundred eleven samples were negative with both methods, including two samples with ITC. One hundred four samples gave positive results with both assays. Samples, 97 out of 104, contained a macrometastasis, with 90 of them expressing more than 5,000 CK19 mRNA copies/μL (++) (Fig. 1) and seven between 250 and 5,000 CK19 mRNA copies/μL (+). Seven lymph node specimens with a histologically detectable micrometastasis displayed a (++) OSNA result; however, a direct correlation between metastasis size and copy number is not possible since different tissue slices were investigated by each method. H&E staining and immunostaining exhibited concordant results except in three cases which contained a H&E positive micrometastasis or a macrometastasis of 7 or 8 mm, and only weak or no LU5 /CK19 IHC. Remarkably, all these samples gave (++) results in OSNA.
Histologically negative samples (a), micrometastases (b), and macrometastases (c; top) are correlated to CK19 mRNA copy number/μL (bottom). The rise time, which is defined as the time point when the turbidity reached 0.1, is related to CK19 mRNA copy number via a standard curve which was performed beforehand with three calibrators
In one sample containing a 2-mm micrometastasis and one sample with a micrometastasis present in only one level, negative values in the slices used for OSNA were observed. On the other hand, 26 histology negative samples, including one with ITC, yielded a positive result in the OSNA assay. Eleven of these 26 samples had rather low CK19 mRNA copy numbers/μL (250–750 copies/μL; Table 3).
These findings, without taking any data from additional discordant case investigation (DCI) into account, resulted in a concordance rate of 91.8% and sensitivity of 98.1%. The specificity rate of 91.7% was based on the investigation of 120 histologically negative samples, in which the usual five levels plus all additional levels available were analyzed by histology.
Discordant case investigation
RNA and proteins were extracted from the lysates of the 28 discordant cases, followed by QRT-PCR for beta-actin, CK19, FOXA1, and SPDEF as well as Western Blotting for CK19. If the data obtained by those additional analyses were consistent with the results obtained by OSNA, it was concluded that tumor deposits were either only present in slices b or d used for histology or in slices a or c used for OSNA. As a consequence, these samples were excluded from the sample cohort because, in all likelihood, a tissue allocation bias (TAB) had occurred (Table 3).
The two histology positive/OSNA negative samples gave negative results in both QRT-PCR and Western blot (Table 3). In 11 of the 26 histology negative/OSNA positive samples, the outcome of additional analyses indicated the presence of tumor deposits in the slices a or c used for OSNA. When these 13 samples with discordant results between histology and OSNA were not taken into account anymore, the concordance rate changed to 95.5% (315 out of 330) and sensitivity to 100% (104 out of 104). The specificity accounted for 96.5% (109 out of 114) because discordant samples 2, 8, 10, 15, 18, and 25 were part of the specificity study.
Interestingly, more than one OSNA positive/histology negative sample originated from the same patient: samples 1 and 15; samples 7, 13, and 17; samples 22–24; as well as samples 18 and 20 came from one patient, respectively, suggesting the presence of tumor cells in the lymph nodes of these patients.
Discussion
Recently, several studies have addressed the intraoperative use of molecular methods to detect metastatic deposits in SN of breast cancer patients, with varying degree of success. The GeneSearch breast lymph node (BLN) assay which uses CK19 in combination with mammaglobin as targets for RT-PCR gave concordance rates of 92.3% [19, 27] with an inferior performance at detecting micrometastases, as 57% sensitivity were reported. The concordance rates of the OSNA method as determined in two studies were 98.2% [20] and 94.8% [21]. Whereas the BLN assay gave negative or positive results based on ct, the results of OSNA were categorized into (++), (+), as well as (−), and further described by a display of CK19 mRNA copy number as a quantitative information.
In this study, the OSNA performance versus five-level histology (H&E staining, IHC with LU5) was evaluated in 343 ALN from 93 German breast cancer patients. The concordance rate was 91.7%, sensitivity 98.1%, and specificity 90.8%. Since alternate slices of the LN were used for OSNA and histology, it is self-evident that in some events, tumor deposits might be confined to the slices analyzed by OSNA or to the slices used for histology (TAB). In fact, it was recently shown that most discrepancies obtained from analysis of SN by histological and molecular approaches arise from the use of alternate slices for each method [28]. In order to clarify if some of the discordant results obtained in this study occurred as a consequence of this TAB, the homogenates of these lymph node samples were subjected to DCI by RT-PCR and Western blotting. In both of the OSNA negative/histology positive and 11 out of 26 OSNA positive/histology negative samples, DCI revealed equivalent results to the ones seen in the OSNA assay. When these specimens were removed from the sample cohort, the concordance rate was 95.5%, sensitivity 100%, and specificity 95.6%. It cannot be fully excluded that even a higher proportion of discordant results were due to TAB because the homogenates were exposed to long storage and transport conditions which might have lowered the concentration and quality of RNA and proteins. This is especially true for OSNA samples with copy numbers close to the cutoff level as QRT-PCR, and Western blot investigation is then also likely to be close to the detection limit.
By taking the study design into consideration, it is quite apparent that in the OSNA assay, the whole of slices a&c was analyzed, whereas multiple 100 μm skip ribbons of the slices used for histology were left uninvestigated, a concept which is inherently indicative of OSNA positive/histology negative results. At the same time, since this protocol reflects the real situation in its best-case scenario with regard to routine histological investigation of sentinel nodes, the advantage of OSNA is at hand. Even more small metastases might have been missed if the lymph nodes had been cut in 500 μm intervals because the German guidelines recommend two to three sections between 100 and 500 μm [29]. Eleven out of the 26 OSNA positive/histology negative had CK19 mRNA copy numbers/μL below 1,000. With 250 copies/μL as the cutoff level, these positive OSNA results very likely indicate a low tumor burden in the lymph nodes which was probably absent in the tissue sections used for histological investigation.
It was reported that almost all (98.2%) breast cancer tumors express CK19 [30]. The results obtained in the present study support this notion, since OSNA based on CK19 mRNA expression detected all metastases which were reported by histology, after correcting the results for TAB. One must keep in mind that these numbers dealing with CK19 expression in breast cancer tumors are based on protein but not mRNA expression. In one OSNA-positive specimen, H&E staining revealed a macrometastases (8 mm in diameter). This metastasis exhibited a very weak reaction with LU5 and no reaction with the CK19 antibody. This example shows that low CK19 protein expression is no compelling evidence for low CK19 mRNA expression. Except this one case, all H&E-positive samples were also positive with CK19 IHC.
In summary, the OSNA assay based on CK19 mRNA expression proved to be a reliable and standardized tool for the intraoperative detection of lymph node metastases in breast cancer patients. Since OSNA showed a similar performance to in-depth histological analyses routinely performed in SN of German breast cancer patients, its adoption as a clinical approach could lead to a benefit for the patients in that unnecessary second surgeries are avoided, and diagnosis is improved.
References
Morton DL, Wen DR, Wong JH et al (1992) Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg 127:392–399
Golshan M, Martin WJ, Dowlatshahi K et al (2003) Sentinel lymph node biopsy lowers the rate of lymphedema when compared with standard axillary lymph node dissection. Am Surg 69:209–211
Veronesi U, Paganelli G, Viale G et al (1999) Sentinel lymph node biopsy and axillary dissection in breast cancer: results in a large series. J Natl Cancer Inst 91:368–373
Lyman GH, Giuliano AE, Somerfield MR et al (2005) American Society of Clinical Oncology guideline recommendations for sentinel lymph node biopsy in early-stage breast cancer. J Clin Oncol 23:7703–7720
Ferrari A, Rovera F, Dionigi P et al (2006) Sentinel lymph node biopsy as the new standard of care in the surgical treatment for breast cancer. Expert Rev Anticancer Ther 6:1503–1515
Mabry H, Giuliano AE (2007) Sentinel node mapping for breast cancer: progress to date and prospects for the future. Surg Oncol Clin N Am 16:55–70
Motomura K, Inaji H, Komoike Y et al (2000) Intraoperative sentinel lymph node examination by imprint cytology and frozen sectioning during breast surgery. Br J Surg 87:597–601
Creager AJ, Geisinger KR, Shiver SA et al (2002) Intraoperative evaluation of sentinel lymph nodes for metastatic breast carcinoma by imprint cytology. Mod Pathol 15:1140–1147
Leidenius MH, Krogerus LA, Toivonen TS et al (2003) The feasibility of intraoperative diagnosis of sentinel lymph node metastases in breast cancer. J Surg Oncol 84:68–73
Brogi E, Torres-Matundan E, Tan LK et al (2005) The results of frozen section, touch preparation, and cytological smear are comparable for intraoperative examination of sentinel lymph nodes: a study in 133 breast cancer patients. Ann Surg Oncol 12:173–180
Cserni G, Amendoeira I, Apostolikas N et al (2003) Pathological work-up of sentinel lymph nodes in breast cancer. Review of current data to be considered for the formulation of guidelines. Eur J Cancer 39:1654–1667
Cserni G, Amendoeira I, Apostolikas N et al (2004) Discrepancies in current practice of pathological evaluation of sentinel lymph nodes in breast cancer. Results of a questionnaire based survey by the European Working Group for Breast Screening Pathology. J Clin Pathol 57:695–701
Roberts CA, Beitsch PD, Litz CE et al (2003) Interpretive disparity among pathologists in breast sentinel lymph node evaluation. Am J Surg 186:324–329
Mitas M, Mikhitarian K, Walters C et al (2001) Quantitative real-time RT-PCR detection of breast cancer micrometastases using a multigene marker panel. Int J Cancer 93:162–171
Weigelt B, Verduijn P, Bosma AJ et al (2004) Detection of metastases in sentinel lymph nodes of breast cancer patients by multiple mRNA markers. Br J Cancer 90:1531–1537
Nissan A, Jager D, Roystacher M et al (2004) Multimarker RT-PCR assay for the detection of minimal residual disease in sentinel lymph nodes of breast cancer patients. Br J Cancer 94:681–685
Gimbergues P, Dauplat MM, Cayre A et al (2007) Correlation between molecular metastases in sentinel lymph nodes of breast cancer patients and St Gallen risk category. Eur J Surg Oncol 33:16–22
Gillanders WE, Mikhitarian K, Hebert R et al (2004) Molecular detection of micrometastatic breast cancer in histopathology-negative axillary lymph nodes correlates with traditional predictors of prognosis: an interim analysis of a prospective multi-institutional cohort study. Ann Sur 239:828–837, discussion 837–840
Julian TB, Blumencranz P, Deck K et al (2008) Novel intraoperative molecular test for sentinel lymph node metastases in patients with early-stage breast cancer. J Clin Oncol 26:3338–3345
Tsujimoto M, Nakabayashi K, Yoshidome K et al (2007) One-Step Nucleic Acid Amplification (OSNA) for intraoperative detection of lymph node metastasis in breast cancer patients. Clin Can Res 13:4807–4816
Visser M, Jiwa M, Horstman A et al (2008) Intra-operative rapid diagnostic method based on CK19 mRNA expression for the detection of lymph node metastases in breast cancer. Int J Cancer 122:2562–2567
Taniyama K, Motoshita J, Sakane J et al (2006) Combination analysis of a whole lymph node by one-step nucleic acid amplification and histology for intraoperative detection of micrometastasis. Pathobiology 73:183–191
Notomi T, Okayama H, Masubuchi H et al (2000) Loop-mediated isothermal amplification of DNA. Nucleic Acids Research 28:e63
Mori Y, Nagamine K, Tomita N et al (2001) Detection of loop-mediated isothermal amplification reaction by turbidity derived from magnesium pyrophosphate formation. Biochem Biophys Res Commun 289:150–154
Sobin LH, Wittekind C et al (2002) UICC TNM classification of malignant tumours, 6th edn. John Wiley & Sons, Inc., New York
Singletary SE, Greene FL (2003) Revision of breast cancer staging: the 6th edition of the TNM classification. Semin Surg Oncol 21:53–59
Blumencranz P, Whitworth PW, Deck K et al (2007) Sentinel node staging for breast cancer: intraoperative molecular pathology overcomes conventional histologic sampling errors. Am J Surg 194:426–432
Daniele L, Annaratone L, Allia E et al (2008) Technical limits of comparison of step-sectioning, immunohistochemistry and RT-PCR on breast cancer sentinel nodes: a study on methacarn fixed tissue. J Cell Mol Med (in press)
Kreienberg R, Kopp I, Albert U et al (2008) Interdisciplinary S3-Guideline for breast cancer diagnostic procedures, therapy and follow-up. (article in German) W. Zuckschwerdt Verlag 1. Aktualisierung 02/2008, ISBN: 978-3-88603-934-0
Chu PG, Weiss LM (2002) Keratin expression in human tissues and neoplasms. Histopathology 40:403–439
Acknowledgements
The authors want to thank Sunna Frank, Anja Bredtmann, Maike Pacena, and Silvia Holz for their contribution in coordinating the study and their technical assistance.
This study was supported by Sysmex (Kobe, Japan).
Conflict of interest statement
We declare that we have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Schem, C., Maass, N., Bauerschlag, D.O. et al. One-step nucleic acid amplification—a molecular method for the detection of lymph node metastases in breast cancer patients; results of the German study group. Virchows Arch 454, 203–210 (2009). https://doi.org/10.1007/s00428-008-0703-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-008-0703-9