Abstract
Background
An appropriate timing for surgical resection of branch duct-type intraductal papillary mucinous neoplasm (BD-IPMN) to achieve sufficient postoperative survival is still unknown.
Methods
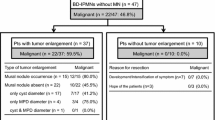
Of 80 patients with histologically proven IPMNs, 61 patients who had BD-IPMN without pancreatic cancer concomitant with IPMN were enrolled in this study. We divided BD-IPMN into four groups according to disease progression: low to intermediate grade of dysplasia (LGD/IGD-IPMN), high grade of dysplasia (HGD-IPMN), minimally invasive IPMN (MI-IPMN: T1a), and invasive IPMN (IN-IPMN: ≥T1b). Indicators of surgical resection were investigated on the basis of pathological findings and postoperative prognosis.
Results
Postoperative survival was distinctly worse for patients with IN-IPMN than for patients with MI-IPMN, HGD-IPMN, and LGD/IGD-IPMN. Postoperative disease-specific 5-year survival rate was 100 % in patients with IN-IPMN, HGD-IPMN, and LGD/IGD-IPMN, by contrast, 40 % in patients with IN-IPMN. The presence of two of the three factors (pancreatitis, serum carbohydrate antigen [CA] 19-9 levels >13 U/mL, and mural nodules) could distinguish HGD-IPMN from LGD/IGD-IPMN with a sensitivity of 92.9 %, specificity of 90.2 %, positive predictive value of 76.5 %, negative predictive value of 97.4 %, and accuracy of 90.9 %.
Conclusions
To manage patients with BD-IPMN and achieve a good postoperative prognosis, surgical resection should be performed before progression to IN-IPMN.


Similar content being viewed by others
References
Hruban RH, Takaori K, Klimstra DS, Adsay NV, Albores-Saavedra J, Biankin AV, Biankin SA, Compton C, Fukushima N, Furukawa T, Goggins M, Kato Y, Kloppel G, Longnecker DS, Luttges J, Maitra A, Offerhaus GJ, Shimizu M, Yonezawa S (2004) An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol 28(8):977–987
Fernandez-del Castillo C, Adsay NV (2010) Intraductal papillary mucinous neoplasms of the pancreas. Gastroenterology 139(3):708–713. doi:10.1053/j.gastro.2010.07.025, 713 e701-702
Tanaka M, Fernandez-del Castillo C, Adsay V, Chari S, Falconi M, Jang JY, Kimura W, Levy P, Pitman MB, Schmidt CM, Shimizu M, Wolfgang CL, Yamaguchi K, Yamao K, International Association of P (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 12(3):183–197. doi:10.1016/j.pan.2012.04.004
Fritz S, Hackert T, Hinz U, Hartwig W, Buchler MW, Werner J (2011) Role of serum carbohydrate antigen 19-9 and carcinoembryonic antigen in distinguishing between benign and invasive intraductal papillary mucinous neoplasm of the pancreas. Br J Surg 98(1):104–110. doi:10.1002/bjs.7280
Pedrazzoli S, Sperti C, Pasquali C, Bissoli S, Chierichetti F (2011) Comparison of International Consensus Guidelines versus 18-FDG PET in detecting malignancy of intraductal papillary mucinous neoplasms of the pancreas. Ann Surg 254(6):971–976. doi:10.1097/SLA.0b013e3182383137
Ohno E, Itoh A, Kawashima H, Ishikawa T, Matsubara H, Itoh Y, Nakamura Y, Hiramatsu T, Nakamura M, Miyahara R, Ohmiya N, Ishigami M, Katano Y, Goto H, Hirooka Y (2012) Malignant transformation of branch duct-type intraductal papillary mucinous neoplasms of the pancreas based on contrast-enhanced endoscopic ultrasonography morphological changes: focus on malignant transformation of intraductal papillary mucinous neoplasm itself. Pancreas 41(6):855–862. doi:10.1097/MPA.0b013e3182480c44
Lafemina J, Katabi N, Klimstra D, Correa-Gallego C, Gaujoux S, Kingham TP, Dematteo RP, Fong Y, D’Angelica MI, Jarnagin WR, Do RK, Brennan MF, Allen PJ (2013) Malignant progression in IPMN: a cohort analysis of patients initially selected for resection or observation. Ann Surg Oncol 20(2):440–447. doi:10.1245/s10434-012-2702-y
Maire F, Hammel P, Terris B, Paye F, Scoazec JY, Cellier C, Barthet M, O’Toole D, Rufat P, Partensky C, Cuillerier E, Levy P, Belghiti J, Ruszniewski P (2002) Prognosis of malignant intraductal papillary mucinous tumours of the pancreas after surgical resection. Comparison with pancreatic ductal adenocarcinoma. Gut 51(5):717–722
Wada K, Kozarek RA, Traverso LW (2005) Outcomes following resection of invasive and noninvasive intraductal papillary mucinous neoplasms of the pancreas. Am J Surg 189(5):632–636. doi:10.1016/j.amjsurg.2005.01.020, discussion 637
Niedergethmann M, Grutzmann R, Hildenbrand R, Dittert D, Aramin N, Franz M, Dobrowolski F, Post S, Saeger HD (2008) Outcome of invasive and noninvasive intraductal papillary-mucinous neoplasms of the pancreas (IPMN): a 10-year experience. World J Surg 32(10):2253–2260. doi:10.1007/s00268-008-9692-8
Takahashi H, Nakamori S, Nakahira S, Tsujie M, Takahshi Y, Marubashi S, Miyamoto A, Takeda Y, Nagano H, Dono K, Umeshita K, Sakon M, Monden M (2006) Surgical outcomes of noninvasive and minimally invasive intraductal papillary-mucinous neoplasms of the pancreas. Ann Surg Oncol 13(7):955–960. doi:10.1245/ASO.2006.05.043
Nara S, Shimada K, Kosuge T, Kanai Y, Hiraoka N (2008) Minimally invasive intraductal papillary-mucinous carcinoma of the pancreas: clinicopathologic study of 104 intraductal papillary-mucinous neoplasms. Am J Surg Pathol 32(2):243–255. doi:10.1097/PAS.0b013e3181484f1e
Hirono S, Tani M, Kawai M, Okada K, Miyazawa M, Shimizu A, Kitahata Y, Yamaue H (2012) The carcinoembryonic antigen level in pancreatic juice and mural nodule size are predictors of malignancy for branch duct type intraductal papillary mucinous neoplasms of the pancreas. Ann Surg 255(3):517–522. doi:10.1097/SLA.0b013e3182444231
Kim KW, Park SH, Pyo J, Yoon SH, Byun JH, Lee MG, Krajewski KM, Ramaiya NH (2014) Imaging features to distinguish malignant and benign branch-duct type intraductal papillary mucinous neoplasms of the pancreas: a meta-analysis. Ann Surg 259(1):72–81. doi:10.1097/SLA.0b013e31829385f7
Shimizu Y, Yamaue H, Maguchi H, Yamao K, Hirono S, Osanai M, Hijioka S, Hosoda W, Nakamura Y, Shinohara T, Yanagisawa A (2013) Predictors of malignancy in intraductal papillary mucinous neoplasm of the pancreas: analysis of 310 pancreatic resection patients at multiple high-volume centers. Pancreas 42(5):883–888. doi:10.1097/MPA.0b013e31827a7b84
Baiocchi GL, Bertagna F, Gheza F, Grazioli L, Calanducci D, Giubbini R, Portolani N, Giulini SM (2012) Searching for indicators of malignancy in pancreatic intraductal papillary mucinous neoplasms: the value of 18FDG-PET confirmed. Ann Surg Oncol 19(11):3574–3580. doi:10.1245/s10434-012-2234-5
Adsay NV, Merati K, Basturk O, Iacobuzio-Donahue C, Levi E, Cheng JD, Sarkar FH, Hruban RH, Klimstra DS (2004) Pathologically and biologically distinct types of epithelium in intraductal papillary mucinous neoplasms: delineation of an “intestinal” pathway of carcinogenesis in the pancreas. Am J Surg Pathol 28(7):839–848
Levy P, Jouannaud V, O’Toole D, Couvelard A, Vullierme MP, Palazzo L, Aubert A, Ponsot P, Sauvanet A, Maire F, Hentic O, Hammel P, Ruszniewski P (2006) Natural history of intraductal papillary mucinous tumors of the pancreas: actuarial risk of malignancy. Clin Gastroenterol Hepatol Off Clin Pract J Am Gastroenterol Assoc 4(4):460–468. doi:10.1016/j.cgh.2006.01.018
Salvia R, Crippa S, Falconi M, Bassi C, Guarise A, Scarpa A, Pederzoli P (2007) Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut 56(8):1086–1090. doi:10.1136/gut.2006.100628
Maguchi H, Tanno S, Mizuno N, Hanada K, Kobayashi G, Hatori T, Sadakari Y, Yamaguchi T, Tobita K, Doi R, Yanagisawa A, Tanaka M (2011) Natural history of branch duct intraductal papillary mucinous neoplasms of the pancreas: a multicenter study in Japan. Pancreas 40(3):364–370. doi:10.1097/MPA.0b013e31820a5975
Nakata K, Ohuchida K, Aishima S, Sadakari Y, Kayashima T, Miyasaka Y, Nagai E, Mizumoto K, Tanaka M, Tsuneyoshi M, Oda Y (2011) Invasive carcinoma derived from intestinal-type intraductal papillary mucinous neoplasm is associated with minimal invasion, colloid carcinoma, and less invasive behavior, leading to a better prognosis. Pancreas 40(4):581–587. doi:10.1097/MPA.0b013e318214fa86
Akita H, Takeda Y, Hoshino H, Wada H, Kobayashi S, Marubashi S, Eguchi H, Tanemura M, Mori M, Doki Y, Nagano H (2011) Mural nodule in branch duct-type intraductal papillary mucinous neoplasms of the pancreas is a marker of malignant transformation and indication for surgery. Am J Surg 202(2):214–219. doi:10.1016/j.amjsurg.2010.06.020
Ohtsuka T, Kono H, Nagayoshi Y, Mori Y, Tsutsumi K, Sadakari Y, Takahata S, Morimatsu K, Aishima S, Igarashi H, Ito T, Ishigami K, Nakamura M, Mizumoto K, Tanaka M (2012) An increase in the number of predictive factors augments the likelihood of malignancy in branch duct intraductal papillary mucinous neoplasm of the pancreas. Surgery 151(1):76–83. doi:10.1016/j.surg.2011.07.009
Katz MH, Varadhachary GR, Fleming JB, Wolff RA, Lee JE, Pisters PW, Vauthey JN, Abdalla EK, Sun CC, Wang H, Crane CH, Lee JH, Tamm EP, Abbruzzese JL, Evans DB (2010) Serum CA 19-9 as a marker of resectability and survival in patients with potentially resectable pancreatic cancer treated with neoadjuvant chemoradiation. Ann Surg Oncol 17(7):1794–1801. doi:10.1245/s10434-010-0943-1
Winter JM, Yeo CJ, Brody JR (2013) Diagnostic, prognostic, and predictive biomarkers in pancreatic cancer. J Surg Oncol 107(1):15–22. doi:10.1002/jso.23192
Jones NB, Hatzaras I, George N, Muscarella P, Ellison EC, Melvin WS, Bloomston M (2009) Clinical factors predictive of malignant and premalignant cystic neoplasms of the pancreas: a single institution experience. HPB Off J Int Hepato Pancreato Biliary Assoc 11(8):664–670. doi:10.1111/j.1477-2574.2009.00114.x
Ingkakul T, Sadakari Y, Ienaga J, Satoh N, Takahata S, Tanaka M (2010) Predictors of the presence of concomitant invasive ductal carcinoma in intraductal papillary mucinous neoplasm of the pancreas. Ann Surg 251(1):70–75. doi:10.1097/SLA.0b013e3181c5ddc3
Kanno A, Satoh K, Hirota M, Hamada S, Umino J, Itoh H, Masamune A, Asakura T, Shimosegawa T (2010) Prediction of invasive carcinoma in branch type intraductal papillary mucinous neoplasms of the pancreas. J Gastroenterol 45(9):952–959. doi:10.1007/s00535-010-0238-0
Conflicts of interest
The authors state that they have no conflicts of interest and that they received no financial or material support.
Authors’ contributions
Hiroshi Kurahara: study conception and design and drafting of manuscript. Kosei Maemura, Yuko Mataki, and Yuko Kijima: acquisition of data. Masahiko Sakoda, Satoshi Iino, and Shinichi Ueno: analysis and interpretation of data. Sumiya Ishigami, Hiroyuki Shinchi, and Shoji Natsugoe: critical revision of manuscript.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 39 kb)
Rights and permissions
About this article
Cite this article
Kurahara, H., Maemura, K., Mataki, Y. et al. Predictors of early stages of histological progression of branch duct IPMN. Langenbecks Arch Surg 400, 49–56 (2015). https://doi.org/10.1007/s00423-014-1259-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-014-1259-6