Abstract
Background
There are many reports about limited surgery for intraductal papillary mucinous neoplasms (IPMNs) of the pancreas. However, there is no consensus on limited surgery for IPMNs. The primary objective of this study was to define the clinical indications for limited surgery for IPMNs.
Methods
The data of 98 patients who underwent curative resections for IPMN were retrospectively analyzed. IPMNs were classified into four different pathological grades: low-grade dysplasia (LGD), intermediate-grade dysplasia (IGD), high-grade dysplasia (HGD), and invasive carcinoma (Inv-IPMN). Inv-IPMNs were divided into T1a, T1b, and T1c or over T1c (≥T1c). Based on preoperative radiological findings, IPMNs were stratified into the three groups using the 2012 International Consensus Guidelines: worrisome features, high-risk stigmata (HRS), and others.
Results
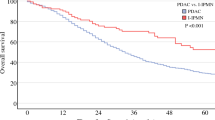
There were no positive lymph node cases and no recurrent cases of LGDs, IGDs, and HGDs. On the other hand, positive lymph node cases in T1a, T1b, and ≥T1c were seen in 37.5, 20, and 22.2% of cases, respectively. The recurrence rates of T1a, T1b, and ≥T1c were 50, 40, and 55.6%, respectively. Of the HRS cases, 30 (73.2%) were malignant and 25 (61%) were Inv-IPMN. HRS showed sensitivity of 92.6%, specificity of 77.5%, and accuracy of 81.6% to identify Inv-IPMN by preoperative imaging.
Conclusions
Limited surgery such as parenchyma-sparing pancreatectomy should be avoided for all cases of Inv-IPMNs, because every Inv-IPMN including T1a has the potential for lymph node metastasis and recurrence. HRS had high preoperative diagnostic ability for predicting Inv-IPMN. For cases that meet HRS criteria, pancreatectomy with lymphadenectomy is needed, and limited surgery should be withheld.



Similar content being viewed by others
References
Maitra A, Fukushima N, Takaori K et al (2005) Precursors to invasive pancreatic cancer. Adv Anat Pathol 12:81–91
Hruban RH, Maitra A, Kern SE et al (2007) Precursors to pancreatic cancer. Gastroenterol Clin North Am 36:831–849
Bosman FT, Carneiro F, Hruban RH, Theise ND (eds) (2010) WHO classification of tumors of Digestive System. International Agency for Research on Cancer, Lyon
Jang JY, Hwang DW, Kim MA et al (2011) Analysis of prognostic factors and a proposed new classification for invasive papillary mucinous neoplasms. Ann Surg Oncol 18:644–650
Yopp AC, Katabi N, Janakos M et al (2011) Invasive carcinoma arising in intraductal papillary mucinous neoplasms of the pancreas: a matched control study with conventional pancreatic ductal adenocarcinoma. Ann Surg 253:968–974
Nara S, Shimada K, Kosuge T et al (2008) Minimally invasive intraductal papillary-mucinous carcinoma of the pancreas: clinicopathologic study of 104 intraductal papillary-mucinous neoplasms. Am J Surg Pathol 32:243–255
Winter JM, Jiang W, Basturk O et al (2016) Recurrence and survival after resection of small intraductal papillary mucinous neoplasm-associated carcinomas (≤20 mm invasive component): a multi-institutional analysis. Ann Surg 263:793–801
Wasif N, Bentrem DJ, Farrell JJ et al (2010) Invasive intraductal papillary mucinous neoplasm versus sporadic pancreatic adenocarcinoma: a stage-matched comparison of outcomes. Cancer 116:3369–3377
Tanaka M, Fernandez-del Castillo C, Adsay V et al (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 12:183–197
Thomas E, Matsuoka L, Alexopoulos S et al (2015) Laparoscopic hand-assisted parenchymal-sparing resections for presumed side-branch intraductal papillary mucinous neoplasms. J Laparoendosc Adv Surg Tech A 25:668–671
Fernandez-Cruz L, Cosa R, Blanco L et al (2007) Curative laparoscopic resection for pancreatic neoplasms: a critical analysis from a single institution. J Gastrointest Surg 11:1607–1621 (discussion 1621–1602)
Sauvanet A, Gaujoux S, Blanc B et al (2014) Parenchyma-sparing pancreatectomy for presumed noninvasive intraductal papillary mucinous neoplasms of the pancreas. Ann Surg 260:364–371
Schwarz L, Fleming J, Katz M et al (2016) Total laparoscopic central pancreatectomy with pancreaticogastrostomy for high-risk cystic neoplasm. Ann Surg Oncol 23:1035
Tanaka M, Chari S, Adsay V et al (2006) International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 6:17–32
Kim J, Jang KT, Mo Park S et al (2011) Prognostic relevance of pathologic subtypes and minimal invasion in intraductal papillary mucinous neoplasms of the pancreas. Tumour Biol 32:535–542
Abu Hilal M, Richardson JR, de Rooij T et al (2016) Laparoscopic radical ‘no-touch’ left pancreatosplenectomy for pancreatic ductal adenocarcinoma: technique and results. Surg Endosc 30:3830–3838
Sharpe SM, Talamonti MS, Wang E et al (2015) The laparoscopic approach to distal pancreatectomy for ductal adenocarcinoma results in shorter lengths of stay without compromising oncologic outcomes. Am J Surg 209:557–563
Sulpice L, Farges O, Goutte N et al (2015) Laparoscopic distal pancreatectomy for pancreatic ductal adenocarcinoma: Time for a randomized controlled trial? Results of an all-inclusive national observational study. Ann Surg 262:868–873 (discussion 873–864)
Anand N, Sampath K, Wu BU (2013) Cyst features and risk of malignancy in intraductal papillary mucinous neoplasms of the pancreas: a meta-analysis. Clin Gastroenterol Hepatol 11:913–921 (quiz e959–960)
Murakami Y, Uemura K, Hayashidani Y et al (2007) Predictive factors of malignant or invasive intraductal papillary-mucinous neoplasms of the pancreas. J Gastrointest Surg 11:338–344
Shimizu Y, Yamaue H, Maguchi H et al (2013) Predictors of malignancy in intraductal papillary mucinous neoplasm of the pancreas: analysis of 310 pancreatic resection patients at multiple high-volume centers. Pancreas 42:883–888
Kanno A, Satoh K, Hirota M et al (2010) Prediction of invasive carcinoma in branch type intraductal papillary mucinous neoplasms of the pancreas. J Gastroenterol 45:952–959
Roch AM, Ceppa EP, Al-Haddad MA et al (2014) The natural history of main duct-involved, mixed-type intraductal papillary mucinous neoplasm: parameters predictive of progression. Ann Surg 260:680–688 (discussion 688–690)
Ogawa T, Horaguchi J, Fujita N et al (2014) Diffusion-weighted magnetic resonance imaging for evaluating the histological degree of malignancy in patients with intraductal papillary mucinous neoplasm. J Hepatobiliary Pancreat Sci 21:801–808
Pedrazzoli S, Sperti C, Pasquali C et al (2011) Comparison of International Consensus Guidelines versus 18-FDG PET in detecting malignancy of intraductal papillary mucinous neoplasms of the pancreas. Ann Surg 254:971–976
Correa-Gallego C, Do R, Lafemina J et al (2013) Predicting dysplasia and invasive carcinoma in intraductal papillary mucinous neoplasms of the pancreas: development of a preoperative nomogram. Ann Surg Oncol 20:4348–4355
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Kimura, K., Amano, R., Ymazoe, S. et al. The Clinical Indications for Limited Surgery of Intraductal Papillary Mucinous Neoplasms of the Pancreas. World J Surg 41, 1358–1365 (2017). https://doi.org/10.1007/s00268-016-3824-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3824-3