Abstract
Schizophrenia is an incurable and debilitating mental disorder that may affect up to 1 % of the world population. Morphological, electrophysiological, and neurophysiological studies suggest that the corpus callosum (CC), which is the largest portion of white matter in the human brain and responsible for inter-hemispheric communication, is altered in schizophrenia patients. Here, we employed mass spectrometry-based proteomics to investigate the molecular underpinnings of schizophrenia. Brain tissue samples were collected postmortem from nine schizophrenia patients and seven controls at the University of Heidelberg, Germany. Because the CC has a signaling role, we collected cytoplasmic (soluble) proteins and submitted them to nano-liquid chromatography-mass spectrometry (nano LC–MS/MS). Proteomes were quantified by label-free spectral counting. We identified 5678 unique peptides that corresponded to 1636 proteins belonging to 1512 protein families. Of those proteins, 65 differed significantly in expression: 28 were upregulated and 37 downregulated. Our data increased significantly the knowledge derived from an earlier proteomic study of the CC. Among the differentially expressed proteins are those associated with cell growth and maintenance, such as neurofilaments and tubulins; cell communication and signaling, such as 14-3-3 proteins; and oligodendrocyte function, such as myelin basic protein and myelin–oligodendrocyte glycoprotein. Additionally, 30 of the differentially expressed proteins were found previously in other proteomic studies in postmortem brains; this overlap in findings validates the present study and indicates that these proteins may be markers consistently associated with schizophrenia. Our findings increase the understanding of schizophrenia pathophysiology and may serve as a foundation for further treatment strategies.
Similar content being viewed by others
Introduction
Schizophrenia is a chronic mental disorder that usually appears at the end of adolescence or the beginning of adulthood and develops slowly for months or even years [1]. About 1 % of the world population has this condition, which presents a heritability of 80–85 % [2] and may reduce life expectancy by almost 20 years [3]. The many symptoms of schizophrenia are classified into positive symptoms, such as hallucinations, and thought disorders, and negative symptoms, such as lack of interest in social interaction, lack of motivation, and anhedonia. Cognitive deficiencies, such as the reduction in executive functions, selective attention, working memory, and mental flexibility, may also be present [4]. As a multifactorial disease, schizophrenia involves exogenous and endogenous factors as early as the beginning of neurodevelopment. Some molecular aspects of the pathology are still to be unraveled, and knowledge about the connections between the known aspects has to be improved for a more integrated understanding of schizophrenia physiopathology.
The corpus callosum (CC) is the largest portion of white matter in the human brain; it is located at its center between the right and left hemispheres and is responsible mainly for inter-hemispheric communication [5]. Morphological, electrophysiological, and neurophysiological studies have suggested alterations in the CC of schizophrenia patients [6–8]. These findings indicate the pivotal importance of the CC in establishing and maintaining schizophrenia, claiming for the understanding of its molecular features. Proteomics is a suitable tool for this purpose, since it can contribute to understanding biological and molecular processes through the integrated identification of unregulated biochemical pathways [9].
Our research group and others have contributed to this issue by analyzing the transcriptome and proteome of postmortem brain tissues and providing evidence on the potential role of oligodendrocytes and myelination in schizophrenia [10, 11]. These studies have also identified a large number of differentially expressed proteins associated with energy metabolism, the cytoskeleton, and cell signaling [12]. Since these pathways are mainly in the cytoplasm, the present study used an enrichment method to obtain only the soluble fraction of the CC proteome and pinpoints exactly differences in the expression of glial proteins, because the CC is predominantly a white matter region. The method used here is suitable for studies when one needs to obtain a detailed coverage of the proteome of interest [13].
In this paper, we describe our efforts in deciphering the cytoplasmic proteome of the CC in schizophrenia and mentally healthy controls. We chose the CC because of its importance in schizophrenia and also because of evidence on the role of glia cells in the disease. Although this brain region has been previously studied [14], the methodology used here is the state of the art in the field [15]; in contrast, in their study in 2007, Sivagnanasundaram et al. employed two-dimensional gel electrophoresis (2DE), which has intrinsic limitations for large-scale proteome analysis [16]. We cross-validated our results by comparing them with those obtained in other brain regions.
Materials and methods
Human samples
The CC samples (with no definition if from the anterior, middle, or posterior part) were provided by the BrainNet Europe consortium. Samples were collected postmortem from nine chronic schizophrenia patients with residual symptoms (diagnosed antemortem by an experienced psychiatrist according to the DSM-IV criteria) and seven controls (Table 1). Patients’ samples came from the State Mental Hospital, Wiesloch, Germany, while control samples came from the Institute of Neuropathology, Heidelberg University, Heidelberg, Germany. The controls had not had any kind of brain disorder or somatic disease and had not taken any antidepressant or antipsychotic medications. Each schizophrenia patient had a record of antipsychotic treatment, so we calculated chlorpromazine equivalents (CPE). The CPE for typical neuroleptics and clozapine were calculated with Jahn and Mussgay’s algorithm [17], while the CPE for olanzapine was calculated according to Meltzer and Fatemi [18]. Patients and controls were German Caucasians with no history of alcohol or drug abuse. Brains were submitted to neuropathological characterization to rule out any associated brain disorder. The brains analyzed here presented Braak staging less than II. All assessments, postmortem evaluations, and procedures were approved by the ethics committee of the Faculty of Medicine, Heidelberg University, Heidelberg, Germany.
Sample preparation
Cytosolic proteins were obtained from the brain tissues according to the protocol developed by Cox and Emili [19]. Twenty milligrams of each CC sample was homogenized in ten volumes of 0.32 M sucrose (Sigma-Aldrich, St. Louis, MO, USA) and 4 mM HEPES (Sigma-Aldrich) buffer (pH = 7.4), and one tablet of protease cocktail inhibitor was added (Roche Diagnostics, Indianapolis, IN, USA) per 25 ml of buffer. The homogenate was centrifuged at 1000×g for 10 min at 4 °C. Pellets were dissolved in ammonium bicarbonate 50 mM prior to protein digestion.
Nano-liquid chromatography-mass spectrometry (nano LC–MS/MS) analyses
Each sample was digested in solution overnight with a 1:80 trypsin:total protein ratio. Next, the resulting peptides were lyophilized and frozen prior to mass spectrometric analyses. Just before analysis, peptides were dissolved in 0.1 % formic acid aqueous solution and injected into a nano-LC system comprising an autosampler and 2D-nano high-performance liquid chromatography (HPLC; Eksigent, Dublin, CA, USA), coupled online to an LTQ-Orbitrap XL mass spectrometer (Thermo Scientific, Bremen, Germany). The full detailed description of the nano LC–MS/MS configuration and data analyses can be found in Maccarrone et al. [20].
Proteome quantification
CC cytosolic proteomes were quantified by the label-free spectral counting approach using Mascot Distiller (Matrix Sciences, London, UK). Mascot Distiller aligned the mass spectrometric data from each CC cytosolic sample by using mass and elution time. The quantification was based on the relative intensities of extracted ion chromatograms (XICs). FDR was set to a minimum of 0.1 and based in at least five independent MS/MS spectra.
Results and discussion
We identified a total of 5678 unique peptides that corresponded to 1636 proteins belonging to 1512 protein families on the CC cytosolic proteome. Of these proteins, 65 were differentially expressed in patients with schizophrenia compared with mentally healthy controls: 28 were upregulated and 37 downregulated (Table 2).
Of the proteins differentially expressed in schizophrenia patients, 31 % are related to cell growth and maintenance, 28 % to energy metabolism, and 20 % to cell communication and signaling. Among the proteins related to cell growth and maintenance, nine are structural, nine are cytoskeletal, and two are from the extracellular matrix; among those related to energy metabolism, 17 are metabolic enzymes; and among those related to cell communication and signaling, six are adapter molecules (Table 2), which are essential for the pathways in which they are involved. The enzymes altered in energy metabolism are key molecules to regulate the energy metabolism pathway [21, 22], and the structural and cytoskeleton proteins are indispensable to maintain cellular shape [23–26], in addition to playing a role in information transmission from dendrites to axons [27], a requirement for the cell to properly exercise its function. The receptor molecules at the membranes are related to cell communication, and, in the case of neurons, they are essential for a proper synaptic function [28, 29].
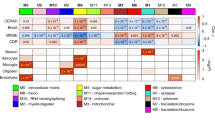
As can be seen in Fig. 1, Ingenuity Pathway Analysis (IPA, Ingenuity Systems, Qiagen, Redwood, CA, USA; www.ingenuity.com) also showed that these proteins clustered within those pathways. IPA is based on an algorithm that uses curated connectivity information from the literature to determine the network of interactions among the differentially expressed proteins and canonical pathways in which they are involved [30].
As shown in Fig. 1, three predominant pathways have differentially expressed proteins in schizophrenia: energy metabolism, cell communication and signaling, and cell growth and maintenance. These pathways have already been found to be dysregulated in patients with schizophrenia [14, 23, 31]. This protein network also evidences connections among differentially expressed proteins within their biological processes and between different processes, suggesting dysfunctional networks of proteins, as is known to be the case in schizophrenia [32].
In addition, information provided about altered canonical pathways in schizophrenia samples shows that differently expressed proteins are related to each other as part of common pathways, such as cell metabolism and cell signaling, as shown in Fig. 2, further reinforcing those pathways’ dysregulation, as shown in Fig. 1. All pathways were significantly altered in the schizophrenia samples compared to the control samples (p < 0.05). The information also indicates that canonical pathways are associated to oxidative stress such as superoxide radical degradation and NRF2-mediated oxidative stress response.
We compared our results with those obtained by Sivagnanasundaram et al. [25]. Using the combination of 2DE and mass spectrometry (2DE-MS), they identified 34 differentially expressed proteins in the CC in schizophrenia, nine of which overlap with the data we present here. To validate our findings and also to highlight proteins consistently different in expression in schizophrenia patients’ brains, we compared our results to 16 other brain tissue studies of the proteome of schizophrenia. Thirty of the proteins differentially expressed in our study overlap with these studies (Table 3).
Several studies consistently found differential expression of proteins associated with 14-3-3-mediated signaling, the pathway in which we found the main disruption in the CC of schizophrenia patients (Fig. 2). 14-3-3 protein zeta/delta (YWHAZ), 14-3-3 protein epsilon (YWHAE), and 14-3-3 protein gamma (YWHAG) are associated with cell communication and signaling, as binding proteins to several protein kinases and phosphatases, and also are involved in actin dynamics. They were found dysregulated also in other reports on the schizophrenia proteome [32]. The 14-3-3 protein family is highly associated with neurotransmitting processes [28], with some isoforms particularly enriched in synapses, and the YWHAZ and YWHAE genes were previously associated with schizophrenia [33–35]. For instance, broad 14-3-3 functional knockout mice, in addition to showing schizophrenia-like behavior, have high dopamine levels and a decrease in dendritic complexity and spine density, defects linked to schizophrenia [36]. As the main white matter region in the brain, the CC is composed mostly of glia cells and neuronal axons. Because these axons are responsible for the connection between the two brain hemispheres, the dysregulation of proteins involved in cell communication and neurotransmission may be pivotal to impairments in brain connectivity, as previously suggested [6–8].
Genome-wide association studies (GWAS) found that the gene for the protein clathrin heavy chain 1 (CLTC) is associated with schizophrenia. The protein, that has been found downregulated in our results (Table 2), has the function of a vesicle coat and plays a role in clathrin-mediated endocytosis and thus is involved in cell signaling [37]. According to Schubert el al. [38], clathrin influences processes such as synaptic dysfunction, white matter changes, and aberrant neurodevelopment and consequently may be related to schizophrenia pathology.
We found differential expression of the light and medium neurofilaments (NEFL and NEFM), as did Sivagnanasundaram et al. [25]. Differential expression of NEFM was found also by five other studies and differential expression of NEFL by two, highlighting their importance in schizophrenia. These proteins, which are coded by gene regions that are usually altered in schizophrenia patients [23, 26], are associated with cell growth and maintenance, reinforcing the role of this pathway in schizophrenia [23, 25, 39]. Neurofilaments play also important roles in the function of oligodendrocytes, cells enriched in brain white matter. Along these lines, we observed also the downregulation of myelin basic protein (MBP) and myelin–oligodendrocyte glycoprotein (MOG), the main constituents of myelin sheaths. These proteins were previously found differentially expressed in other schizophrenia brain regions [10, 32, 39], a finding that is in line with evidence at the transcriptome [40, 41] and morphological levels [42, 43]. The differential expression of MBP and MOG supports the idea that a degenerative process might be occurring in schizophrenia brains [10, 44–46]. Also, MBP and MOG might be biomarker candidates to be further investigated in combination with other potential biomarkers, since they were found in different concentrations in the cerebrospinal fluid (CSF) of living schizophrenia patients [23].
The family of tubulin proteins also was associated with the cell cytoskeleton. The isoform TUBB was found in our study and another ten studies (Table 3), which reinforces its role in schizophrenia pathobiology. According to Moehle et al. [47], tubulin proteins are the major protein components in axons, dendrites, and dendritic spines, and knockdown studies indicate that the different isoforms have distinct roles in neurodevelopment. Studies with mice knocked out for the STOP gene (stable tubulin-only polypeptide) have associated the family of tubulin proteins with synaptic dysfunctions probably caused by glutamatergic transmission dysregulation [14, 48].
The protein gelsolin (GSN) belongs to a superfamily of actin-binding proteins (ABPs) [49] and is related to actin remodeling on cell growth and apoptosis [50]. Our studies and that of Prabakaran et al. [51] found this protein to be downregulated, and transcriptome studies found its gene to be altered [10]. Considering that this protein is related also to myelin sheath generation and maintenance [44], it may be involved in myelination dysfunction in schizophrenia patients.
Another protein found upregulated here and differentially expressed in other four schizophrenia proteome analyses was gamma-enolase (ENO2). This enzyme participates in the glycolytic pathway, a pathway found to be the second most affected in this study (Fig. 2) and also by others [22]. ENO2 interconverts 2-phosphoglycerate to phosphoenolpyruvate [21]. Since glia cells are responsible for supplying energy to neuronal axons [52], this glycolysis dysregulation may affect negatively synaptic activity and neuronal plasticity [25, 39, 53]. Another three glycolytic enzymes were differentially expressed in our study but not in the study by Sivagnanasundaram et al. [25]. These three are pyruvate kinase (PKM), fructose-bisphosphate aldolase A (ALDOA), and glyceraldehyde-3-phosphate dehydrogenase (GAPDH), confirming the dysregulation in schizophrenia of glycolysis, a pivotal energy pathway [22].
In agreement with Sivagnanasundaram et al. [25] and another two studies (Table 3), we found differential expression of superoxide dismutase [Cu–Zn] (SOD1), which has been observed consistently to be dysregulated in the brain and liver of patients with schizophrenia [22, 54–57]. Our study and another two studies (Table 3) also found another protein related to oxidative stress, peroxiredoxin-1 (PRDX1), to be downregulated, reinforcing the concept of a reduced response to oxidative stress [58, 59].
Conclusions
Given the central role of the corpus callosum, our data revisited proteome alterations of this brain region with a more powerful proteomic methodology. To provide further evidence for the dysregulation of signaling and structural proteins, we investigated the cytosolic fraction of the CC proteome. We found not only these pathways dysregulated, but also we were able to reinforce the role of energy metabolism and oligodendrocytes in schizophrenia, despite the data provided in this study should further be validated by other orthogonal methods (i.e., western blot, immunocytochemistry). Our findings increase the understanding of schizophrenia pathophysiology and could be targeted for further treatment strategies.
References
Freedman R (2003) Schizophrenia. N Engl J Med 349(18):1738–1749
Sullivan PF, Kendler KS, Neale MC (2003) Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Arch Gen Psychiatry 60(12):1187–1192
Hegarty JD, Baldessarini RJ, Tohen M, Waternaux C, Oepen G (1994) One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am J Psychiatry 151(10):1409–1416
Weickert TW, Goldberg TE, Gold JM, Bigelow LB, Egan MF, Weinberger DR (2000) Cognitive impairments in patients with schizophrenia displaying preserved and compromised intellect. Arch Gen Psychiatry 57(9):907–913
Fitsiori A, Nguyen D, Karentzos A, Delavelle J, Vargas MI (2011) The corpus callosum: white matter or terra incognita. Br J Radiol 84:5–18
Guo H, Christoff JM, Campos VE, Li Y (2000) Normal corpus callosum in Emx1 mutant mice with C57BL/6 background. Biochem Biophys Res Commun 276(2):649–653
Rotarska-Jagiela A, Schönmeyer R, Oertel V, Haenschel C, Vogeley K, Linden DEJ (2008) The corpus callosum in schizophrenia—volume and connectivity changes affect specific regions. NeuroImage 39:1522–1532
Innocenti GM, Ansermet F, Parnas J (2003) Schizophrenia, neurodevelopment and corpus callosum. Mol Psychiatry 8:261–274
Martins-De-Souza D (2012) Proteomics tackling schizophrenia as a pathway disorder. Schizophr Bull 38(6):1107–1108
Martins-de-Souza D (2010) Proteome and transcriptome analysis suggests oligodendrocyte dysfunction in schizophrenia. J Psychiatr Res 44(3):149–156. doi:10.1016/j.jpsychires.2009.07
Horvth S, Janka Z, Mirnics K (2011) Analyzing schizophrenia by DNA microarrays. Biol Psychiatry 69(2):157–162. doi:10.1016/j.biopsych.2010.07.017
Nascimento JM, Martins-de-Souza D (2015) The proteome of schizophrenia. Npj Schizophrenia 1:14003
Rockstroh M, Müller SA, Jende C, Kerzhner A, von Bergen M, Tomm JM (2011) Cell fractionation—an important tool for compartment proteomics. OMICS 1:135–143
Martins-de-Souza D, Gattaz WF, Schmitt A, Novello JC, Marangoni S, Turck CW, Dias-Neto E (2009) Proteome analysis of schizophrenia patients Wernicke’s area reveals an energy metabolism dysregulation. BMC Psychiatry 9:17
Nogueira FCS, Domont GD (2014) Survey of shotgun proteomics. Shotgun proteomics. Springer, New York, pp 3–23
Oliveira BM, Coorssen JR, Martins-de-Souza D (2014) 2DE: the phoenix of proteomics. J Proteomics 104:140–150
Jahn T, Mussgay L (1989) Die statistische Kontrolle moeglicher Medikamenteneinfluesse in experimentalpsychologischen Schizophrenie studien: Ein Vorschlag zur Berechnung von Chlorpromazina aequivalenten. Z Klin Psychol Psychother 18:10
Meltzer HY, Fatemi SH (1998) Treatment of schizophrenia. In: Schatzberg AF, Nemeroff CB (eds) The American psychiatric text book of psychopharmacology. American Psychiatric Press, Washington, pp 127–135 10
Cox B, Emili A (2006) Tissue subcellular fractionation and protein extraction for use in mass-spectrometry-based proteomics. Nat Protoc 1(4):1872–1878. doi:10.1038/nprot.2006.273
Maccarrone G, Rewerts C, Lebar M, Turck CW, Martins-de- Souza D (2013) Proteome profiling of peripheral mononuclear cells from human blood. Proteomics 13:893–897
Oliva Daniele et al (1991) Complete structure of the human gene encoding neuron-specific enolase. Genomics 10(1):157–165
Martins-de-Souza D, Harris LW, Guest PC, Bahn S (2011) The role of energy metabolism dysfunction and oxidative stress in schizophrenia revealed by proteomics. Antioxid Redox Signal 15(7):2067–2079. doi:10.1089/ars.2010.3459
Martins-de-Souza D, Maccarrone G, Wobrock T, Zerr I, Gormanns P, Reckow S, Turck CW (2010) Proteome analysis of the thalamus and cerebrospinal fluid reveals glycolysis dysfunction and potential biomarkers candidates for schizophrenia. J Psychiatr Res 44(16):1176–1189
Ishtiaq M, Campos-Melo D, Volkening K, Strong MJ (2014) Analysis of novel NEFL mRNA targeting microRNAs in amyotrophic lateral sclerosis. PLoS One 9(1):e85653. doi:10.1371/journal.pone.0085653
Sivagnanasundaram S, Crossett B, Dedova I, Cordwell S, Matsumoto I (2007) Abnormal pathways in the genu of the corpus callosum in schizophrenia pathogenesis: a proteome study. Proteomics Clin Appl 1:1291–1305
Bergson C, Levenson R, Goldman-Rakic PS, Lidow MS (2003) Dopamine receptor-interacting proteins: the Ca2+ connection in dopamine signaling. Trends Pharmacol Sci 24:486–492
Kapitein LC, Hoogenraad CC (2011) Which way to go? Cytoskeletal organization and polarized transport in neurons. Mol Cell Neurosci 46(1):9–20
Berg D, Holzmann C, Riess O (2003) 14-3-3 proteins in the nervous system. Nat Rev Neurosci 4(September):752–762
Muratake T, Hayashi S, Ichikawa T, Kumanishi T, Ichimura Y, Kuwano R, Takahashi Y (1996) Structural organization and chromosomal assignment of the human 14-3-3 eta chain gene (YWHAH). Genomics 36:63–69
Calvano SE, Xiao W, Richards DR, Felciano RM, Baker HV, Cho RJ, Lowry SF (2005) A network-based analysis of systemic inflammation in humans. Nature 437(October):1032–1037
Martins-de-Souza D, Gattaz WF, Schmitt A, Maccarrone G, Hunyadi-Gulyás E, Eberlin MN, Dias-Neto E (2009) Proteomic analysis of dorsolateral prefrontal cortex indicates the involvement of cytoskeleton, oligodendrocyte, energy metabolism and new potential markers in schizophrenia. J Psychiatr Res 43(11):978–986
Martins-de-Souza D, Guest PC, Rahmoune H, Bahn S (2012) Proteomic approaches to unravel the complexity of schizophrenia. Expert Rev Proteomics 9(1):97–108
Bell R, Munro J, Russ C, Powell JF, Bruinvels A, Kerwin RW, Collier DA (2000) Systematic screening of the 14-3-3 eta (eta) chain gene for polymorphic variants and case-control analysis in schizophrenia. Am J Med Genet 96:736–743
Wong AHC, Likhodi O, Trakalo J, Yusuf M, Sinha A, Pato CN, Kennedy JL (2005) Genetic and post-mortem mRNA analysis of the 14-3-3 genes that encode phosphoserine/threonine-binding regulatory proteins in schizophrenia and bipolar disorder. Schizophr Res 78:137–146
Ikeda M, Hikita T, Taya S, Uraguchi-asaki J, Toyo-Oka K, Wynshaw-boris A, Iwata N (2008) Identification of YWHAE, a gene encoding 14-3-3 epsilon, as a possible susceptibility gene for schizophrenia. Hum Mol Genet 17(20):3212–3222
Foote M, Qiao H, Graham K, Wu Y, Zhou Y (2015) Inhibition of 14-3-3 proteins leads to schizophrenia-related behavioral phenotypes and synaptic defects in mice. Biol Psychiatry 1–10. doi:10.1016/j.biopsych.2015.02.015
Schmid SL (1997) Clathrin-coated vesicle formation and protein sorting: an integrated process. Annu Rev Biochem 66(1):511–548
Schubert KO, Föcking M, Prehn JHM, Cotter DR (2012) Hypothesis review: are clathrin-mediated endocytosis and clathrin-dependent membrane and protein trafficking core pathophysiological processes in schizophrenia and bipolar disorder? Mol Psychiatry 17(7):669–681. doi:10.1038/mp.2011.123
Martins-De-Souza D, Gattaz WF, Schmitt A, Rewerts C, Marangoni S, Novello JC, Dias-Neto E (2009) Alterations in oligodendrocyte proteins, calcium homeostasis and new potential markers in schizophrenia anterior temporal lobe are revealed by shotgun proteome analysis. J Neural Transm 116:275–289
Hakak Y, Walker JR, Li C, Wong WH, Davis KL, Buxbaum JD et al (2001) Genome-wide expression analysis reveals dysregulation of myelination-related genes in chronic schizophrenia. Proc Natl Acad Sci USA 98(8):4746–4751
Tkachev D, Mimmack ML, Ryan MM, Wayland M, Freeman T, Jones PB et al (2003) Oligodendrocyte dysfunction in schizophrenia and bipolar disorder. Lancet 362(9386):798–805
Foong J, Maier M, Barker GJ, Brocklehurst S, Miller DH, Ron MA (2000) In vivo investigation of white matter pathology in schizophrenia with magnetization transfer imaging. J Neurol Neurosurg Psychiatry 68:70–74
Uranova N, Orlovskaya D, Vikhreva O, Zimina I, Kolomeets N, Vostrikov V et al (2001) Electron microscopy of oligodendroglia in severe mental illness. Brain Res Bull 55(5):597–610
Konrad A, Winterer G (2008) Disturbed structural connectivity in schizophrenia—primary factor in pathology or epiphenomenon? Schizophr Bull 34(1):72–92. doi:10.1093/schbul/sbm034
Bartzokis G (2002) Schizophrenia: breakdown in the well- regulated lifelong process of brain development and maturation. Neuropsychopharmacology 27(4):672–683
Chew LJ, Fusar-Poli P, Schmitz T (2013) Oligodendroglial alterations and the role of microglia in white matter injury: relevance to schizophrenia. Dev Neurosci 35(2–3):102–129. doi:10.1159/000346157
Moehle MS, Luduena RF, Haroutunian V, Meador-Woodruff JH, McCullumsmith RE (2012) Regional differences in expression of β-tubulin isoforms in schizophrenia. Schizophr Res 135(1):181–186
Denarier E, Aguezzoul M, Jolly C, Vourc’h C, Roure A, Andrieux A et al (1998) Genomic structure and chromosomal mapping of the mouse STOP gene (Mtap6). Biochem Biophys Res Commun 243:791–796
Xi ZR, Qin W, Yang YF, He G, Gao SH, Ren MS, He L (2004) Transmission disequilibrium analysis of the GSN gene in a cohort of family trios with schizophrenia. Neurosci Lett 372(3):200–203. doi:10.1016/j.neulet.2004.09.041
Sun HQ, Yamamoto M, Mejillano M, Yin HL (1999) Gelsolin, a multifunctional actin regulatory protein. J Biol Chem 274(47):33179–33182. doi:10.1074/jbc.274.47.33179
Prabakaran S, Wengenroth M, Lockstone HE, Lilley K, Leweke FM, Bahn S (2007) 2-D DIGE analysis of liver and red blood cells provides further evidence for oxidative stress in schizophrenia. J Proteome Res 6:141–149
Funfschilling U, Supplie LM, Mahad D, Boretius S, Aiman S, Edgar J, Nave K (2013) Glycolytic oligodendrocytes maintain myelin and long-term axonal integrity. Nature 485(7399):517–521. doi:10.1038/nature11007
Magistretti PJ (2011) Neuron-glia metabolic coupling and plasticity. Exp Physiol 96:407–410
Reddy RD, Sahebarao MP, Mukherjee S, Murthy JN (1991) Enzymes of the antioxidant defense system in chronic schizophrenic patients. Biol Psychiatry 30:409–412
Yao JK, Reddy RD, van Kammen DP (2001) Oxidative damage and schizophrenia: an overview of the evidence and its therapeutic implications. CNS Drugs 15:287–310
Zhang XY, Zhou DF, Cao LY, Zhang PY, Wu GY (2003) Elevated blood superoxide dismutase in neuroleptic-free schizophrenia: association with positive symptoms. Psychiatry Res 117:85–88
Rajasekaran A, Venkatasubramanian G, Berk M, Debnath M (2015) Mitochondrial dysfunction in schizophrenia: pathways, mechanisms and implications. Eurosci Biobehav Rev 48:10–21
Föcking M, Lopez LM, English JA, Dicker P, Wolff A, Brindley E, Cotter DR (2014) Proteomic and genomic evidence implicates the postsynaptic density in schizophrenia. Mol Psychiatry 20:424–432. doi:10.1038/mp.2014.63
Prabakaran S, Swatton JE, Ryan MM, Huffaker SJ, Huang JT-J, Griffin JL, Bahn S (2004) Mitochondrial dysfunction in schizophrenia: evidence for compromised brain metabolism and oxidative stress. Mol Psychiatry 9(7):684–697
Clark D, Dedova I, Cordwell S, Matsumoto I (2006) A proteome analysis of the anterior cingulate cortex gray matter in schizophrenia. Mol Psychiatry 11(5):459–470
Beasley CL, Pennington K, Behan A, Wait R, Dunn MJ, Cotter D (2006) Proteomic analysis of the anterior cingulate cortex in the major psychiatric disorders: Evidence for disease-associated changes. Proteomics 6(11):3414–3425
Pennington K, Beasley CL, Dicker P, Fagan A, English J, Pariante CM, Cotter DR (2008) Prominent synaptic and metabolic abnormalities revealed by proteomic analysis of the dorsolateral prefrontal cortex in schizophrenia and bipolar disorder. Mol Psychiatry 13(12):1102–1117
Behan AT, Byrne C, Dunn MJ, Cagney G, Cotter DR (2009) Proteomic analysis of membrane microdomain-associated proteins in the dorsolateral prefrontal cortex in schizophrenia and bipolar disorder reveals alterations in LAMP, STXBP1 and BASP1 protein expression. Mol Psychiatry 14(6):601–613
Pennington K, Dicker P, Dunn MJ, Cotter DR (2008) Proteomic analysis reveals protein changes within layer 2 of the insular cortex in schizophrenia. Proteomics 8(23–24):5097–5107
Martins-de-Souza D, Gattaz WF, Schmitt A, Rewerts C, Maccarrone G, Dias-Neto E, Turck CW (2009) Prefrontal cortex shotgun proteome analysis reveals altered calcium homeostasis and immune system imbalance in schizophrenia. Eur Arch Psychiatry Clin Neurosci 259(3):151–163
English JA, Dicker P, Föcking M, Dunn MJ, Cotter DR (2009) 2-D DIGE analysis implicates cytoskeletal abnormalities in psychiatric disease. Proteomics 9(12):3368–3382
Schubert KO, Föcking M, Cotter DR (2015) Proteomic pathway analysis of the hippocampus in schizophrenia and bipolar affective disorder implicates 14-3-3 signaling, aryl hydrocarbon receptor signaling, and glucose metabolism: potential roles in GABAergic interneuron pathology. Schizophr Res. doi:10.1016/j.schres.2015.02.002
Föcking M, Dicker P, English JA, Schubert KO, Dunn MJ, Cotter DR (2011) Common proteomic changes in the hippocampus in schizophrenia and bipolar disorder and particular evidence for involvement of cornu ammonis regions 2 and 3. Arch Gen Psychiatry 68(5):477–488
Martins-de-Souza D, Schmitt A, Röder R, Lebar M, Schneider-Axmann T, Falkai P, Turck CW (2010) Sex-specific proteome differences in the anterior cingulate cortex of schizophrenia. J Psychiatr Res 44(14):989–991
Acknowledgments
The authors thank Prof. Sabine Bahn (University of Cambridge, UK) for providing access to IPA, and Jacquie Klesing, Board-certified Editor in the Life Sciences (ELS), for editing assistance with the manuscript. D.M.S., J.S.C. and J.M.N. are funded by FAPESP (São Paulo Research Foundation, Grants 2013/08711-3, 2014/10068-4, 2014/21035-0 and 2014/14881-1) and CNPq (The Brazilian National Council for Scientific and Technological Development, Grant 460289/2014-4).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Saia-Cereda, V.M., Cassoli, J.S., Schmitt, A. et al. Proteomics of the corpus callosum unravel pivotal players in the dysfunction of cell signaling, structure, and myelination in schizophrenia brains. Eur Arch Psychiatry Clin Neurosci 265, 601–612 (2015). https://doi.org/10.1007/s00406-015-0621-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00406-015-0621-1