Abstract
Introduction
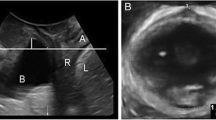
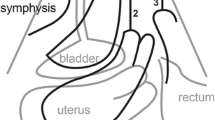
Pelvic floor ultrasound plays a major role in urogynecologic diagnostics. Using 3D ultrasound we can identify integrity of levator ani and measure hiatal area in the axial plane. The main goal of our study was to measure hiatal area on Valsalva in a cohort of urogynecological patients. Furthermore, we aimed to correlate hiatal area with urogynecological symptoms, levator integrity and evaluate cut-off values for pelvic organ prolapse.
Materials and methods
In a retrospective analysis, we included 246 patients seen for urogynecological problems in our tertiary urogynecological unit. After a standardized interview and physical examination, a 3D pelvic floor ultrasound was performed. According to the cardinal urogynecological symptoms and signs, patients were categorized into three groups: pelvic organ prolapse, stress urinary incontinence and overactive bladder symptoms.
Results
Median age of our study population was 66 (range 29–94) years, median parity was 2.1 (range 0–9) with 17 (6.9 %) nulliparous women. Symptoms of overactive bladder in 71.1 % were most common, followed by 54.5 % symptoms of stress incontinence and 32.1 % symptoms of prolapse. On examination 49.2 % showed signs of prolapse. Levator avulsions on 3D ultrasound were detected in 20.7 %. Hiatal area was normally distributed with a median of 28.7 cm2 (range 10.4–50.0 cm2). Patients with levator avulsion had a significantly larger hiatal area (p < 0.001). Also patients with signs of prolapse had a significantly larger hiatal area (p < 0.001). There was no correlation between hiatal area and symptoms of overactive bladder (p = 0.374). Although not reaching statistical significance there was evidence of a smaller hiatal area for patients with stress incontinence (p = 0.016). In our cohort there were 33.7 % (83) women without ballooning, 27.2 % (67) showed mild, 18.3 % (45) moderate, 12.3 % (30) marked and 8.5 % (21) severe ballooning. The ROC curve analysis for hiatal area on patients with prolapse yielded an AUC of 0.755 [95 % CI (0.696–0.814)]. Using the Youden-Index we obtained 27.53 cm2 as a cut-off with a sensitivity of 0.70 and a specificity of 0.69.
Discussion
Hiatal area is a new repeatable diagnostic parameter. Its clinical application could improve our understanding of the pathophysiology of pelvic organ prolapse as a form of hiatal hernia.





Similar content being viewed by others
References
Rortveit G, Brown JS, Thom DH, Van Den Eeden SK, Creasman JM, Subak LL (2007) Symptomatic pelvic organ prolapse: prevalence and risk factors in a population-based, racially diverse cohort. Obstet Gynecol 109:1396–1403
Chow D, Rodriguez LV (2013) Epidemiology and prevalence of pelvic organ prolapse. Curr Opin Urol 23:293–298
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M (2014) Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol 123:1201–1206
Smith FJ, Holman CD, Moorin RE, Tsokos N (2010) Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol 116:1096–1100
Strohbehn K, Ellis JH, Strohbehn JA, DeLancey JO (1996) Magnetic resonance imaging of the levator ani with anatomic correlation. Obstet Gynecol 87:277–285
Petri E, Kölbl H, Schär G (1999) What is the place of ultrasound in urogynecology? A written panel. Int Urogynecol J Pelvic Floor Dysfunct 10:262–273
Gupta S, Sharma JB, Hari S, Kumar S, Roy KK, Singh N (2012) Study of dynamic magnetic resonance imaging in diagnosis of pelvic organ prolapse. Arch Gynecol Obstet 286:953–958
Tunn R, Petri E (2003) Introital and transvaginal ultrasound as the main tool in the assessment of urogenital and pelvic floor dysfunction: an imaging panel and practical approach. Ultrasound Obstet Gynecol 22:205–213
Tunn R et al (2005) Updated recommendations on ultrasonography in urogynecology. Int Urogynecol J Pelvic Floor Dysfunct 16:236–241
Albrich S, Bauer RM, Haberer E, Skala C, Naumann G (2013) Importance of sonography in the diagnostics of functional disorders of the female pelvic floor. Der Urol Ausg A 52:533–540
Dietz HP (2006) Why pelvic floor surgeons should utilize ultrasound imaging. Ultrasound Obstet Gynecol 28:629–634
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I (2013) Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG Int J Obstet Gynaecol 120:152–160
Vergeldt TF, Weemhoff M, IntHout J, Kluivers KB (2015) Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J 26:1559–1573
Dietz HP (2010) Geburtsbedingtes Beckenbodentrauma. Geburtshilfe Frauenheilkd 70:969–978
Walker GJ, Gunasekera P (2011) Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J 22:127–135
Dietz HP (2004) Ultrasound imaging of the pelvic floor. Part II: three-dimensional or volume imaging. Ultrasound Obstet Gynecol 23:615–625
Albrich S, Steetskamp J, Knoechel SL, Porta S, Hoffmann G, Skala C (2016) Assessment of pelvic floor muscle contractility: digital palpation versus 2D and 3D perineal ultrasound. Arch Gynecol Obstet 293:839–843
Dietz HP, Lanzarone V (2005) Levator trauma after vaginal delivery. Obstet Gynecol 106:707–712
Tunn R, DeLancey JO, Howard D, Thorp JM, Ashton-Miller JA, Quint LE (1999) MR imaging of levator ani muscle recovery following vaginal delivery. Int Urogynecol J Pelvic Floor Dysfunct 10:300–307
Hoyte L, Schierlitz L, Zou K, Flesh G, Fielding JR (2001) Two- and 3-dimensional MRI comparison of levator ani structure, volume, and integrity in women with stress incontinence and prolapse. Am J Obstet Gynecol 185:11–19
DeLancey JO, Sorensen HC, Lewicky-Gaupp C, Smith TM (2012) Comparison of the puborectal muscle on MRI in women with POP and levator ani defects with those with normal support and no defect. Int Urogynecol J 23:73–77
Shek KL, Dietz HP (2010) Intrapartum risk factors for levator trauma. BJOG Int J Obstet Gynaecol 117:1485–1492
Albrich SB, Laterza RM, Skala C, Salvatore S, Kölbl H, Naumann G (2012) Impact of mode of delivery on levator morphology: a prospective observational study with three-dimensional ultrasound early in the postpartum period. BJOG Int J Obstet Gynaecol 119:51–60
Dietz HP, Franco AV, Shek KL, Kirby A (2012) Avulsion injury and levator hiatal ballooning: two independent risk factors for prolapse? An observational study. Acta Obstet Gynecol Scand 91:211–214
Albrich S, Rommens K, Steetskamp J, Weyer V, Hoffmann G, Skala C, Zahn E (2015) Prevalence of levator ani defects in urogynecological patients. Geburtshilfe Frauenheilkunde 75:51–55
Weemhoff M, Vergeldt TF, Notten K, Serroyen J, Kampschoer PH, Roumen FJ (2012) Avulsion of puborectalis muscle and other risk factors for cystocele recurrence: a 2-year follow-up study. Int Urogynecol J 23:65–71
Wong V, Shek K, Rane A, Goh J, Krause H, Dietz HP (2013) Is levator avulsion a predictor of cystocele recurrence following anterior vaginal mesh placement? Ultrasound Obstet Gynecol 42:230–234
Dietz HP, Shek C, De Leon J, Steensma AB (2008) Ballooning of the levator hiatus. Ultrasound Obstet Gynecol 31:676–680
Dietz HP, Shek KL (2009) Tomographic ultrasound imaging of the pelvic floor: which levels matter most? Ultrasound Obstet Gynecol 33:698–703
Dietz HP, Shek C, Clarke B (2005) Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol 25:580–585
Majida M, Braekken IH, Umek W, Bo K, Saltyte Benth J, Ellstrom Engh M (2009) Interobserver repeatability of three- and four-dimensional transperineal ultrasound assessment of pelvic floor muscle anatomy and function. Ultrasound Obstet Gynecol 33:567–573
Hampel C, Gillitzer R, Pahernik S, Hohenfellner M, Thuroff JW (2003) Epidemiology and etiology of overactive bladder. Der Urol Ausg A 42:776–786
Jundt K, Scheer I, Schiessl B, Karl K, Friese K, Peschers UM (2010) Incontinence, bladder neck mobility, and sphincter ruptures in primiparous women. Eur J Med Res 15:246–252
Falkert A, Willmann A, Endress E, Meint P, Seelbach-Gobel B (2013) Three-dimensional ultrasound of pelvic floor: is there a correlation with delivery mode and persisting pelvic floor disorders 18–24 months after first delivery? Ultrasound Obstet Gynecol 41:204–209
Pirpiris A, Shek KL, Dietz HP (2010) Urethral mobility and urinary incontinence. Ultrasound Obstet Gynecol 36:507–511
Abdool Z, Shek KL, Dietz HP (2009) The effect of levator avulsion on hiatal dimension and function. Am J Obstet Gynecol 201(89):e1–e5
Shek KL, Pirpiris A, Dietz HP (2010) Does levator avulsion increase urethral mobility? Eur J Obstet Gynecol Reprod Biol 153:215–219
Acknowledgments
Parts of the doctoral thesis of co-author Bente Wolpert were included in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors indicate no potential conflict of interest in relation to this article.
Financial interest
All authors indicate no financial interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional research committee.
Informed consent
Due to the retrospective nature of the research and the fact that all data collection occurred as part of routine clinical care, our institutional research committee waived the requirement for individual informed consent.
Rights and permissions
About this article
Cite this article
Albrich, S.B., Welker, K., Wolpert, B. et al. How common is ballooning? Hiatal area on 3D transperineal ultrasound in urogynecological patients and its association with lower urinary tract symptoms. Arch Gynecol Obstet 295, 103–109 (2017). https://doi.org/10.1007/s00404-016-4200-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4200-0