Abstract
Objective
This meta-study intends to elucidate schizophrenia–pregnancy inferences.
Methods
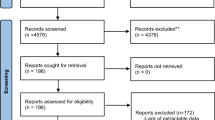
A total of 63 quasi-randomized, case–control, linkage studies on outcomes of singleton pregnancies in women with schizophrenia are identified through PubMed, ACOG, and SCOPUS. A sample of 216 pregnant and puerperal women with schizophrenia, allocated from studies of level I–IIA evidence, is compared with a sample of 487 births to unaffected women. Calculations use births as unit of analysis. Poisson regression model is used in exchangeable correlation structure.
Results
Older age (2.13), excessive smoking (1.85) and less antenatal care (1.92) in women with schizophrenia determine high risk for prematurity (2.08), including miscarriages (2.04) and preterm birth (1.98). Neonates to mothers with schizophrenia are profiled with twice likelihood of low Apgar scores (2.22), intrauterine growth retardation (2.16), and congenital defects (2.1). Poor maternal–fetal attachment and preoccupation about fetus are related to negative symptoms of schizophrenia (−0.518), length of antipsychotic treatment (−0.304) and are not associated with maternal age (0.216). Postpartum period is eventful with psychotic relapse (7.86), and parenting difficulties (11.2).
Conclusions
After adjusting for age, parity, unhealthy behaviors, length of antipsychotic treatment, and maternal–fetal attachment, maternal schizophrenia remains predictive to prematurity and postpartum psychosis.

Similar content being viewed by others
References
Ahern N, Ruland JP (2003) Maternal–fetal attachment. J Perinat Educ 12(4):27–35
Aichhorn W, Stuppaeck C, Whitworth AB (2005) Risperidone and breast-feeding. J Psychopharmacol 19:211–213
Alhusen JL (2008) A literature update on maternal–fetal attachment. J Obstet Gynecol Neonat Nurs 37(3):315–328
Altshuler LL, Cohen L, Szuba MP et al (1996) Pharmacological management of psychiatric illness during pregnancy: dilemmas and guidelines. Am J Psychiatry 153:592–606
Bennedsen BE, Mortensen PB, Olesen AV et al (1999) Preterm birth and intra-uterine growth retardation among children of women with schizophrenia. Br J Psychiatry 175:239–245
Bennedsen BE, Mortensen PB, Olesen AV et al (2001) Obstetric complications in women with schizophrenia. Schizophr Res 47(203):167–175
Condon JT (1993) The assessment of antenatal emotional attachment: development of a questionnaire instrument. Br J Med Psychol 66(pt 2):167–183
Cranley MS (1981) Development of a tool for the measurement of maternal attachment during pregnancy. Nurs Res 30:281–284
Dev V, Krupp P (1995) Adverse event profile and safety of clozapine. Rev Contemp Pharmacother 6:197–208
Dudzinski DM, Sullivan M (2004) When agreeing with the patient is not enough: a schizophrenic woman requests pregnancy termination. Law Ethics Psychiatry
Ellman LN, Huttenen M, Lönnqvist J et al (2007) The effects of genetic liability for schizophrenia and maternal smoking during pregnancy on obstetrical complications. Schizophr Res 93(1–3):229–236
Field MA (1989) Controlling the woman to protect the fetus. Law Med Health Care 17(2):114–129
Gardiner SJ, Kristensen JH, Begg EJ et al (2003) Transfer of olanzapine into breast milk, calculation of infant drug dose, and effect on breast-fed infants. Am J Psychiatry 160:1428–1431
Hendrick V (2006) Psychiatric disorders in pregnancy and the postpartum: principles and treatment. (Current Clinical Practice Series) Hardcover, Humana Press
Hill RC, McIvor RJ, Wojnar-Horton RE et al (2000) Risperidone distribution and excretion into human milk: case report and estimated infant exposure during breast-feeding. J Clin Psychopharmacol 20:285–286
Hizkiyahu R, Levy A, Sheiner E (2009) Pregnancy outcome of patients with schizophrenia. Am J Perinatol 27(1):19–23
Howard LM, Kumar R, Thornicroft G (2001) Psychosocial characteristics and needs of mothers with psychotic disorders. Br J Psychiatry 178:427–432
Howard LM (2005) Fertility and pregnancy in women with psychotic disorders. Eur J Obstetrics Gynecology Reprod Biol 119:3–10
Hultman CM, Cnattingius S, Olausson PO et al (2008) Schizophrenia and offspring’s risk for adverse pregnancy outcomes and infant death. Br J Psychiatry 193:311–315
Ilett KF, Hackett LP, Kristensen JH et al (2004) Transfer of risperidone and 9-hydroxyrisperidone into human milk. Ann Pharmacother 38:273–276
Jablensky AV, Morgan V, Soc MS et al (2005) Pregnancy, delivery, and neonatal complications in a population cohort of women with schizophrenia and major affective disorders. Am J Psychiatry 162:79–91
Jeffries JJ, Plummer E, Thornton JF, Seeman MV (1999) Living and working with schizophrenia, 2nd edn, Hardcover
King-Hele SA, Abel KM, Webb RT et al (2007) Risk of sudden infant death syndrome with parental mental illness. Arch Gen Psychiatry 64(11):1323–1330
Kolder VE, Gallagher J (1987) Court-ordered obstetrical interventions. N Engl J Med 316(19):1192–1196
Kotlicka AM, Gmitrowitcz A, Sobow TM et al (2001) Obstetrical complications and Apgar score in early-onset schizophrenic patients with prominent positive and prominent negative symptoms. J Psychiatr Res 35(4):249–257
Lee HC, Lin HC (2009) Maternal bipolar disorder increased low birth weight and preterm births: a nationwide population-based study. J Affect Disord 121(1–2):100–105
Lee A, Giesbrecht E, Dunn E et al (2004) Excretion of quetiapine in breast milk. Am J Psychiatry 161:1715–1716
Lerum CW, LoBiondo-Wood G (1989) The relationship of maternal age, quickening, and physical symptoms of pregnancy to the development of maternal–fetal attachment. Birth 16:13–17
Lin HC, Chen IJ, Chen YH et al (2010) Maternal schizophrenia and pregnancy outcome: does the use of antipsychotics make a difference? Schizophr Res 116(1):55–60
Lindgren K (2001) Relationships among maternal-fetal attachment, prenatal depression, and health practices in pregnancy. Res Nurs Health 24(3):203–217
Maret SM (1989) Frank Lake’s maternal–fetal distress syndrome:—an analysis, Chap. 3, Caldwell University, Caldwell
Maskenzie TB, Nagel TC (1986) When a pregnant woman endangers her fetus. Hastings Center Report 16(1):24–25
McIntosh AM, Homes S, Gleeson S et al (2002) Maternal recall bias, obstetric history and schizophrenia. Br J Psychiatry 181:520–525
Miller LJ, Shah A (1999) Major mental illness during pregnancy. Primary Care Update for OB/GYNS 6(5, 10):163–168
Miller LJ (2007) Comprehensive care of pregnant mentally ill women. J Behav Health Serv Res
Miller LJ (1997) Sexuality, reproduction, and family planning in women with schizophrenia. Schizophr Bull 23(4):623–635
McK. Doan H, Cox NL et al (2003) The maternal fetal attachment scale: some methodological pondering. J Prenat Perinat Psychol Health 18(2):167–188
Muller ME (1993) Development of the prenatal attachment inventory. Western J Nurs Res 15:199–215
Nilsson E, Lichtenstein P, Cnattingius S et al (2002) Women with schizophrenia: pregnancy outcome and infant death among their offspring. Schizophr Res 58:221–229
Ogle A, Mazzullo L (2002) Before your pregnancy: a 90 day guide for couples on how to prepare for a healthy conception, Hardcover
Ostler T (2009) Mental illness in peripartum period. Zero to Three 29(5)
Pinkerton JV, Finerty JJ (1996) Resolving the clinical and ethical dilemmas involved in fetal–maternal conflicts. Am J Obstet Gynecol 175(2):289–295
Preti A, Cardascia L, Zen T et al (2000) Risk for obstetric complications and schizophrenia. Psychiatry Res 96(2):127–139
Righetti PL, Dell’Avanzo M, Grigio M et al (2005) Maternal/paternal antenatal attachment and fourth-dimensional ultrasound technique: a preliminary report. Br J Psychol 96(Pt 1):129–137
Riley D (1995) Perinatal mental health, Hardcover. Radcliffe Medical Press, Oxford
Salisbury A, Law K, LaGasse L et al (2003) Maternal–fetal attachment. JAMA 289:1701
Schneid-Kofman N, Sheiner E, Levy A (2008) Psychiatric illness and adverse pregnancy outcome. Int J Gynecol Obstet 101(1):53–56
Schubert EW, Blennow G, McNeil TF (1996) Wakefulness and arousal in neonates born to women with schizophrenia: diminished arousal and its association with neurological deviations. Schizophr Res 22(1):49–59
Spinelli MG (2004) Maternal infanticide associated with mental illness: prevention and the promise of saved lives. Am J Psychiatry 161:1548–1557
Susser ES, Gorman JM, Brown AS (1999) Prenatal exposures in schizophrenia, vol 56, Hardcover, American Psychiatric Publishing
Tsai-Ching L, Chin-Shyan C, Chung Ping AL (2009) Do children of parents with mental illness have lower survival rate? A population-based study. Comprehensive psychiatry (in press)
Van Bogaert LJ (2006) Rights of and duties to non-consenting patients—informed refusal in the developing world. Develop World Bioethics 6(1):13–22
Wan MW, Moulton S, Abel KM (2008) A review of mother–child relational interventions and their usefulness for mothers with schizophrenia. Arch Womens Mental Health 11(3):171–179
Yaeger D, Smith HG, Altshuler LL (2006) Atypical antipsychotics in the treatment of schizophrenia during pregnancy and the postpartum. Am J Psychiatry 163:2064–2070
Yarcheski A, Mahon NE, Yarcheski TJ et al (2009) A meta-analytic study of predictors of maternal-fetal attachment. Int J Nurs Studies 46(5):708–715
Yaris F, Yaris E, Kadioglu M et al (2004) Use of polypharmacotherapy in pregnancy: a prospective outcome in a case. Prog Neuropsychopharmacol Biol Psychiatry 28(3):603–605
Yun Y, Phillips LJ, Cotton S et al (2005) Obstetric complications and transition to psychosis in an ‘ultra’ high risk sample. Aust N Zealand J Psychiatry 39(6):460–466
Zammit S, Allebeck P, Dalman C et al (2003) Paternal age and risk for schizophrenia. Br J Psychiatry 183:405–408
Zammit S, Lewis S, Gunnell D (2007) Schizophrenia and neural tube defects: comparisons from an epidemiological perspective. Schizophr Bull 33(4):853–858
Zax M, Sameroff AJ, Babijian HM (1977) Birth outcomes in the offspring of mentally disordered women. Am J Orthopsychiatry 47(2):218–230
Zimerman A, Doan H, McK (2003) Prenatal attachment and other feelings and thoughts during pregnancy in three groups of pregnant women. J Prenatal Perinatal Psychol Health 18(2):131–148
Zipursky RB, Schulz SC (1987) Seasonality of birth and CT findings in schizophrenia. Biol Psychiatry 22(10):1288–1292
Zornberg GL, Buka SL, Tsuang MT (2000) The problem of obstetrical complications and schizophrenia. Schizophr Bull 26(2):249–256
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Matevosyan, N.R. Pregnancy and postpartum specifics in women with schizophrenia: a meta-study. Arch Gynecol Obstet 283, 141–147 (2011). https://doi.org/10.1007/s00404-010-1706-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-010-1706-8