Abstract
Purpose
Maternal schizophrenia is associated with adverse birth outcomes, but the reasons for this remain unclear. In a population-based cohort of infants born to women with schizophrenia, we determined the occurrence of key perinatal outcomes and explored whether factors identifiable in our datasets explained any elevated risk.
Methods
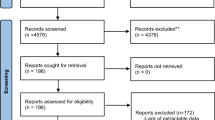
Using population-level health administrative data linked to clinical birth-registry data in Ontario, Canada (2006–2011), we examined the relative risk (RR) of preterm birth (< 37 weeks), small for gestational age (SGA), and Apgar scores < 8 in infants of women with schizophrenia (n = 4279) versus infants of unaffected women (n = 286,147). Generalized estimating equations determined whether reproductive history, maternal health conditions, pregnancy exposures, and complications explained elevated RRs.
Results
Among infants of women with schizophrenia, risk was higher for prematurity (11.4% vs. 6.9%, aRR 1.64, 95% CI 1.51–1.79), SGA (3.5% vs. 2.5%, aRR 1.40, 95% CI 1.20–1.64), and Apgar score < 8 at 1 (19.0% vs. 12.8%, aRR 1.49, 95% CI 1.40–1.59) and 5 min (5.6% vs. 3.0%, aRR 1.90, 95% CI 1.68–2.16). Smoking, fourfold more common among women with schizophrenia, was the variable that explained the greatest proportion of the elevated aRR for prematurity (9.9%), SGA (28.7%), and Apgar < 8 at 1 and 5 min (9.8%, 5.6%). Illicit substance use, certain reproductive history variables, and pregnancy complications also contributed to the elevated aRR for preterm birth.
Conclusions
Elevated risks of preterm birth, SGA, and low Apgar scores in infants of women with schizophrenia are partly explained by potentially modifiable factors such as smoking and illicit drug use, suggesting opportunities for targeted intervention.


Similar content being viewed by others
References
Bennedsen BE (1998) Adverse pregnancy outcome in schizophrenic women: occurrence and risk factors. Schizophr Res 33(1–2):1–26
Conde A et al (2010) Mother’s anxiety and depression and associated risk factors during early pregnancy: effects on fetal growth and activity at 20–22 weeks of gestation. J Psychosom Obstet Gynaecol 31(2):70–82
Judd F et al (2014) Adverse obstetric and neonatal outcomes in women with severe mental illness: to what extent can they be prevented? Schizophr Res 157(1–3):305–309
Vigod SN et al (2012) Temporal trends in general and age-specific fertility rates among women with schizophrenia (1996–2009): a population-based study in Ontario, Canada. Schizophr Res 139(1–3):169–175
Ng R et al (2015) Brain disorders in Ontario: prevalence, incidence and costs from health administrative data. Institute for Clinical Evaluative Sciences, Toronto, Ontario, Canada
Lasser K et al (2000) Smoking and mental illness: a population-based prevalence study. JAMA 284(20):2606–2610
Hudson CG (2005) Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am J Orthopsychiatr 75(1):3–18
Lin HC, Chen YH, Lee HC (2009) Prenatal care and adverse pregnancy outcomes among women with schizophrenia: a nationwide population-based study in Taiwan. J Clin Psychiatr 70(9):1297–1303
Buss C et al (2012) The Role of stress in brain development: the gestational environment’s long-term effects on the brain. Cerebrum 2012:4
Beijers R et al (2010) Maternal prenatal anxiety and stress predict infant illnesses and health complaints. Pediatrics 126(2):e401–e409
Dunkel Schetter C, Tanner L (2012) Anxiety, depression and stress in pregnancy: implications for mothers, children, research, and practice. Curr Opin Psychiatr 25(2):141–148
Williams J et al (1996) Patterns of health care in Ontario: the ICES Practice Atlas. Canadian Medical Association, Ottawa
Ray JG et al (2012) Birth weight curves tailored to maternal world region. J Obstet Gynaecol Can 34(2):159–171
Kurdyak P et al (2015) Validation of a population-based algorithm to detect chronic psychotic illness. Can J Psychiatr 60(8):362–368
Razaz N et al (2016) Five-minute Apgar score as a marker for developmental vulnerability at 5 years of age. Arch Dis Child Fetal Neonatal Ed 101(2):F114–F120
Health Canada, M.o.P.W.a.G.S.C. (2000) Perinatal health indicators for Canada: a resource manual, Ottawa
Ehrenstein V et al (2009) Association of Apgar score at 5 min with long-term neurologic disability and cognitive function in a prevalence study of Danish conscripts. BMC Pregnancy Childbirth 9:14
Urquia ML et al (2007) Birth outcomes by neighbourhood income and recent immigration in Toronto. Health Rep 18(4):21–30
Hux JE et al (2002) Diabetes in Ontario: determination of prevalence and incidence using a validated administrative data algorithm. Diabetes Care 25(3):512–516
Quan H et al (2009) Validation of a case definition to define hypertension using administrative data. Hypertension 54(6):1423–1428
McCarthy J, Maine D (1992) A framework for analyzing the determinants of maternal mortality. Stud Fam Plann 23(1):23–33
Saccone G, Perriera L, Berghella V (2016) Prior uterine evacuation of pregnancy as independent risk factor for preterm birth: a systematic review and metaanalysis. Am J Obstet Gynecol 214(5):572–591
Steer P (2005) The epidemiology of preterm labour. BJOG 112(Suppl 1):1–3
Gravett MG et al (2010) Global report on preterm birth and stillbirth (2 of 7): discovery science. BMC Pregnancy Childbirth 10(Suppl 1):S2
Sheehan PM et al (2015) Maternal thyroid disease and preterm birth: systematic review and meta-analysis. J Clin Endocrinol Metab 100(11):4325–4331
Aagaard-Tillery KM et al (2008) In utero tobacco exposure is associated with modified effects of maternal factors on fetal growth. Am J Obstet Gynecol 198(1):66.e1–66.e6
Patra J et al (2011) Dose-response relationship between alcohol consumption before and during pregnancy and the risks of low birthweight, preterm birth and small for gestational age (SGA)-a systematic review and meta-analyses. BJOG 118(12):1411–1421
Maeda A et al (2014) Opioid abuse and dependence during pregnancy: temporal trends and obstetrical outcomes. Anesthesiology 121(6):1158–1165
Gouin K et al (2011) Effects of cocaine use during pregnancy on low birthweight and preterm birth: systematic review and metaanalyses. Am J Obstet Gynecol 204(4):340.e1–340.e12
Gorman MC et al (2014) Outcomes in pregnancies complicated by methamphetamine use. Am J Obstet Gynecol 211(4):429.e1–429.e7
Hingson R et al (1982) Maternal cigarette smoking, psychoactive substance use, and infant Apgar scores. Am J Obstet Gynecol 144(8):959–966
Vahanian SA et al (2015) Placental implantation abnormalities and risk of preterm delivery: a systematic review and metaanalysis. Am J Obstet Gynecol 213(4 Suppl):S78–S90
Ananth CV et al (1999) Placental abruption and adverse perinatal outcomes. JAMA 282(17):1646–1651
Zou G (2004) A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 159(7):702–706
Schluchter MD (2008) Flexible approaches to computing mediated effects in generalized linear models: generalized estimating equations and bootstrapping. Multivariate Behav Res 43(2):268–288
Bennedsen BE et al (1999) Preterm birth and intra-uterine growth retardation among children of women with schizophrenia. Br J Psychiatr 175:239–245
Bennedsen BE et al (2001) Obstetric complications in women with schizophrenia. Schizophr Res 47(2–3):167–175
Nilsson E et al (2002) Women with schizophrenia: pregnancy outcome and infant death among their offspring. Schizophr Res 58(2–3):221–229
Zhong QY et al (2018) Adverse obstetric and neonatal outcomes complicated by psychosis among pregnant women in the United States. BMC Pregnancy Childbirth 18(1):120
Lee HC, Lin HC (2010) Maternal bipolar disorder increased low birthweight and preterm births: a nationwide population-based study. J Affect Disord 121(1–2):100–105
Nguyen TN et al (2013) Obstetric and neonatal outcomes of pregnant women with severe mental illness at a specialist antenatal clinic. Med J Aust 199(3 Suppl):S26–S29
Schneid-Kofman N, Sheiner E, Levy A (2008) Psychiatric illness and adverse pregnancy outcome. Int J Gynaecol Obstet 101(1):53–56
Vigod SN et al (2014) Maternal and newborn outcomes among women with schizophrenia: a retrospective population-based cohort study. BJOG 121(5):566–574
Matevosyan NR (2011) Pregnancy and postpartum specifics in women with schizophrenia: a meta-study. Arch Gynecol Obstet 283(2):141–147
Simoila L et al (2018) Obstetric and perinatal health outcomes related to schizophrenia: a national register-based follow-up study among Finnish women born between 1965 and 1980 and their offspring. Eur Psychiatr 52:68–75
Jablensky AV et al (2005) Pregnancy, delivery, and neonatal complications in a population cohort of women with schizophrenia and major affective disorders. Am J Psychiatr 162(1):79–91
Berger H et al (2016) Diabetes in pregnancy. J Obstet Gynaecol Can 38(7):667
Butalia S et al (2018) Hypertension Canada’s 2018 guidelines for the management of hypertension in pregnancy. Can J Cardiol 34(5):526–531
Association A. D (2018) Management of diabetes in pregnancy. Diabetes Care 41(Suppl 1):S137–S143
Bérard A, Zhao JP, Sheehy O (2016) Success of smoking cessation interventions during pregnancy. Am J Obstet Gynecol 215(5):611.e1–611.e8
Hand DJ et al (2017) Contingency management interventions for tobacco and other substance use disorders in pregnancy. Psychol Addict Behav 31(8):907–921
Oncken C et al (2008) Nicotine gum for pregnant smokers: a randomized controlled trial. Obstet Gynecol 112(4):859–867
Wisborg K et al (2000) Nicotine patches for pregnant smokers: a randomized controlled study. Obstet Gynecol 96(6):967–971
Kilbourne AM et al (2014) SMI life goals: description of a randomized trial of a collaborative care model to improve outcomes for persons with serious mental illness. Contemp Clin Trials 39(1):74–85
Vaez K et al (2017) Evaluating diabetes care for patients with serious mental illness using the chronic care model: a pilot study. Health Serv Res Manag Epidemiol 4:2333392817734206
Dickerson F et al (2013) Cigarette smoking among persons with schizophrenia or bipolar disorder in routine clinical settings, 1999-2011. Psychiatr Serv 64(1):44–50
Faulkner G, Cohn T, Remington G (2007) Interventions to reduce weight gain in schizophrenia. Cochrane Database Syst Rev 1:CD005148
Gilbody S et al (2015) Bespoke smoking cessation for people with severe mental ill health (SCIMITAR): a pilot randomised controlled trial. Lancet Psychiatr 2(5):395–402
Hauck Y et al (2008) Healthy babies for mothers with serious mental illness: a case management framework for mental health clinicians. Int J Ment Health Nurs 17(6):383–391
Tsoi DT, Porwal M, Webster AC (2013) Interventions for smoking cessation and reduction in individuals with schizophrenia. Cochrane Database Syst Rev 2:CD007253
Bennett ME, Bradshaw KR, Catalano LT (2017) Treatment of substance use disorders in schizophrenia. Am J Drug Alcohol Abuse 43(4):377–390
Seeman MV (2008) Prevention inherent in services for women with schizophrenia. Can J Psychiatry 53(5):332–341
Hoirisch-Clapauch S, Nardi AE (2014) Markers of low activity of tissue plasminogen activator/plasmin are prevalent in schizophrenia patients. Schizophr Res 159(1):118–123
Hoirisch-Clapauch S, Brenner B, Nardi AE (2015) Adverse obstetric and neonatal outcomes in women with mental disorders. Thromb Res 135(Suppl 1):S60–S63
Mittal VA, Ellman LM, Cannon TD (2008) Gene-environment interaction and covariation in schizophrenia: the role of obstetric complications. Schizophr Bull 34(6):1083–1094
Suvisaari JM et al (2013) Obstetric complications as risk factors for schizophrenia spectrum psychoses in offspring of mothers with psychotic disorder. Schizophr Bull 39(5):1056–1066
Mei-Dan E, Ray JG, Vigod SN (2015) Perinatal outcomes among women with bipolar disorder: a population-based cohort study. Am J Obstet Gynecol 212(3):367e1–367e8
Acknowledgements
We thank the Ontario Ministry of Health and Long-Term Care for their data. Parts of this material are based on data and/or information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of the CIHI. This study is based in part on data provided by Better Outcomes Registry and Network (“BORN”), part of the Children’s Hospital of Eastern Ontario. The interpretation and conclusions contained herein do not necessarily represent those of BORN Ontario.
Funding
This work was supported by the ICES, which is funded by an annual Grant from the MOHLTC. It was also supported by the Mental Health and Addictions Scorecard and Evaluation Framework Grant from the MOHLTC (Grant number 04601A14-19). The opinions, results, and conclusions reported in this paper are those of the authors and are independent from the funding sources. No endorsement by ICES or the Ontario MOHLTC is intended or should be inferred.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
In terms of author disclosures, Dr. Vigod receives royalties for authorship of chapters related to depression and pregnancy from UpToDate Inc. The other authors have declared that there are no conflicts of interest in relation to the subject of this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vigod, S.N., Fung, K., Amartey, A. et al. Maternal schizophrenia and adverse birth outcomes: what mediates the risk?. Soc Psychiatry Psychiatr Epidemiol 55, 561–570 (2020). https://doi.org/10.1007/s00127-019-01814-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-019-01814-7