Abstract
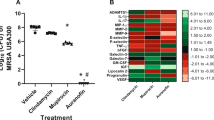
The topical application of a mixture of sugar and povidone-iodine (PI) has been reported to accelerate the healing of cutaneous wounds and ulcers by promoting reepithelialization and granulation tissue formation, as well as by having an anti-microbial effect. In order to clarify the efficacy of a 70% sugar and 3% PI paste (U-PASTA™)(SP) on infectious skin ulcers, we made a bacterial infection model using methicillin-resistant Staphylococcus aureus (MRSA) on the skin of diabetic db/db mice, and investigated the effect of the paste on the healing process of wounds. Full-thickness wounds were made on the backs of female diabetic mice, (C57BL/ksJ db/db) and inoculated with S. aureus. SP was applied to the closed wounds for 8 days. The degree of repair was evaluated using three histological parameters: The degree of reepithelialization was given a percentage value of 0–100%; the amount of granulation tissue was quantified by measuring the area of granulation (mm2); and the number of capillary lumens in the granulation tissue was counted in the complete wound cross-section at 100× magnification. In addition, the colony-forming units (CFU) of MRSA on the wounds were counted. Continuous MRSA infection in the wounds of db/db mice was demonstrated with macroscopic and histopathological images. Wounding and infection caused by MRSA on the back of the diabetic mice significantly induced delayed reepithelialization, granulation tissue formation with inflammatory cell infiltrate and increased CFU on wounds (P < 0.01, respectively) compared to those of the MRSA-infected normal mice. Application of SP significantly accelerated reepithelialization (P < 0.01) and decreased CFU (P < 0.05) of the ulcers in the MRSA-infected wounds, compared to the non-treated group. Histopathological evaluation and CFU on this animal model revealed no significant difference between Methicilin-sensitive Staphylococcus aureus and MRSA infection. These results indicate that wounding on db/db mice provides a useful animal model of bacterial skin infections, and that SP is an effective topical agent for the treatment of diabetic skin ulcers.






Similar content being viewed by others
Abbreviations
- PI:
-
Povidone-iodine
- SP:
-
A paste comprising 70% sugar and 3% PI
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MSSA:
-
Methicilin-sensitive Staphylococcus aureus
- CFU:
-
Colony-forming units
- PBS:
-
Phosphate buffered saline
References
Addison MK, Walterspiel JN (1985) Sugar and wound healing. Lancet ii:663–664
Akiyama H, Huh WK, Yamasaki O, Oono T, Iwatsuki K (2002) Confocal laser scanning microscopic observation of glycocalyx production by Staphylococcus aureus in mouse skin: does S. aureus generally produce a biofilm on damaged skin? Br J Dermatol 147:879–885
Akiyama H, Oono T, Saito M, Iwatsuki K (2004) Assessment of cadexomer iodine against Staphylococcus aureus biofilm in vivo and in vitro using confocal laser scanning microscopy. J Dermatol 31:529–534
Anania WC, Rosen RC, Wallace JA, Weinblatt MA, Gerland JS, Castillo J (1985) Treatment of diabetic skin ulcerations with povidone-iodine and sugar. J Am Podiatr Med Assoc 75:472–474
Bianchi J (2001) Cadexomer-iodine in the treatment of venous leg ulcers: what is the evidence? J Wound Care 10:225–229
Breuing K, Kaplan S, Liu P, Onderdonk AB, Eriksson E (2003) Wound fluid bacterial levels exceed tissue bacterial counts in controlled porcine partial-thickness burn infections. Plast Reconstr Surg 111:781–788
Burks RI (1998) Povidone-iodine solution in wound treatment. Phys Ther 78:212–218
Clark RA (1993) Basics of cutaneous wound repair. J Dermatol Surg Oncol 19:693–706
Danielsen L, Cherry GW, Harding K, Rollman O (1997) Cadexomer iodine in ulcers colonised by Pseudomonas aeruginosa. J Wound Care 6:169–172
Eto Y, Matsumoto J, Akiba T, Wada Y, Nagakura M, Nakamura M (1989) The healing effect of KT-136 on incised and open wounds in rats. Jpn Pharmcol Ther 17(Suppl 1):7–13 (in Japanese)
Gordon H, Middleton K, Seal D, Sullens K (1985) Sugar and wound healing (letter). Lancet 2:663–664
Heggers J, Goodheart RE, Washington J, McCoy L, Carino E, Dang T, Edgar P, Maness C, Chinkes D (2005) Therapeutic efficacy of three silver dressings in an infected animal model. J Burn Care Rehabil 26:53–56
Keith JF, Knodel L (1988) Sugar in wound healing. Drug Intell Clin Pharm 22:409–411
Knutson RA, Merbitz LA, Creekmore MA, Snipes HG (1981) Use of sugar and povidone-iodine to enhance wound healing: five years’ experience. South Med J 74:1329–1335
Lamme EN, Gustafsson TO, Middelkoop E (1998) Cadexomer-iodine ointment shows stimulation of epidermal regeneration in experimental full-thickness wounds. Arch Dermatol Res 290:18–24
Mayer DA, Tsapogas MJ (1993) Povidone-iodine and wound healing: a critical review. Wounds 5:14–23
Miyachi Y, Imamura S (1990) Use of sugar and povidone-iodine in the treatment of refractory cutaneous ulcers. J Dermatol Treat 1:191–193
Miyachi Y, Imamura S (1991) Improved healing of pressure sores with sugar and povidone-iodine. Ther Res 49:81–87
Mueller S, Vogt PM, Steinau HU, Leuner C, Hopp M, Bosse B, Fleischer W, Reimer K (2006) Repithel®: removing the barriers to wound healing. Dermatology 212(Suppl 1):77–81
Nakao H, Yamazaki M, Tsuboi R, Ogawa H (2006) Mixture of sugar and povidone-iodine stimulates wound healing by activating keratinocytes and fibroblast functions. Arch Dermatol Res 298:175–182
Shi CM, Takimoto R, Tsuboi R, Ogawa H (1996) Topical application of sugar and povidone iodine stimulates wound healing in diabetic mice. Jpn J Dermatol 106:403–408 (in Japanese)
Shiraishi T, Oka R, Nakagawa Y (1997) Pharmaceutical and bacteriological study on povidone-iodine sugar ointment. Dermatology 195(Suppl 2):100–103
Stepinska M, Grzybowski J, Struzyna J, Olszowska M, Jablonska H, Chomicka M, Chomiczewski K (1995) Mouse model of infected wound. Acta Microbiol Pol 44:39–46
Tachi M, Hirabayashi S, Yonehara Y, Suzuki Y, Bowler P (2004) Development of an experimental model of infected skin ulcer. Int Wound J 1:49–55
Topham J (1996) Sugar paste and povidone-iodine in the treatment of wounds. J Wound Care 5:364–365
Tsuboi R, Rifkin DB (1990) Recombinant basic fibroblast growth factor stimulates wound healing in healing-impaired db/db mice. J Exp Med 172:245–251
Tsuboi R, Shi CM, Rifkin DB, Ogawa H (1992) A wound healing model using healing-impared diabetic mice. J Dermatol 19:673–675
Tsuboi R, Shi CM, Sato C, Cox GN, Ogawa H (1995) Co-administration of insulin-like growth factor (IGF)-I and IGF-binding protein-1 stimulates wound healing in animal models. J Invest Dermatol 104:199–203
Zhou LH, Nahm WK, Badiavas E, Yufit T, Falanga V (2002) Slow release iodine preparation and wound healing: in vitro effects consistent with lack of in vivo toxicity in human chronic wounds. Br J Dermatol 146:365–374
Acknowledgments
We thank Prof. Keiichi Hiramatsu of the Department of Microbiology, Juntendo University School of Medicine for the gift of MRSA(N315 PZR) and MSSA (N315 P). Rooms for the infection experiment were provided by Kowa Research Institute, Kowa Company Ltd., 1-25-5 Kannondai, Tsukuba, Japan. This work was supported by High-Tech Research Center Project for private universities. A matching fund subsidy was provided by the MEXT (Ministry of Education, Culture, Sports, Science and Technology of Japan, 2003–2007) (RT).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shi, CM., Nakao, H., Yamazaki, M. et al. Mixture of sugar and povidone-iodine stimulates healing of MRSA-infected skin ulcers on db/db mice. Arch Dermatol Res 299, 449–456 (2007). https://doi.org/10.1007/s00403-007-0776-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00403-007-0776-3