Abstract
Objective
To determine whether the effects of intensive (< 120 mmHg) compared with standard (< 140 mmHg) systolic blood pressure (SBP) treatments are different among those with different baseline SBP.
Methods
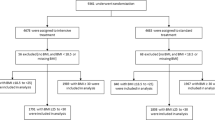
De-identified SPRINT database was used for this post hoc analysis. SPRINT participants were categorized by baseline SBP status, defined as high-SBP (≥ 140 mmHg) group versus the low-SBP (< 140 mmHg) group. The primary outcome was a composite of myocardial infarction, acute coronary syndrome not resulting in myocardial infarction, stroke, acute decompensated heart failure, or death from cardiovascular causes. Treatment-related adverse events including hypotension, syncope, and bradycardia were also evaluated. Cox regression was used to calculate hazard ratios for study outcomes with intensive compared with standard SBP treatment between these two groups.
Results
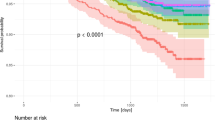
Among 9361 participants randomized (age 67.9 ± 9.4 years; 35.5% female), 4964 and 4397 had baseline low SBP (< 140 mmHg) and high SBP (≥ 140 mmHg), respectively. After a median follow-up of 3.26 years, the hazard ratio for the primary outcome was 0.65 (95% CI 0.50, 0.83) and 0.84 (95% CI 0.66, 1.06) among those in the low-SBP group and high-SBP group, respectively (P value for interaction 0.15). For treatment-related adverse events, the hazard ratio with intensive SBP treatment was 2.03 (95% CI 1.44, 2.85) for the low-SBP group and 1.80 (95% CI 1.32, 2.47) for the high-SBP group (P value for interaction 0.28).
Conclusions
Hypertensive patients with low baseline SBP may benefit from intensive SBP lowering, whereas benefits were inconclusive among those with high baseline SBP.


Similar content being viewed by others
References
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J (2005) Global burden of hypertension: analysis of worldwide data. Lancet 365(9455):217–223. https://doi.org/10.1016/S0140-6736(05)17741-1
Liu FD, Shen XL, Zhao R et al. Pulse pressure as an independent predictor of stroke: a systematic review and a meta-analysis. Clin Res Cardiol 2016;105(8): 677–686. https://doi.org/10.1007/s00392-016-0972-2
Collins R, Peto R, Macmahon S, Hebert P (1990) et al. Blood pressure, stroke, and coronary heart disease. Part 2, short-term reduction in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet 335:827–838
Sundstr MJ, Arima H, Woodward M et al (2014) Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet 384(9943):591–598. https://doi.org/10.1016/S0140-6736(14)61212-5
Turnbull F (2003) Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 362(9395):1527–1535. https://doi.org/10.1016/S0140-6736(03)14739-3
Kulenthiran S, Ewen S, Böhm M et al (2017) Hypertension up to date: SPRINT to SPYRAL. Clin Res Cardiol 106(7):475–484. https://doi.org/10.1007/s00392-017-1095-0
Bohm M, Schumacher H, Teo KK et al (2017) Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet 389(10085):2226–2237. https://doi.org/10.1016/S0140-6736(17)30754-7
Cotter G, Davison BA, Butler J et al (2018) Relationship between baseline systolic blood pressure and long-term outcomes in acute heart failure patients treated with TRV027: an exploratory subgroup analysis of BLAST-AHF. Clin Res Cardiol 107(2):170–181. https://doi.org/10.1007/s00392-017-1168-0
Wang TD, Lin HJ, Chen WJ, Weng TC, Shau WY (2017) Increased all-cause mortality with intensive blood-pressure control in patients with a baseline systolic blood pressure of ≥ 160 mmHg and a Lower Framingham risk score: a cautionary note from SPRINT. In: Presentation at: annual meeting of the European Society of Cardiology, August 28, 2017, Barcelona
Group TSR (2015) A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 373(22):2103–2116. https://doi.org/10.1056/NEJMoa1511939
Ambrosius WT, Sink KM, Foy CG et al (2014) The design and rationale of a multicenter clinical trial comparing two strategies for control of systolic blood pressure: the systolic blood pressure intervention trial (SPRINT). Clin Trials 11(5):532–546. https://doi.org/10.1177/1740774514537404
Kajimoto K, Sato N, Takano T (2015) Association of age and baseline systolic blood pressure with outcomes in patients hospitalized for acute heart failure syndromes. Int J Cardiol 191:100–106. https://doi.org/10.1016/j.ijcard.2015.04.258
Weiner DE, Gaussoin SA, Nord J et al (2017) Cognitive function and kidney disease: baseline data from the systolic blood pressure intervention trial (SPRINT). Am J Kidney Dis 70(3):357–367. https://doi.org/10.1053/j.ajkd.2017.04.021
Williamson JD, Supiano MA, Applegate WB et al (2016) Intensive vs standard blood pressure control and cardiovascular disease outcomes in adults aged ≥ 75 years. JAMA 315(24):2673–2682. https://doi.org/10.1001/jama.2016.7050
Bress AP, King JB, Kreider KE et al (2017) Effect of intensive versus standard blood pressure treatment according to baseline prediabetes status: a post hoc analysis of a randomized trial. Diabetes Care. https://doi.org/10.2337/dc17-0885
Obi Y, Kalantar-Zadeh K, Shintani A, Kovesdy CP, Hamano T (2018) Estimated glomerular filtration rate and the risk-benefit profile of intensive blood pressure control amongst nondiabetic patients: a post hoc analysis of a randomized clinical trial. J Intern Med 283(3):314–327. https://doi.org/10.1111/joim.12701
Zanchetti A, Grassi G, Mancia G (2009) When should antihypertensive drug treatment be initiated and to what levels should systolic blood pressure be lowered? A critical reappraisal. J Hypertens 27:923–934. https://doi.org/10.1097/HJH.0b013e32832aa6b5
Srinivasan B, Glenn MC, Alfred K, Cheung et al (2017) Influence of baseline diastolic blood pressure on effects of intensive compared to standard blood pressure control. Circulation 137(2):134–143. https://doi.org/10.1161/CIRCULATIONAHA.117.030848
Brunström M, Carlberg B (2017) Association of blood pressure lowering with mortality and cardiovascular disease across blood pressure levels. JAMA Intern Med 177(10):1498–1505. https://doi.org/10.1001/jamainternmed.2017.4377
Group AS, Cushman WC, Evans GW, Byington RP, Goff D Jr (2010) Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med 362(17):1575–1585. https://doi.org/10.1056/NEJMoa1001286
Waits GS, O’Neal WT, Sandesara PB, Li Y, Shah AJ, Soliman EZ (2018) Association between low diastolic blood pressure and subclinical myocardial injury. Clin Res Cardiol 107(4):312–318. https://doi.org/10.1007/s00392-017-1184-0
Mancia G, Kjeldsen SE, Zappe DH, Holzhauer B, Hua TA (2016) Cardiovascular outcomes at different on-treatment blood pressures in the hypertensive patients of the VALUE trial. Eur Heart J. 37:955–964. https://doi.org/10.1093/eurheartj/ehv633
Thomopoulos C, Parati G, Zanchetti A (2014) Effects of blood pressure lowering on outcome incidence in hypertension. J Hypertens 32(12):2296–2304. https://doi.org/10.1097/HJH.0000000000000379
Nishikawa T, Ueba T, Kajiwara M, Iwata R, Miyamatsu N, Yamashita K (2010) Preventive effect of aggressive blood pressure lowering on hematoma enlargement in patients with ultra-acute intracerebral hemorrhage. Neurol Med Chir (Tokyo) 50(11):966–971. https://doi.org/10.2176/nmc.50.966
Sakamoto Y, Koga M, Todo K et al (2015) Relative systolic blood pressure reduction and clinical outcomes in hyperacute intracerebral hemorrhage. J Hypertens 33(5):1069–1073. https://doi.org/10.1097/HJH.0000000000000512
Anderson CS, Selim MH, Molina CA, Qureshi AI (2017) Intensive blood pressure lowering in intracerebral hemorrhage. Stroke 48:2034–2037. https://doi.org/10.1161/STROKEAHA.117.016185
Cushman WC, Whelton PK, Fine LJ et al (2015) SPRINT trial results latest news in hypertension management. Hypertension 2(67):263–265. https://doi.org/10.1161/HYPERTENSIONAHA.115.06722
Bress AP, Tanner RM, Hess R, Colantonio LD, Shimbo D, Muntner P (2016) Generalizability of SPRINT results to the U.S. adult population. J Am Coll Cardiol 67(5):463–472. https://doi.org/10.1016/j.jacc.2015.10.037
Bhatt H, Ghazi L, Calhoun D, Oparil S (2016) BP targets in hypertension: what should we do now that SPRINT is out? Curr Cardiol Rep 18(10):98. https://doi.org/10.1007/s11886-016-0775-0
Jones DW, Weatherly L, Hall JE (2016) SPRINT what remains unanswered and where do we go from here? Hypertension 67:261–262. https://doi.org/10.1161/HYPERTENSIONAHA.115.06723
Sakamoto Y, Koga M, Yamagami H et al (2013) Systolic blood pressure after intravenous antihypertensive treatment and clinical outcomes in hyperacute intracerebral hemorrhage: the stroke acute management with urgent risk-factor assessment and improvement-intracerebral hemorrhage study. Stroke 44(7):1846–1851. https://doi.org/10.1161/STROKEAHA.113.001212
Verdecchia P, Angeli F, Mazzotta G, Garofoli M, Reboldi G (2013) aggressive blood pressure lowering is dangerous: the J-curve: con side of the argument. Hypertension 63(1):37–40. https://doi.org/10.1161/HYPERTENSIONAHA.113.01018
Whelton PK, Carey RM, Aronow WS et al (2017) 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol 71(19):e127–e248. https://doi.org/10.1016/j.jacc.2017.11.006
Reboldi G, Angeli F, de Simone G, Staessen JA, Verdecchia P (2014) Tight versus standard blood pressure control in patients with hypertension with and without cardiovascular disease. Hypertension 63(3):475–482. https://doi.org/10.1161/HYPERTENSIONAHA.113.02089
Bundy JD, Li C, Stuchlik P et al (2017) Systolic blood pressure reduction and risk of cardiovascular disease and mortality. JAMA Cardiol 2(7):775–781. https://doi.org/10.1001/jamacardio.2017.1421
Ettehad D, Emdin CA, Kiran A et al (2016) Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 387(10022):957–967. https://doi.org/10.1016/S0140-6736(15)01225-8
De Jager RL, Sanders MF, Bots ML et al. Renal denervation in hypertensive patients not on blood pressure lowering drugs. Clin Res Cardiol 2016;105(9): 755–762. https://doi.org/10.1007/s00392-016-0984-y
Stoiber L, Mahfoud F, Zamani SM et al (2018) Renal sympathetic denervation restores aortic distensibility in patients with resistant hypertension: data from a multi-center trial. Clin Res Cardiol. https://doi.org/10.1007/s00392-018-1229-z (Epub ahead of print)
Funding
This study was supported by the Natural Science Foundation of Guangdong Province (2016A030310140/20160903) to LXX, and the Natural Science Foundations of China (Grant no. 81600206) to ZXD.
Author information
Authors and Affiliations
Contributions
LXX and ZXX had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: LXX, ZXD, SXT, GY, DZM. Acquisition, analysis, or interpretation of data: NZQ, SXT, ZSZ, ZHM, DZM. Drafting of the manuscript: ZXD, LXX, SXT. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: NZQ, SXT, ZXB. Obtained funding: LXX, ZXD. Administrative, technical, or material support: ZXD.
Corresponding authors
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Rights and permissions
About this article
Cite this article
Sun, X., Guo, Y., Nie, Z. et al. Influence of baseline systolic blood pressure on the relationship between intensive blood pressure control and cardiovascular outcomes in the Systolic Blood Pressure Intervention Trial (SPRINT). Clin Res Cardiol 108, 273–281 (2019). https://doi.org/10.1007/s00392-018-1353-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-018-1353-9