Abstract
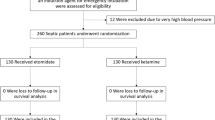
We investigated the incidence of post-intubation hypotension (PIH) in hemodynamically stable patients with STEMI requiring rapid sequences intubation (RSI) and medicated with ketamine or midazolam as induction agent. STEMI patients admitted between 1st January 2009 and 1st January 2017 who did not receive any type of inotropic support before the endotracheal intubation (ETI) was reviewed. PIH was defined as a reduction greater than 20% or a drop of systolic blood pressure (SBP) below 90 mmHg within 10 min from the administration of the induction agent [ketamine (1 mg/kg) or midazolam (0.3 mg/kg)]. Over the study period, 136 patients (66 male and 70 females, mean age 72.25 ± 7.33 years) met the inclusion criteria. Patients treated with midazolam and ketamine were 63 and 73, respectively. PIH was observed in 38 (27.9%) patients after 10 min from ETI. Midazolam patients had a significant lower SBP at both 5 and 10 min after induction (97.75 ± 8.06 vs 100.81 ± 8.08, p = 0.029 and 92.83 ± 7.53 vs 101.58 ± 7.29, p < 0.0001, respectively) (ANOVA p < 0.0001). Age (OR 1.91, 95% CI 1.87–1.97, p = 0.001), history of arterial hypertension (OR 2.27, 95% CI 2.21–2.35, p = 0.0001), multivessel coronary artery disease (OR 2.66, 95% CI 2.58–2.71, p = 0.001), SI ≥0.9 (OR 2.41, 95% CI 2.36–2.48, p < 0.0001) and anterior STEMI (OR 2.51, 95% CI 2.48–2.57, p = 0.0001) resulted independent predictors of PIH in STEMI patients treated with midazolam, as induction agent, before ETI. Midazolam was more likely than ketamine to cause significant PIH when used as an induction agent for RSI in hemodynamically stable patients with STEMI.





Similar content being viewed by others
References
Metkus TS, Albaeni A, Chandra-Strobos N, Eid SM (2017) Incidence and prognostic impact of respiratory support in patients with ST-segment elevation myocardial infarction. Am J Cardiol 119:171–177
Lee WC, Fang HY, Chen HC, Hsueh SK, Chen CJ, Yang CH, Yip HK, Hang CL, Wu CJ, Fang CY (2017) Effect of improved door-to-balloon time on clinical outcomes in patients with ST segment elevation myocardial infarction. Int J Cardiol 240:66–71
Pesaro AE, Katz M, Katz JN, Barbas CS, Makdisse MR, Correa AG, Franken M, Pereira C, Serrano CV Jr, Lopes RD (2016) Mechanical ventilation and clinical outcomes in patients with acute myocardial infarction: a retrospective observational study. PLoS ONE 11:e0151302
Lazzeri C, Valente S, Chiostri M, Attanà P, Mattesini A, Gensini GF (2013) Mechanical ventilation in the early phase of ST elevation myocardial infarction treated with mechanical revascularization. Cardiol J 20:612–617
Mort TC (2007) Complications of emergency tracheal intubation: hemodynamic alterations—part I. J Intensive Care Med 22:157–165
Heffner AC, Swords D, Kline JA, Jones AE (2012) The frequency and significance of postintubation hypotension during emergency airway management. J Crit Care 27:417e9–417e13
Smischney NJ, Ricter BD, Hoeft CC, Johnson LM, Ansar S, Kashyap R (2014) Association of post-intubation hemodynamic instability in an adult ICU with in-hospital mortality and ICU length of stay. Am J Respir Crit Care Med 189:A4558
Franklin C, Samuel J, Hu TC (1994) Life-threatening hypotension associated with emergency intubation and the initiation of mechanical ventilation. Am J Emerg Med 12:425–428
Stolfo D, Cinquetti M, Merlo M, Santangelo S, Barbati G, Alonge M, Vitrella G, Rakar S, Salvi A, Perkan A, Sinagra G (2016) ST-elevation myocardial infarction with reduced left ventricular ejection fraction: insights into persisting left ventricular dysfunction. A pPCI-registry analysis. Int J Cardiol 15(215):340–345
Choi Y, Wong T, Lau C (2004) Midazolam is more likely to cause hypotension than etomidate in emergency department rapid sequence intubation. Emerg Med J 21:700–702
Yoon SH (2012) Concerns of the anesthesiologist: anesthetic induction in severe sepsis or septic shock patients. Korean J Anesthesiol 63:3–10
Zuin M, Rigatelli G, Picariello C, dell’Avvocata F, Marcantoni L, Pastore G, Carraro M, Nanjundappa A, Faggian G, Roncon L (2017) Correlation and prognostic role of neutrophil to lymphocyte ratio and SYNTAX score in patients with acute myocardial infarction treated with percutaneous coronary intervention: a six-year experience. Cardiovasc Revasc Med. doi:10.1016/j.carrev.2017.05.007
Katz RI, Levy A, Slepian B, Sobel B, Lagasse RS (1998) Haemodynamic stability and ketamine-alfentanil anaesthetic induction. Br J Anaesth 81:702–706
Zed PJ, Abu-Laban RB, Harrison DW (2006) Intubating conditions and hemodynamic effects of etomidate for rapid sequence intubation in the emergence department: an observational cohort study. Acad Emerg Med 13:378–383
Sivilotti ML, Ducharme J (1998) Randomized, double-blind study on sedatives and hemodynamics during rapid-sequence intubation in the emergency department: the SHRED study. Ann Emerg Med 31:313–324
Green RS, Edwards J, Sabri E, Fergusson D (2012) Evaluation of the incidence, risk factors, and impact on patient outcomes of postintubation hemodynamic instability. CJEM 14:74–82
Smischney NJ, Demirci O, Diedrich DA, Barbara DW, Sandefur BJ, Trivedi S, McGarry S, Kashyap R (2016) Incidence of and risk factors for post-intubation hypotension in the critically ill. Med Sci Monit 22:346–355
Jaber S, Amraoui J, Lefrant JY, Arich C, Cohendy R, Landreau L, Calvet Y, Capdevila X, Mahamat A, Eledjam JJ (2006) Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med 34:2355–2361
Green R, Hutton B, Lorette J, Bleskie D, McIntyre L, Fergusson D (2014) Incidence of postintubation hemodynamic instability associated with emergent intubations performed outside the operating room: a systematic review. CJEM 16:69–79
Lin CC, Chen KF, Shih CP, Seak CJ, Hsu KH (2008) The prognostic factors of hypotension after rapid sequence intubation. Am J Emerg Med 26:845–851
Heffner AC, Swords DS, Nussbaum ML, Kline JA, Jones AE (2012) Predictors of the complication of postintubation hypotension during emergency airway management. J Crit Care 27:587–593
Scherzer D, Leder M, Tobias JD (2012) Pro-con debate: etomidate or ketamine for rapid sequence intubation in pediatric patients. J Pediatr Pharmacol Ther 17(2):142–149
Fleg JL (2012) Age-associated changes in cardiovascular structure and function: a fertile milieu for future disease. Heart Fail Rev 17:545–554
Behar S, Rabinowitz B, Zion M, Reicher-Reiss H, Kaplinsky E, Abinader E, Agmon J, Friedman Y, Kishon Y, Palant A, Peled B, Reisin L, Schlesinger Z, Zahavi I, Goldbourt U (1993) Immediate and long-term prognostic significance of a first anterior versus first inferior wall Q-wave acute myocardial infarction. Secondary Prevention Reinfarction Israeli Nifedipine Trial (SPRINT) study group. Am J Cardiol 72:1366–1370
Squeri A, Gaibazzi N, Reverberi C, Caracciolo MM, Ardissino D, Gherli T (2012) Ejection fraction change and coronary artery disease severity: a vasodilator contrast stress-echocardiography study. J Am Soc Echocardiogr 25:454–459
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflict of interest to declare.
Rights and permissions
About this article
Cite this article
Zuin, M., Rigatelli, G., Dell’Avvocata, F. et al. Ketamine and midazolam differently impact post-intubation hemodynamic profile when used as induction agents during emergency airway management in hemodynamically stable patients with ST elevation myocardial infarction. Heart Vessels 33, 213–225 (2018). https://doi.org/10.1007/s00380-017-1049-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-1049-5