Abstract
Purpose
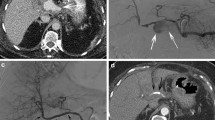
Hepatic artery pseudoaneurysms are a rare but potentially life-threatening complication of major pancreaticobiliary surgery. We evaluated the safety and efficacy of endovascular stentgraft implantation for the management of such vascular lesions.
Materials and Methods
Between May 2013 and October 2015, ten patients with postoperative hepatic artery pseudoaneurysm, of which eight presented with active hemorrhage, were treated with endovascular stentgraft implantation. All patients had undergone major pancreatic or hepatic surgery before (pylorus-preserving pancreaticoduodenectomy, pancreatectomy, hemihepatectomy, extended hemihepatectomy). The pseudoaneurysms were diagnosed 13–202 days after surgery and were associated with postsurgical complications (e.g., leakage of pancreaticojejunal anastomosis).
Results
In 9/10 patients, the pseudoaneurysm was completely excluded via stentgraft implantation. In 1/10 patient, the pseudoaneurysm ruptured during the procedure and was successfully treated by immediate open surgery. In 1/10 patient, a second intervention was performed after 6 days because of rebleeding; this was successfully treated by implantation of a second overlapping stentgraft. Mean follow-up time is 51 days. None of the patients died due to stentgraft- or aneurysm-related complications. Further episodes of hemorrhage were not observed. In one patient, clinically asymptomatic complete occlusion of the stentgraft was discovered at follow-up imaging.
Conclusion
Stentgraft implantation is a safe and effective technique to treat hepatic artery pseudoaneurysms related to major pancreatic or hepatic surgery, especially in the setting of acute hemorrhage.



Similar content being viewed by others
References
Hossain A, Reis ED, Dave SP, Kerstein MD, Hollier LH. Visceral artery aneurysms: experience in a tertiary-care center. Am Surg. 2001;67(5):432–7.
O’Driscoll D, Olliff SP, Olliff JF. Hepatic artery aneurysm. Br J Radiol. 1999;72(862):1018–25.
Berceli SA. Hepatic and splenic artery aneurysms. Semin Vasc Surg. 2005;18(4):196–201.
Iswanto S, Nussbaum ML. Hepatic artery pseudoaneurysm after surgical treatment for pancreatic cancer: minimally invasive angiographic techniques as the preferred treatment. N Am J Med Sci. 2014;6(6):287–90.
Chen J, Weinstein J, Black S, Spain J, Brady PS, Dowell JD. Surgical and endovascular treatment of hepatic arterial complications following liver transplant. Clin Transplant. 2014.
Belli AM, Markose G, Morgan R. The role of interventional radiology in the management of abdominal visceral artery aneurysms. Cardiovasc Intervent Radiol. 2012;35(2):234–43.
Sachdev-Ost U. Visceral artery aneurysms: review of current management options. Mt Sinai J Med. 2010;77(3):296–303.
Spiliopoulos S, Sabharwal T, Karnabatidis D, Brountzos E, Katsanos K, Krokidis M, et al. Endovascular treatment of visceral aneurysms and pseudoaneurysms: long-term outcomes from a multicenter European study. Cardiovasc Intervent Radiol. 2012;35(6):1315–25.
Abbas MA, Fowl RJ, Stone WM, Panneton JM, Oldenburg WA, Bower TC, et al. Hepatic artery aneurysm: factors that predict complications. J Vasc Surg. 2003;38(1):41–5.
Sachdev U, Baril DT, Ellozy SH, Lookstein RA, Silverberg D, Jacobs TS, et al. Management of aneurysms involving branches of the celiac and superior mesenteric arteries: a comparison of surgical and endovascular therapy. J Vasc Surg. 2006;44(4):718–24.
Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, Ouriel K. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2007;45(2):276–83.
Kasirajan K, Greenberg RK, Clair D, Ouriel K. Endovascular management of visceral artery aneurysm. J Endovasc Ther. 2001;8(2):150–5.
Carrafiello G, Rivolta N, Fontana F, Piffaretti G, Mariscalco G, Bracchi E, et al. Combined endovascular repair of a celiac trunk aneurysm using celiac-splenic stent graft and hepatic artery embolization. Cardiovasc Intervent Radiol. 2010;33(2):352–4.
Pasha SF, Gloviczki P, Stanson AW, Kamath PS. Splanchnic artery aneurysms. Mayo Clin Proc. 2007;82:472–9.
Balderi A, Antonietti A, Pedrazzini F, Sortino D, Vinay C, Grosso M. Treatment of visceral aneurysm using multilayer stent: two-year follow-up results in five consecutive patients. Cardiovasc Intervent Radiol. 2013;36:1256–61.
Claessen BE, Henriques JP, Jaffer FA, Mehran R, Piek JJ, Dangas GD. Stent thrombosis: a clinical perspective. JACC Cardiovasc Interv. 2014;7(10):1081–92.
Greenhalgh RM, Powell JT. Endovascular repair of abdominal aortic. N Engl J Med. 2008;358(5):494–501.
de Castro SM, Kuhlmann KF, Busch OR, van Delden OM, Laméris JS, van Gulik TM, Obertop H, Gouma DJ. Delayed massive hemorrhage after pancreatic and biliary surgery: embolization or surgery? Ann Surg. 2005;241(1):85–91.
Suzuki K, Mori Y, Komada T, Matsushima M, Ota T, Naganawa S. Stent-graft treatment for bleeding superior mesenteric artery pseudoaneurysm after pancreaticoduodenectomy. Stent-graft treatment for bleeding superior mesenteric artery pseudoaneurysm after pancreaticoduodenectomy. Cardiovasc Interv Radiol. 2009;32(4):762–6.
Lü PH, Zhang XC, Wang LF, Chen ZL, Shi HB. Stent graft in the treatment of pseudoaneurysms of the hepatic arteries. Vasc Endovascular Surg. 2013;47(7):551–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Pedersoli, F., Isfort, P., Keil, S. et al. Stentgraft Implantation for the Treatment of Postoperative Hepatic Artery Pseudoaneurysm. Cardiovasc Intervent Radiol 39, 575–581 (2016). https://doi.org/10.1007/s00270-015-1274-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-015-1274-1