Abstract
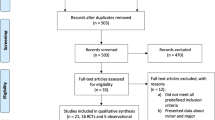
Trocar injuries are a possible cause for severe morbidity and mortality when performing laparoscopic surgery. This systematic review investigates the differences in the incidence of complications depending on the method of entry. A meta-analysis of the medical literature was performed. Search results were limited to clinical trials and the following languages: English, French, German, or Dutch. All results that compared the Veress, Hasson, and direct entry technique or compared sharp, blunt, and radially expanding trocars (RET) were included (n = 19). Studies involving pediatric and pregnant patients were excluded. When comparing the Veress needle to direct trocar insertion (DTI), pooled analysis showed a borderline significant reduction for major complications (p = 0.04) based on five events in 2 RCT’s (n = 978) and a reduction in minor complications (p < 0.001) in favor of DTI. RCT’s comparing the Hasson and Veress techniques showed no significant reduction in major complications (p = 0.17), but the Hasson technique showed significantly less minor complications (p = 0.01) and failed entries (p = 0.002). CO2 leakage was far more common when using the Hasson technique (p < 0.001). Our search method did not reveal any studies comparing the Hasson technique to DTI. When comparing bladed to RET, three studies (n = 408) showed less minor complications when using a RET (p = 0.003) and a qualitative analysis showed a trend toward pain reduction when using RET. This meta-analysis concludes that there are less minor complications and failed attempts when using the Hasson or direct entry technique when compared to the Veress method, but there is limited evidence regarding major complications. RET reduce minor vascular complications when compared to bladed trocars.










Similar content being viewed by others
Abbreviations
- DT:
-
Direct trocar
- DTI:
-
Direct trocar insertion
- MeSH:
-
Medical subject heading
- RCT:
-
Randomized controlled trial
- RE:
-
Radially expanding
- RET:
-
Radially expanding trocar
- RUQ:
-
Right upper quadrant
- VN:
-
Veress needle
References
The Southern Surgeons Club (1991) A prospective analysis of 1518 laparoscopic cholecystectomies. N Engl J Med 324:1073–1078
Mc Anena OJ, Austin O, Hederman WP et al (1991) Laparoscopic versus open appendicectomy. Lancet 338:693
Vilos GA (2000) Litigation of laparoscopic major vessel injuries in Canada. J Am Assoc Gynecol Laparosc 7:503–509
Vilos GA (2002) Laparoscopic bowel injuries: forty litigated gynaecological cases in Canada. J Obstet Gynaecol Can 24:224–230
Jansen FW, Kolkman W, Bakkum EA et al (2004) Complications of laparoscopy: an inquiry about closed- versus open-entry technique. Am J Obstet Gynecol 190:634–638
Magrina JF (2002) Complications of laparoscopic surgery. Clin Obstet Gynecol 45:469–480
Kroft J, Aneja A, Tyrwhitt J et al (2009) Laparoscopic peritoneal entry preferences among Canadian gynaecologists. J Obstet Gynaecol Can 31:641–648
Lalchandani S, Phillips K (2005) Laparoscopic entry technique—a survey of practices of consultant gynaecologists. Gynecol Surg 2:245–249
Ternamian A (2007) B manual of new hysterectomy techniques, Chapter 19—port creation during laparoscopic hysterectomy. Press Medical Publishers Ltd, Jaypee Bros 2007
Antoniou SA, Antoniou GA, Koch OO et al (2013) Blunt versus bladed trocars in laparoscopic surgery: a systematic review and meta-analysis of randomized trials. Surg Endosc 27:2312–2320
Philips PA, Amaral JF (2001) Abdominal access complications in laparoscopic surgery. J Am Coll Surg 192:525–536
Hasson HM, Rotman C, Rana N et al (2000) Open laparoscopy: 29-year experience. Obstet Gynecol 96:763–766
Agresta F, De Simone P, Ciardo LF et al (2004) Direct trocar insertion versus Veress needle in nonobese patients undergoing laparoscopic procedures: a randomized prospective single-center study. Surg Endosc 18:1778–1781
Ternamian AM, Vilos GA, Vilos AG et al (2010) Laparoscopic peritoneal entry with the reusable threaded visual cannula. J Minim Invasive Gynecol 17:461–467
Vilos GA, Vilos AG, Abu-Rafea B et al (2009) Three simple steps during closed laparoscopic entry may minimize major injuries. Surg Endosc 23:758–764
Nezhat FR, Silfen SL, Evans D et al (1991) Comparison of direct insertion of disposable and standard reusable laparoscopic trocars and previous pneumoperitoneum with Veress needle. Obstet Gynecol 78:148–150
Angioli R, Terranova C, De Cicco Nardone C et al (2013) A comparison of three different entry techniques in gynecological laparoscopic surgery: a randomized prospective trial. Eur J Obstet Gynecol Reprod Biol 171:339–342
Byron JW, Markenson G, Miyazawa K (1993) A randomized comparison of Verres needle and direct trocar insertion for laparoscopy. Surg Gynecol Obstet 177:259–262
Zakherah MS (2010) Direct trocar versus veress needle entry for laparoscopy: a randomized clinical trial. Gynecol Obstet Invest 69:260–263
Prieto-Diaz-Chavez E, Medina-Chavez JL, Gonzalez-Ojeda A et al (2006) Direct trocar insertion without pneumoperitoneum and the Veress needle in laparoscopic cholecystectomy: a comparative study. Acta Chir Belg 106:541–544
Gunenc MZ, Yesildaglar N, Bingol B et al (2005) The safety and efficacy of direct trocar insertion with elevation of the rectus sheath instead of the skin for pneumoperitoneum. Surg Laparosc Endosc Percutan Tech 15:80–81
Borgatta L, Gruss L, Barad D et al (1990) Direct trocar insertion versus Verres needle use for laparoscopic sterilization. J Reprod Med 35:891–894
Cogliandolo A, Manganaro T, Saitta FP et al (1998) Blind versus open approach to laparoscopic cholecystectomy: a randomized study. Surg laparosc Endosc 8:353–355
Akbar M, Khan IA, Naveed D et al (2008) Comparison of closed and open methods of pneumoperitonium in laparoscopic cholecystectomy. JAMC 20:85–89
Bemelman WA, Dunker MS, Busch OR et al (2000) Efficacy of establishment of pneumoperitoneum with the Veress needle, Hasson trocar, and modified blunt trocar (TrocDoc): a randomized study. J Laparoendosc Adv Surg Tech A 10:325–330
Channa GA, Siddiqui AJ, Zafar SN (2009) Open versus closed method of establishing pneumoperitoneum for laparoscopic cholecystectomy. J Coll Phys Surg Pak 19:557–560
Peitgen K, Nimtz K, Hellinger A et al (1997) Open approach or Veress needle in laparoscopic interventions? Results of a prospective randomized controlled study—Der Chirurg. Zeitschrift fur alle Gebiete der operativen Medizen 68:910–913
Bhoyrul S, Payne J, Steffes B et al (2000) A randomized prospective study of radially expanding trocars in laparoscopic surgery. J Gastrointest Surg 4:392–397
Bisgaard T, Jakobsen HL, Jacobsen B et al (2007) Randomized clinical trial comparing radially expanding trocars with conventional cutting trocars for the effects on pain after laparoscopic cholecystectomy. Surg Endosc 21:2012–2016
Feste JR, Bojahr B, Turner DJ (2000) Randomized trial comparing a radially expandable needle system with cutting trocars. J Soc Laparoendosc 4:11–15
Yim SF, Yuen PM (2001) Randomized double-masked comparison of radially expanding access device and conventional cutting tip trocar in laparoscopy. Obstet Gynecol 97:435–438
Stepanian AA, Winer WK, Isler CM et al (2007) Comparative analysis of 5-mm trocars: dilating tip versus non-shielded bladed. J Minim Invasive Gynecol 14:176–183
Hamade AM, Issa ME, Haylett KR et al (2007) Fixity of ports to the abdominal wall during laparoscopic surgery: a randomized comparison of cutting versus blunt trocars. Surg Endosc 21:965–969
Venkatesh R, Sundaram CP, Figenshau RS et al (2007) Prospective randomized comparison of cutting and dilating disposable trocars for access during laparoscopic renal surgery. J Soc Laparoendosc Surg 11:198–203
Jacobson MT, Osias J, Bizhang R et al (2002) The direct trocar technique: an alternative approach to abdominal entry for laparoscopy. J Soc Laparoendosc Surg 6:169–174
Ternamian AM (1997) Laparoscopy without trocars. Surg Endosc 11:815–818
Hickey L, Rendon RA (2006) Safe and novel technique for peritoneal access in urologic laparoscopy without prior insufflation. J Endourol 20:622–626
Melzer A, Riek S, Roth K et al (1995) Endoscopically controlled trocar and cannula insertion. Endosc Surg Allied Technol 3:63–68
Ahmad G, O’Flynn H, Duffy JM, Phillips K, Watson A (2012) Laparoscopic entry techniques (Review). Cochrane Database Syst Rev 2:6583
Shayani-Nasab H, Amir-Zargar MA, Mousavi-Bahar SH et al (2013) Complications of entry using Direct Trocar and/or Veress Needle compared with modified open approach entry in laparoscopy: 6-year experience. Urol J 10:861–865
Altun H, Banli O, Karakoyun R et al (2010) Direct trocar insertion technique for initial access in morbid obesity surgery: technique and results. Surg Laparosc Endosc Percutan Tech 20:228–230
Bhoyrul SMT, Way LW (1996) Radially expanding dilatation. A superior method of laparoscopic trocar access. Surg Endosc 10:775–778
Lam TY, Lee SW, So HS et al (2000) Radially expanding trocar: a less painful alternative for laparoscopic surgery. J Laparoendosc Adv Surg Tech A 10:269–273
Mordecai SC, Warren OW, Warren SJ (2012) Radially expanding laparoscopic trocar ports significantly reduce postoperative pain in all age groups. Surg Endosc 26:843–846
Schafer M, Lauper M, Krahenbuhl L (2001) Trocar and Veress needle injuries during laparoscopy. Surg Endosc 15:275–280
Fuller J, Ashar BS, Carey-Corrado J (2005) Trocar-associated injuries and fatalities: an analysis of 1399 reports to the FDA. J Minim Invasive Gynecol 12:302–307
Chapron C, Querleu D, Bruhat MA et al (1998) Surgical complications of diagnostic and operative gynaecological laparoscopy: a series of 29,966 cases. Hum Reprod 13(4):867–872
Romain N, Michaud K, Brandt-Casadevall C et al (2003) Fatal aortic injury during laparoscopy: report of two cases. Am J Forensic Med Pathol 24:80–82
Leonard F, Lecuru F, Rizk E et al (2000) Perioperative morbidity of gynecological laparoscopy. A prospective monocenter observational study Acta obstetricia et gynecologica Scandinavica 79:129–134
Hurd WW, Bude RO, DeLancey JO et al (1994) The location of abdominal wall blood vessels in relationship to abdominal landmarks apparent at laparoscopy. Am J Obstet Gynecol 171:642–646
Nezhat F, Brill AI, Nezhat CH et al (1998) Laparoscopic appraisal of the anatomic relationship of the umbilicus to the aortic bifurcation. J Am Assoc Gynecol Laparosc 5:135–140
Balzer KM, Witte H, Recknagel S et al (1999) Anatomic guidelines for the prevention of abdominal wall hematoma induced by trocar placement. Surg Radiol Anat 21:87–89
Saber AA, Meslemani AM, Davis R et al (2004) Safety zones for anterior abdominal wall entry during laparoscopy: a CT scan mapping of epigastric vessels. Ann Surg 239:182–185
van Ramshorst GH, Kleinrensink GJ, Hermans JJ et al (2009) Abdominal wall paresis as a complication of laparoscopic surgery Hernia. J Hernia Abdominal Wall Surg 13:539–543
Whiteside JL, Barber MD, Walters MD et al (2003) Anatomy of ilioinguinal and iliohypogastric nerves in relation to trocar placement and low transverse incisions. Am J Obstet Gynecol 189:1574–1578 (discussion 1578)
Levy BF, De Guara J, Willson PD et al (2012) Bladder injuries in emergency/expedited laparoscopic surgery in the absence of previous surgery: a case series. Ann R Coll Surg Engl 94:e118–e120
Philosophe R (2003) Avoiding complications of laparoscopic surgery. Fertil Steril 80(4):30–39 (quiz 54-36)
Brill AI, Nezhat F, Nezhat CH et al (1995) The incidence of adhesions after prior laparotomy: a laparoscopic appraisal. Obstet Gynecol 85:269–272
Levrant SG, Bieber EJ, Barnes RB (1997) Anterior abdominal wall adhesions after laparotomy or laparoscopy. J Am Assoc Gynecol Laparosc 4:353–356
Dubuisson J, Botchorishvili R, Perrette S et al (2010) Incidence of intraabdominal adhesions in a continuous series of 1000 laparoscopic procedures. Am J Obstet Gynecol 203(111):e111–e113
Kolecki RV, Golub RM, Sigel B et al (1994) Accuracy of viscera slide detection of abdominal wall adhesions by ultrasound. Surg Endosc 8:871–874
Kothari SN, Fundell LJ, Lambert PJ et al (2006) Use of transabdominal ultrasound to identify intraabdominal adhesions prior to laparoscopy: a prospective blinded study. Am J Surg 192:843–847
Tu FF, Lamvu GM, Hartmann KE et al (2005) Preoperative ultrasound to predict infraumbilical adhesions: a study of diagnostic accuracy. Am J Obstet Gynecol 192:74–79
Levy B (1997) Perforation of large vascular structures. In: Diamond MP, Corfman RS, DeCherney AH (eds) Complications of Laparoscopy and Hysteroscopy, 2nd edn. Blackwell Science, Oxford, pp 26–29
Pring CM (2007) Aortic injury using the Hasson trocar: a case report and review of the literature. Ann R Coll Surg Engl 89:W3–W5
Polyzos D, Papadopoulos N, Chapman L et al (2007) Where is the aorta? Is it worth palpating the aorta prior to laparoscopy? Acta Obstet Gynecol Scand 86:235–239
Sasmal PK, Tantia O, Jain M et al (2009) Primary access-related complications in laparoscopic cholecystectomy via the closed technique: experience of a single surgical team over more than 15 years. Surg Endosc 23:2407–2415
Schwartz ML, Drew RL, Andersen JN (2003) Induction of pneumoperitoneum in morbidly obese patients. Obes Surg 13:601–604 (discussion 604)
Hurd WW, Bude RO, DeLancey JO et al (1992) The relationship of the umbilicus to the aortic bifurcation: implications for laparoscopic technique. Obstet Gynecol 80:48–51
Hurd WH, Bude RO, DeLancey JO et al (1991) Abdominal wall characterization with magnetic resonance imaging and computed tomography. The effect of obesity on the laparoscopic approach. J Reprod Med 36:473–476
Teoh B, Sen R, Abbott J (2005) An evaluation of four tests used to ascertain Veres needle placement at closed laparoscopy. J Minim Invasive Gynecol 12:153–158
Azevedo OC, Azevedo JL, Sorbello AA et al (2006) Evaluation of tests performed to confirm the position of the Veress needle for creation of pneumoperitoneum in selected patients: a prospective clinical trial. Acta Cir Bras 21:385–391
Vilos GA, Vilos AG (2003) Safe laparoscopic entry guided by Veress needle CO2 insufflation pressure. J Am Assoc Gynecol Laparosc 10:415–420
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Appendix
Appendix
The MEDLINE database was searched for clinical trials using PubMed and the following terms:
Laparoscopy [Mesh] AND “clinical trial” [filter] AND
-
1.
Trocar access (58)
-
2.
Veress (39)
-
3.
Hasson (11)
-
4.
Direct trocar (40)
-
5.
Trocar insertion (58)
-
6.
Entry method (56)
-
7.
Primary port (51)
-
8.
Blunt trocar (6)
-
9.
Bladed trocar (2)
-
10.
Radially expanding (4)
-
11.
Radially expanding trocar (5)
Rights and permissions
About this article
Cite this article
Cornette, B., Berrevoet, F. Trocar Injuries in Laparoscopy: Techniques, Tools, and Means for Prevention. A Systematic Review of the Literature. World J Surg 40, 2331–2341 (2016). https://doi.org/10.1007/s00268-016-3527-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-016-3527-9