Abstract
Background
Our institute caters to a large number of patients with large, longstanding multinodular goiters; tracheal deviation and resulting airway problems like tracheomalacia are relatively common. However, the literature is sparse on the criteria of early diagnosis and optimum management of tracheomalacia, which our study highlights.
Methods
This retrospective study analyzed 900 thyroidectomies carried out during 1990–2005 for which data from 28 patients treated for tracheomalacia after thyroidectomy were available for analysis. Criteria for making a diagnosis of tracheomalacia after thyroidectomy included one or more of the following: normal vocal cord mobility, absence of glottic or subglottic edema or hematoma, soft and floppy trachea on palpation, obstruction to spontaneous respiration on gradual withdrawal of the endotracheal tube.
Results
Mean duration of thyroid enlargement was 13.75 years. Only 7 patients had a history of stridor. Tracheostomy was performed in 26 patients, and 2 patients were put on prolonged intubation. Tracheostomy was performed in 18 patients on the operating table, and 8 in the recovery room. The mean weight of the gland was 442 g and histopathology revealed that 11 cases were benign goiter. The tracheostomy tube was removed after an average of 8.5 days. There were no cases of tracheal stenosis on long-term follow-up.
Conclusions
Patients with longstanding goiter, even when benign, are more prone to develop tracheomalacia. On the basis of our experience we strongly advocate tracheostomy intraoperatively if the trachea is soft and floppy and/or collapse of the trachea is observed following gradual withdrawal of the endotracheal tube.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Tracheomalacia has been defined as an extreme degree of compression of the airway, where the cross-sectional area of the trachea is reduced to less than half. It results from longstanding compression by a large goiter wherein rings of the trachea may be completely destroyed or considerably weakened resulting in poor support to the trachea. Such a trachea is prone to collapse after thyroidectomy, resulting in postoperative respiratory obstruction which may be catastrophic. However, the condition is supposedly rare, poorly understood, and of course apparently reversible. There has been a considerable debate about possible risk factors for the development of tracheomalacia and whether they can be sought preoperatively. The purpose of this retrospective study was to document the existence of tracheomalacia as a definite entity and to suggest guidelines for successful management of this condition.
PATIENTS AND METHODS
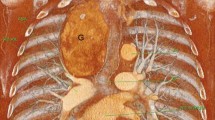
This retrospective study included patients with thyroid diseases who underwent operation in the Department of Endocrine Surgery, SPGIMS, Lucknow, India, over the 15-year period from 1990 to 2005. Of the 900 patients operated on for thyroid diseases, 28 (1.9%) were diagnosed with tracheomalacia. All patients underwent plain x-ray neck (anterior-posterior and lateral view) for assessment of tracheal air shadow, to look for compression, deviation, or narrowing of tracheal lumen.
General anesthesia was administered using thiopental, 50%–70% N2O in O2, opioids (morphine or fentanyl), and inhalation agents (halothane or isoflurane). In all patients undergoing thyroidectomy, tracheal intubation was facilitated without difficulty using vecuronium (0.1 mg / kg) with a cuffed endotracheal tube (ETT) one size smaller than the expected endotracheal size. An attempt was made to place the tip of the ETT well below the vocal cords but above the carina in order to prevent sub-glottic trauma by the ETT cuff. The decision to perform tracheostomy is not based on the number of tracheal rings involved in collapse. Rather, we have selected one or more of the following criteria to make a diagnosis of tracheomalacia intraoperatively: (1) Soft and floppy trachea on palpation at the end of thyroidectomy. This condition will prompt the surgeon to ask the anaesthetist to gradually retract the tube for a short distance to permit palpation of the trachea without the tube in place. This maneuver may help the surgeon see an obvious collapse of the tracheal wall or any obstruction to spontaneous respiration during gradual withdrawal of the ETT after thyroidectomy. (2) Another sign is difficulty in negotiating the suction catheter beyond the ETT after gradual withdrawal. (3) After wound closure, tracheomalacia should be suspected if there is no peritubal leakage after deflation of the ETT cuff, if there is a volume pressure loop on the ventilator, or if respiratory stridor develops in conjunction with a reduction in hemoglobin oxygen saturation on pulse oximetry, even with administration of oxygen. Anesthesia was reversed with neostigmine (2.5 mg) and atropine (0.6 mg) or glycopyrrolate (0.6 mg) as required. We did not perform bronchoscopy on follow-up.
RESULTS
The male:female ratio in our series was 0.75:1; the mean age was 51.4 ± 13.8 years. All patients had grade II goiter (WHO grading). The mean duration of goiter was 13.7 years (Bar chart 1) and tracheal compression, deviation, and kinking was present in all patients preoperatively, as shown by either plain x-ray or CT imaging. Only seven patients had a history of stridor, and four patients noted a history of dysphagia for solids. Retrosternal extension of varying degrees was found in 11 patients. Indirect laryngoscopy was performed preoperatively in all patients, with normal results in 26 patients and failure to visualize the vocal cords in the two remaining patients.
The various operative procedures, timing of the diagnosis of tracheomalacia and criteria for the diagnosis of tracheomalacia are shown in Table 1. In 20 patients, tracheomalacia was diagnosed before extubation, whereas in the remaining 8 patients it was diagnosed after tracheal extubation. Tracheostomy was performed in 26 patients while two patients were put on prolonged intubation. The mean weight of the gland was 442 ± 246 g and on histopathology, 11 cases were of benign goiter. Postoperative indirect laryngoscopy did not reveal bilateral vocal cord palsy in any patient. There was no case of postoperative hematoma.
Of 26 tracheostomized patients, decannulation of the trachea was successfully accomplished in 23 patients at a mean of 8.5 ± 5.6 days postprocedure. Two patients were discharged with a tracheostomy tube in situ, and one patient died on postoperative day (POD) 4 in the surgical intensive care unit. This 38-year-old woman had grade III goiter with bilateral neck nodes of 5 years duration. She had presented with severe compressive symptoms, breathlessness, and stridor. Investigation revealed poorly differentiated thyroid carcinoma with bilateral pulmonary metastases. She underwent total thyroidectomy, and, in view of her severe symptoms, right radical neck dissection and left selective neck dissection of levels II, III, IV, and V. There was no invasion to the tracheal adventitia. The weight of the thyroidectomy specimen was 320 g. Tracheomalacia was recognized before tracheal extubation and a tracheostomy was done. Postoperatively in surgical intensive care unit, the patient could not maintain adequate oxygen saturation, possibly because of diffuse pulmonary metastases. She could not be given ventilatory support in view of her poor financial condition, and she died on POD 4. Histopathology results later reported a poorly differentiated thyroid carcinoma with bilateral neck lymph node metastases.
We did not observe an increased rate of peritracheal infection in our tracheotomized patients. However, antibiotic coverage was started and continued for two days after decannulation. On long-term follow-up no case of tracheal stenosis was seen.
DISCUSSION
Tracheomalacia may result from longstanding compression by a large goiter. The cartilaginous rings of the trachea may be completely destroyed or considerably weakened by longstanding compression, resulting in poor support to the trachea. Such a trachea is prone to collapse after thyroidectomy, and it may result in postoperative respiratory obstruction which may be catastrophic at times. The incidence of tracheomalacia has previously been reported between 0.001% and 1.5%.1–3 The highest incidence (1.5%) previously reported was in substernal goiter4; in our series the incidence was 1.9%. However, in the series of 200 large cervical and substernal goiter treated at Massachusetts Eye and Ear infirmary and Massachusetts General Hospital, not a single case of tracheomalacia was identified, even in the setting of chronic significant tracheal deviation, compression, and remodeling with massive and recurrent goiters.5 Thus, the condition is poorly understood, supposedly rare, and apparently reversible.
Tracheomalacia has been defined as an extreme degree of compression of the airway, where the cross-sectional area of the trachea is reduced to less than half.6,7 The predominant clinical feature is a progressive asphyxia not responding to increasing fractionated inspired oxygen concentration (FiO2). Stridor becomes evident only when the tracheal diameter is reduced to less than 3.5 mm, and it signals critical functional obstruction.8 There has been considerable debate about possible risk factors for the development of tracheomalacia and whether they can be sought preoperatively. Clinical findings thought to be associated with tracheomalacia are a preoperative history of stridor, radiological evidence of tracheal deviation or compression, retrosternal goiter, and difficulty in intubation by the anesthetist. Preoperative history of stridor may not be a predictor of tracheomalacia. In our series, only seven patients had history of stridor. Stridor at times may be associated with mechanical changes in the configuration of the tracheal lumen; however, collapse of the walls is unlikely to occur unless the trachea is pathologically soft.
Radiological evidence of tracheal narrowing or compression was thought to predict a difficult intubation and possibly respiratory obstruction due to tracheomalacia after thyroidectomy. However, ease of Intubation is unrelated to the extent of abnormalities seen on imaging studies of the neck.9 In our series use of fibre optic assisted intubation was not required in any case.
This is consistent with the experience of Shaha and colleagues,10 who treated 120 patients with airway compression secondary to goiter, including 30 patients who presented with acute airway distress. In substernal goiter, although airway compression is by for the most common finding, tracheomalacia is uncommon. In our series 11 patients had varying degrees of retrosternal extension. Preoperative evidence of compression cannot predict tracheomalacia, even though most of our patients who developed tracheomalacia had radiological evidence of varying degrees of tracheal narrowing, compression, and deviation. Other patients with multinodular goiter and preoperative evidence of compression did not develop tracheomalacia.
The next important point is recognition of tracheomalacia on the operating table before extubation. There is no single foolproof criterion for confirming a diagnosis of tracheomalacia. However, for the intraoperative diagnosis of tracheomalacia, we have taken one or more of the following criteria: (1) Soft and floppy trachea on palpation by the surgeon at the end of thyroidectomy. However, because of splinting effect of the endotracheal tube in situ, it may be difficult to appreciate a soft trachea. We therefore ask the anesthethesiologist to gradually withdraw the tube for a short distance and then feel the trachea without the tube in site. This maneuver may also help the surgeon recognize an obvious collapse of the tracheal wall. (2) Obstruction to spontaneous respiration during gradual withdrawal of the ETT after thyroidectomy. (3) Difficulty in negotiating the suction catheter beyond the ETT after gradual withdrawal. (4) After closure of the wound, tracheomalacia can be suspected (a) if there is absence of peritubal leak on deflation of ETT cuff, (b) volume pressure loop on ventilator or (c) development of respiratory stridor along with a falling hemoglobin oxygen saturation (SpO2) on pulse oximetry despite the administration of increasing FiO2. It is also important to rule out B/L vocal cord palsy or glottic/subglottic edema which are more common causes of stridor.
Suggested methods of management of tracheomalacia are tracheostomy, prolonged intubation, tracheopexy, external splinting with Marlex mesh, and external miniplate fixation of tracheal cartilages and placement of a buttress or graft. It has been suggested that leaving the endotracheal tube in place for 24–48 h postoperatively to serve as a splint before extubation in a controlled setting can be successful in many cases.4 However, it can also be argued that if tracheomalacia results from chronic goiter compression, it is unclear how short-term intubation would make structurally intact a trachea that has been rendered significantly floppy by chronic goiter compression. We prefer to go for an early tracheostomy if there is definite softening of the trachea. We think that it is better to do a tracheostomy at the time of surgery, as it is easier to visualize the part of trachea most suitable for tracheostomy. Further, the trachea toilet as well as ventilatory care, if needed, is easier in patients with tracheostomy than in those with the ETT kept in place. Unlike prolonged intubation, tracheostomy results in fibrosis around a soft trachea resulting in early recovery from tracheomalacia. We also did not encounter any cases of trachea stenosis following tracheostomy for tracheomalacia, as found by Green et al.11 All of the tracheostomized patients had their tracheostomy tube removed after an average period of 8.5 days, and none of them showed any long-term complications of the procedure. Because there was no case of bilateral vocal cord palsy, the diagnosis of tracheomalacia was certain in all cases.
It is also important to realize that the collapse of a floppy trachea may not always be circumferential. Collapse of a portion of the lateral tracheal wall may occur, leading to respiratory obstruction in the postoperative period.
CONCLUSIONS
We suggest that tracheomalacia is a definite entity that is likely to be seen in longstanding and large goiters, especially in endemic goiter regions. Our study identifies possible criteria for making an early diagnosis of tracheomalacia and describes various management strategies, among which tracheostomy seems to be the best option.
References
Sitges-Serra A, Sancho J. Surgical management of recurrent and intrathoracic goiter. In Clark O, Duh Q-Y, Kebebew E, editors, Textbook of Endocrine Surgery, Philadelphia, W.B. Saunders Company, 1997
Green WE, Shepperd HW, Stevenson HM, et al. Tracheal collapse after thyroidectomy. Br J Surg 1979;66:554
Peterson JL, Rovenstine EA. Tracheal collapse complicating thyroidectomy: a case report. Curr Res Anesth Analg 1936;15:300
Singh B, Lucente FE, Shaha AR. Substernal goiter: a clinical review. Am J Otolaryngol 1994;15:409
Shin J, Randolph GW, Grillo H. Surgery for cervical and substernal goiter in 200 patients at Massachusetts Eye and Ear Infirmary and Massachusetts General Hospital. Laryngoscope (submitted)
Jokinen K, Palva T, Sutinen S, Nuutinen J. Acquired tracheo-broncho-malacia. Ann Clin Res 1977;9:52–57
Johnson TH, Mikita JJ, Wilson RJ, Feist JH. Acquired tracheomalacia. Diagn Radiol 1973;109:577–580
Conacher ID. Anaesthesia for Thoracic and Pulmonary Surgery. In Prys-Roberts C, Brown Br Jr, Eds., Butterworth Heinemann, 1936;15:300
McHenry CR, Piotrowsi. Thyroidectomy in patients with marked thyroid enlargement: airway management, morbidity, and outcome. Am Surg 1994;60:586–591
Shaha A, Alfonso A, Jaffe BM. Acute airway distress due to thyroid pathology. Surgery 1987;102:1068–1074
Green WER, Shepperd HWH, Stevenson HM, et al. Tracheal collapse after thyroidectomy. Br J Surg 1979;66:554–557
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agarwal, A., Mishra, A.K., Gupta, S.K. et al. High Incidence of Tracheomalacia in Longstanding Goiters: Experience from an Endemic Goiter Region. World J. Surg. 31, 832–837 (2007). https://doi.org/10.1007/s00268-006-0565-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-006-0565-8