Abstract
Objective
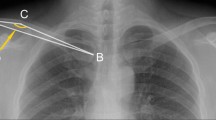
This study aims to introduce a self-designed clavicle reductor and to test the effectivity of a alternative minimally invasive plate osteosynthesis technique (MIPO) for displaced midshaft clavicular fractures (DMCFs) with the application of our self-designed clavicle reductor.
Method
From October 2012 to February 2013, 27 male patients who suffered with unilateral displaced midshaft clavicular fracture (DMCFs) were included into our study. Patients were treated by minimally invasive plate osteosynthesis (MIPO) technique with the application of our self-designed clavicle reductor and followed up regularly. Constant-Murley score was employed to test the functional outcomes at one year’s follow up.
Result
The average follow-up time for the 27 patients was 15.8 months (range, 13–18 months). The average age of all patients was 32.6 (range, 21 to 48). According to OTC system, 12 cases were simple fractures (15-B1), ten cases were wedge fractures (15-B2) and five cases were comminuted fractures (15-B3). With the application of the clavicle reductor, minimally invasive plate osteosynthesis technique can be performed without any barrier in all of the 27 cases. Operative duration was 48.1 minutes (range, 35–65 minutes) and average fluoroscopy time was 12.8 seconds (range, from 7 to 22 seconds). All of the 27 cases healed from four to six months post-operatively. The average Constant-Murley-score of the 27 patients was 92.7 ± 5.88 (range, 80 to 100). No complications were noted.
Conclusion
The self-designed clavicle reductor can effectively pave the way for the application of MIPO technique in the treatment of DMCFs. MIPO technique with locking reconstruction plate is a feasible and worthwhile alternative for displaced midshaft clavicular fractures (DMCFs).



Similar content being viewed by others
References
van der Meijden OA, Gaskill TR, Millett PJ (2012) Treatment of clavicle fractures: current concepts review. J Shoulder Elb Surg 21(3):423–429
Neer CS 2nd (1960) Nonunion of the clavicle. J Am Med Assoc 172:1006–1011
Jorgensen A, Troelsen A, Ban I (2014) Predictors associated with nonunion and symptomatic malunion following non-operative treatment of displaced midshaft clavicle fractures−a systematic review of the literature. Int Orthop 38:2543–2549
Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD (2005) Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the evidence-based orthopaedic trauma working group. J OrthopTrauma 19(7):504–507
Hill JM, McGuire MH, Crosby LA (1997) Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg (Br) 79(4):537–539
Zhu Y, Tian Y, Dong T et al (2015) Management of the mid-shaft clavicle fractures using plate fixation versus intramedullary fixation: an updated meta-analysis. Int Orthop 39:319–328
Millett PJ, Hurst JM, Horan MP, Hawkins RJ (2011) Complications of clavicle fractures treated with intramedullary fixation. J Shoulder Elb Surg 20(1):86–91
Strauss EJ, Egol KA, France MA, Koval KJ, Zuckerman JD (2007) Complications of intramedullary Hagie pin fixation for acute midshaft clavicle fractures. J Shoulder Elb Surg 16(3):280–284
Krettek C, Schandelmaier P, Miclau T, Tscherne H (1997) Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury 28(Suppl 1):A20–A30
Postacchini F, Gumina S, De Santis P, Albo F (2002) Epidemiology of clavicle fractures. J Shoulder Elb Surg 11(5):452–456
Nordqvist A, Petersson C (1994) The incidence of fractures of the clavicle. Clin Orthop Relat Res 300:127–132
Robinson CM (1998) Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg (Br) 80(3):476–484
Collinge C, Devinney S, Herscovici D, DiPasquale T, Sanders R (2006) Anterior-inferior plate fixation of middle-third fractures and nonunions of the clavicle. J Orthop Trauma 20(10):680–686
Chen YF, Wei HF, Zhang C, Zeng BF, Zhang CQ, Xue JF, Xie XT, Lu Y (2012) Retrospective comparison of titanium elastic nail (TEN) and reconstruction plate repair of displaced midshaftclavicular fractures. J Shoulder Elb Surg 21(4):495–501
Apivatthakakul T, Arpornchayanon O, Bavornratanavech S (2005) Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury 36(4):530–538
Sohn HS, Shin SJ, Kim BY (2012) Minimally invasive plate osteosynthesis using anterior-inferior plating of clavicularmidshaft fractures. Arch Orthop Trauma Surg 132(2):239–244
Jiang H, Qu W (2012) Operative treatment of clavicle midshaft fractures using a locking compression plate: comparison between mini-invasive plate osteosynthesis (MIPPO) technique and conventional open reduction. Orthop Traumatol Surg Res 98(6):666–671
Babst R, Hehli M, Regazzoni P (2001) LISS tractor. Combination of the “less invasive stabilization system” (LISS) with the AO distractor for distal femur and proximal tibial fractures. Unfallchirurg 104(6):530–535
Perren SM (2002) The technology of minimally invasive percutaneous osteosynthesis (MIPO). Injury 33(Suppl 1):VI–VII
Krettek C, Muller M, Miclau T (2001) Evolution of minimally invasive plate osteosynthesis (MIPO) in the femur. Injury 32(Suppl 3):SC14–SC23
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
There is no funding source.
Ethical approval
The studyhas approvedby the Ethical Board of the Third Hospital of Hebei Medical University (Shijiazhuang, China) after a thorough examination and verification.
Rights and permissions
About this article
Cite this article
Zhang, T., Chen, W., Sun, J. et al. Minimally invasive plate osteosynthesis technique for displaced midshaft clavicular fracture using the clavicle reductor. International Orthopaedics (SICOT) 41, 1679–1683 (2017). https://doi.org/10.1007/s00264-016-3392-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3392-z