Abstract
Purpose
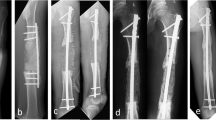
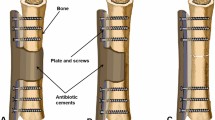
Recently we modified the Masquelet technique by using an antibiotic cement-coated locking plate as a temporary internal fixator when treating septic bone defects. This modification is in order to prevent the complications related to external fixator use and provides the involved limb with a greater stability to undergo earlier and more vigorous physical therapy for recovery of joint function. The purpose of this study was to assess the outcomes of large femoral osteomyelitis defects managed by Masquelet technique combined with the antibiotic cement-coated locking plate used as a temporary internal fixator.
Methods
Between November 2013 to November 2014, 13 cases of large femoral osteomyelitis defects were treated by Masquelet technique and the antibiotic cement-coated locking plate was used as a temporary internal fixator in the first stage surgery. All the patients’ clinical and imaging results were retrospectively analyzed.
Results
After debridement, there was a femoral bone defect with a mean of 9.8 cm (range, 5–16 cm). The mean follow-up was 17.8 months (range 12 to 24 months). One patient developed infection in nine months after second stage surgery. Radiographic bony union was achieved within a mean 20.3 weeks (range, 18–30 weeks) in all patients. The mean time period to full weight bearing after the second step procedure was 5.8 months (range, 5–8.5 months). The mean knee range of motion for the patients at the last follow up was 122° (range 100–135°).
Conclusion
Based on our experience, we believe that antibiotic cement-coated locking plate is a viable fixation method in the first stage of Masquelet technique for the management of large femoral osteomyelitis defects. It may offer a better chance of infection eradication as well as improved recovery of joint function without increasing the infection recurrence rate and without compromising bone graft union.


Similar content being viewed by others
References
Cierny G 3rd (2011) Surgical treatment of osteomyelitis. Plast Reconstr Surg 127(Suppl 1):190S–204S. doi:10.1097/PRS.0b013e3182025070
Kinik H, Karaduman M (2008) Cierny-Mader Type III chronic osteomyelitis: the results of patients treated with debridement, irrigation, vancomycin beads and systemic antibiotics. Int Orthop 32(4):551–558. doi:10.1007/s00264-007-0342-9
Kocaoglu M, Eralp L, Rashid HU, Sen C, Bilsel K (2006) Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J Bone Joint Surg Am 88(10):2137–2145. doi:10.2106/JBJS.E.01152
Masquelet AC, Begue T (2010) The concept of induced membrane for reconstruction of long bone defects. Orthop Clin North Am 41(1):27–37. doi:10.1016/j.ocl.2009.07.011, table of contents
Mauffrey C, Hake ME, Chadayammuri V, Masquelet AC (2015) Reconstruction of long bone infections using the induced membrane technique: tips and tricks. J Orthop Trauma. doi:10.1097/BOT.0000000000000500
Taylor BC, Hancock J, Zitzke R, Castaneda J (2015) Treatment of bone loss with the induced membrane technique: techniques and outcomes. J Orthop Trauma 29(12):554–557. doi:10.1097/BOT.0000000000000338
Masquelet AC, Fitoussi F, Begue T, Muller GP (2000) Reconstruction of the long bones by the induced membrane and spongy autograft. Ann Chir Plast Esthet 45(3):346–353
Bhandari M, Zlowodzki M, Tornetta P 3rd, Schmidt A, Templeman DC (2005) Intramedullary nailing following external fixation in femoral and tibial shaft fractures. J Orthop Trauma 19(2):140–144
Jennison T, McNally M, Pandit H (2014) Prevention of infection in external fixator pin sites. Acta Biomater 10(2):595–603. doi:10.1016/j.actbio.2013.09.019
Bose D, Kugan R, Stubbs D, McNally M (2015) Management of infected nonunion of the long bones by a multidisciplinary team. Bone Joint J 97-B(6):814–817. doi:10.1302/0301-620X.97B6.33276
Campoccia D, Montanaro L, Arciola CR (2006) The significance of infection related to orthopedic devices and issues of antibiotic resistance. Biomaterials 27(11):2331–2339. doi:10.1016/j.biomaterials.2005.11.044
Olesen UK, Eckardt H, Bosemark P, Paulsen AW, Dahl B, Hede A (2015) The Masquelet technique of induced membrane for healing of bone defects. a review of 8 cases. Injury 46(Suppl 8):S44–S47. doi:10.1016/S0020-1383(15)30054-1
Scholz AO, Gehrmann S, Glombitza M, Kaufmann RA, Bostelmann R, Flohe S, Windolf J (2015) Reconstruction of septic diaphyseal bone defects with the induced membrane technique. Injury 46(Suppl 4):S121–S124. doi:10.1016/S0020-1383(15)30030-9
Schmidmaier G, Lucke M, Wildemann B, Haas NP, Raschke M (2006) Prophylaxis and treatment of implant-related infections by antibiotic-coated implants: a review. Injury 37(Suppl 2):S105–S112. doi:10.1016/j.injury.2006.04.016
Thonse R, Conway J (2007) Antibiotic cement-coated interlocking nail for the treatment of infected nonunions and segmental bone defects. J Orthop Trauma 21(4):258–268. doi:10.1097/BOT.0b013e31803ea9e6
Thonse R, Conway JD (2008) Antibiotic cement-coated nails for the treatment of infected nonunions and segmental bone defects. J Bone Joint Surg Am 90(Suppl 4):163–174. doi:10.2106/JBJS.H.00753
Wasko MK, Borens O (2013) Antibiotic cement nail for the treatment of posttraumatic intramedullary infections of the tibia: midterm results in 10 cases. Injury 44(8):1057–1060. doi:10.1016/j.injury.2013.05.001
Chong KW, Woon CY, Wong MK (2011) Induced membranes—a staged technique of bone-grafting for segmental bone loss: surgical technique. J Bone Joint Surg Am 93(Suppl 1):85–91. doi:10.2106/JBJS.J.01251
Blum AL, BongioVanni JC, Morgan SJ, Flierl MA, dos Reis FB (2010) Complications associated with distraction osteogenesis for infected nonunion of the femoral shaft in the presence of a bone defect: a retrospective series. J Bone Joint Surg British 92(4):565–570. doi:10.1302/0301-620X.92B4.23475
Conway JD, Hlad LM, Bark SE (2015) Antibiotic cement-coated plates for management of infected fractures. Am J Orthop 44(2):E49–E53
Tice AD, Hoaglund PA, Shoultz DA (2003) Risk factors and treatment outcomes in osteomyelitis. J Antimicrob Chemother 51(5):1261–1268. doi:10.1093/jac/dkg186
Ueng SW, Wei FC, Shih CH (1999) Management of femoral diaphyseal infected nonunion with antibiotic beads local therapy, external skeletal fixation, and staged bone grafting. J Trauma 46(1):97–103
West WF, Kelly PJ, Martin WJ (1970) Chronic osteomyelitis. I. factors affecting the results of treatment in 186 patients. Jama 213(11):1837–1842
Diefenbeck M, Muckley T, Hofmann GO (2006) Prophylaxis and treatment of implant-related infections by local application of antibiotics. Injury 37(Suppl 2):S95–S104. doi:10.1016/j.injury.2006.04.015
Alemdar C, Azboy I, Atic R, Ozkul E, Gem M, Kapukaya A (2015) Management of infectious fractures with “non-contact plate” (NCP) method. Acta Orthop Belg 81(3):523–529
Pelissier P, Masquelet AC, Bareille R, Pelissier SM, Amedee J (2004) Induced membranes secrete growth factors including vascular and osteoinductive factors and could stimulate bone regeneration. J Orthopaed Res: Off Publ Orthopaed Res Soc 22(1):73–79. doi:10.1016/S0736-0266(03)00165-7
Auregan JC, Begue T (2014) Induced membrane for treatment of critical sized bone defect: a review of experimental and clinical experiences. Int Orthop 38(9):1971–1978. doi:10.1007/s00264-014-2422-y
Stevenson S, Emery SE, Goldberg VM (1996) Factors affecting bone graft incorporation. Clin Orthop Relat Res 324:66–74
Apard T, Bigorre N, Cronier P, Duteille F, Bizot P, Massin P (2010) Two-stage reconstruction of post-traumatic segmental tibia bone loss with nailing. Orthopaed Traumatol, Surg Res : OTSR 96(5):549–553. doi:10.1016/j.otsr.2010.02.010
Villemagne T, Bonnard C, Accadbled F, L’Kaissi M, de Billy B, Sales de Gauzy J (2011) Intercalary segmental reconstruction of long bones after malignant bone tumor resection using primary methyl methacrylate cement spacer interposition and secondary bone grafting: the induced membrane technique. J Pediatr Orthop 31(5):570–576. doi:10.1097/BPO.0b013e31821ffa82
Taylor BC, French BG, Fowler TT, Russell J, Poka A (2012) Induced membrane technique for reconstruction to manage bone loss. J Am Acad Orthopaed Surg 20(3):142–150. doi:10.5435/JAAOS-20-03-142
Prasarn ML, Ahn J, Achor T, Matuszewski P, Lorich DG, Helfet DL (2009) Management of infected femoral nonunions with a single-staged protocol utilizing internal fixation. Injury 40(11):1220–1225. doi:10.1016/j.injury.2009.06.009
Acknowledgments
We thank Yali Deng, GuangYao Jiang, Radiology Department, Southwest Hospital (Chongqing, China), for their assistance in reviewing and rating the radiographs for radiographic signs of bone union.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yu, X., Wu, H., Li, J. et al. Antibiotic cement-coated locking plate as a temporary internal fixator for femoral osteomyelitis defects. International Orthopaedics (SICOT) 41, 1851–1857 (2017). https://doi.org/10.1007/s00264-016-3258-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3258-4