Abstract
Purpose
The purpose of this study was to correlate the pre-operative imaging, vascularity of the proximal pole, and histology of the proximal pole bone of established scaphoid fracture non-union.
Methods
This was a prospective non-controlled experimental study. Patients were evaluated pre-operatively for necrosis of the proximal scaphoid fragment by radiography, computed tomography (CT) and magnetic resonance imaging (MRI). Vascular status of the proximal scaphoid was determined intra-operatively, demonstrating the presence or absence of puncate bone bleeding. Samples were harvested from the proximal scaphoid fragment and sent for pathological examination. We determined the association between the imaging and intra-operative examination and histological findings.
Results
We evaluated 19 male patients diagnosed with scaphoid nonunion. CT evaluation showed no correlation to scaphoid proximal fragment necrosis. MRI showed marked low signal intensity on T1-weighted images that confirmed the histological diagnosis of necrosis in the proximal scaphoid fragment in all patients. Intra-operative assessment showed that 90 % of bones had absence of intra-operative puncate bone bleeding, which was confirmed necrosis by microscopic examination.
Conclusions
In scaphoid nonunion MRI images with marked low signal intensity on T1-weighted images and the absence of intra-operative puncate bone bleeding are strong indicatives of osteonecrosis of the proximal fragment.
Similar content being viewed by others
Introduction
The scaphoid is the most commonly fractured carpal bone, making up 60 % of such fractures [1]. Although the majority of scaphoid fractures heal without surgery, most case series report an approximate 10 % non-union rate [2]. Any fracture that persists for longer than six months is considered a non-union [3]. Non-union can show a distinct pattern of degenerative changes, eventually leading to a scaphoid non-union advanced collapse wrist [4]. In established non-union, the treatment goal, in addition to bone union with restoration of the shape of the scaphoid, should be to re-establish wrist function so that the patient can resume normal activities [5]. These are mostly related to fractures of the proximal pole or to avascular necrosis of the proximal fragment [6, 7]. The main explanation for this is a decreased arterial supply, attributable to the retrograde intraosseous blood supply to the proximal pole that makes fractures in that area more likely to progress to non-union and limits potential healing, and another important reason for non-union is the bone instability [8]. In the surgical treatment of non-union of the proximal pole of the scaphoid, failure rates of approximately 65 % have been reported [9, 10]. In such adverse conditions, determination of the vascular status of the scaphoid segments is essential [11]. Green [12, 13] originally suggested that debriding the proximal pole of the scaphoid and observing the amount of bleeding is the most accurate method for diagnosing avascular necrosis.
Radiography, computed tomography (CT), and magnetic resonance imaging (MRI) are pre-operative diagnostic tests for avascular necrosis of the scaphoid [14, 15]. MRI might be the most accurate, but it is not infallible [16]. Diagnostic confirmation, however, is possible only with a histological examination [17]. It is important to have a pre-operative diagnosis of the vascular status of the non-united proximal segment of the scaphoid to plan the surgical approach [18].
We examined the ability of pre-operative radiography, CT, and MRI to evaluate the vascularity of the proximal segment of the scaphoid as seen intra-operatively, as well as the correlation with the histological analysis of the proximal scaphoid fragment in scaphoid non-union.
Methods
This was a prospective non-controlled experimental study. The study sample comprised patients with non-union of the scaphoid diagnosed by medical interview, physical examination, and radiography, who were treated in the orthopaedic division. The inclusion criterion was skeletally mature patients with non-union of the scaphoid. We excluded patients with acute scaphoid fractures (<six months since the trauma), with scaphoid non-union who previously underwent surgery, a combination of fractures or dislocations of other carpal bones, or any associated bone disorders. This study was approved by the institution research ethics committee.
The following images were assessed pre-operatively by an independent blinded musculoskeletal radiologist for all cases: (1) plain radiographs of the wrist including posteroanterior, posteroanterior in ulnar deviation, lateral, and oblique views; (2) CT scans reconstructions in three planes: coronal (90° elbow flexion, lateral side of the fifth finger touching the table top), axial (fingers spread, palm down on the table top), and sagittal (90° elbow flexion, fingers spread, palm down on the table top), with slice thickness of 1–3 mm in a multislice CT scanner; and (3) MRI with T1-weighted images obtained in the sagittal, coronal, and axial planes using 1.5-T high-field circumferential coils.
For all surgical cases, regardless of the approach used, samples were collected from the proximal segment during surgery. A tourniquet was insufflated after simple elevation of the extremity for exsanguination. Opening the joint capsule, the focus of non-union was identified and then resected. Sufficient bone tissue was removed from the proximal segment of the scaphoid, including the dorsal and volar central areas, en bloc using osteotomes and delicate curettes. The specimen was fixed in 10 % buffered formalin, using a solution volume ten times that of the solid component, and sent for analysis by the pathology department. There, the fixed specimen was decalcified in 10 % nitric acid, cut, and embedded in paraffin. Then sections (5-μm thick) were cut with a microtome and stained with hematoxylin-eosin and Masson’s trichrome.
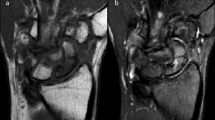
The following criteria were used to diagnose necrosis of the proximal segment of the scaphoid: (1) radiography, increased radiodensity of the proximal segment of the scaphoid compared to the capitate bone as assessed by a radiologist; (2) CT, increased radiodensity of the proximal segment of the scaphoid compared to the capitate bone as assessed by a radiologist; (3) MRI, T1- and T2-weighted sequences with fat saturation in all patients—T1 was chosen because of the possible relationship between low signal intensities on T1-weighted images with osteonecrosis—and the images were stratified according to the T1-weighted signal intensity into low and marked low depending on whether the intensity was greater or less than the muscle signal in the same image as assessed by a radiologist [19] (Figs. 1 and 2); (4) intra-operative vascular status of the proximal segment of the scaphoid after drilling, such that the absence of intra-operative punctuate bone bleeding after the tourniquet is released presupposes avascular necrosis (Fig. 3); and (5) histologically. Histologically, the microscopic changes were categorized into four main types [20–23]: G1 (bone viable, with regeneration and the presence of osteoblasts), in this category, cells were seen on the trabecular surfaces and the bone elements were clearly vital (Fig. 4); G2 (intermediate grade with higher bone viability), loss of regularity of the bone surface without uniformity in the cells of the trabecular surface with possible signs of necrosis, or intense bone remodeling, but still lacking the most complete features of viable bone; G3 (intermediate grade with minimal bone viability), the bone tissues showed clear signs of necrosis (as described above) and minimal signs of regeneration; and G4 (complete necrosis, no osteoblasts), severe, obvious bone necrosis, with well-formed or ruptured bone lamellae, surrounded by soft or necrotic myeloid tissue, or bone lamellae immersed in unfilled areas (Fig. 5). For the statistical analysis, types G1 and G2 were grouped together as viable and types G3 and G4 as necrotic.
Statistical analysis
The data were stored in Excel for organizational purposes and exported to SPSS ver. 19.0. A descriptive statistical analysis was conducted, with means and standard deviations calculated for age, time from injury in months, and number of fractures by region. The results were expressed by sensitivity, specificity, positive predictive value and negative predictive value of the different imaging modalities and peroperative observations, the histology being the reference. For inferential statistics, the χ² test was used to evaluate the correlations between imaging tests and the intra-operative examination and histological findings. The null hypothesis was rejected when p < 0.05.
Results
We evaluated 19 males diagnosed with nonunion of the scaphoid who were treated between November 2008 and December 2011. The mean patient age was 33.7 ± 8.7 years. Table 1 summarizes their baseline characteristics.
The assessment indicated that eight cases had a radiological diagnosis of necrosis of the proximal pole of the scaphoid, of which seven cases had no viable bone on histological analysis, and one patient had viable bone, yielding an agreement of 86 % (7/8). There was a correlation between the radiographic changes and bone necrosis (χ² = 4.968, p = 0.026).
There was no significant correlation between the CT findings and a diagnosis of necrosis of the scaphoid bone (χ² = 2.358, p = 0.125).
The diagnosis of necrosis was confirmed histologically for all scans that indicated marked low signal intensities on T1-weighted images (n = 8; χ² = 10.050, p = 0.002).
Of the bones that were found to be sclerotic during surgery (intra-operative punctate bone bleeding), 90 % were confirmed to be necrotic on intra-operative microscopic examination (χ² = 8.927, p = 0.003).
Results are summarised in Tables 2 and 3.
Discussion
Treatment of nonunion of the scaphoid remains a challenge in hand surgery, particularly when it involves the proximal pole or vascular impairment of the segments [5]. Success treating nonunion of the scaphoid is measured by consolidation, re-establishment of the shape of the scaphoid, pain relief, and recovery of the normal mobility and biomechanics of the wrist [24]. When consolidation of the nonunion is not achieved, the outcome is generally poor: patients develop persistent pain, joint stiffness, and radiocarpal arthritis [25].
Avascular necrosis of the proximal pole of the scaphoid can prevent bone union [26]. However, it is not the only factor; the general condition of microcirculation (age, presence of vascular disease, etc.) can play a role. Dinah and Vickers [27] concluded that smoking was significantly associated with the failure of operative treatment of established non-union of the scaphoid. Vascular impairment following a scaphoid fracture must be conceived as a dynamic condition, ranging from transient ischemia to frank anoxia [28].
A study that compared the use of vascularized versus conventional non-vascularized bone grafts from the distal dorsal radius concluded that vascularized bone gave a higher consolidation rate and superior functional results than the conventional non-vascularized procedure [18].
In a clinical study, Bilic et al. demonstrated that recombinant bone morphogenic protein (BMP) resulted in radiological and clinical repair of scaphoid non-unions with an avascular, necrotic proximal scaphoid after treatment with a vascularized pedicle bone graft [29]. Another study suggested that ultrasound therapy benefits the healing of non-union of the scaphoid after treatment with a vascularized pedicle bone graft [30]. This demonstrates the importance of finding more effective methods for diagnosing and treating non-union of the scaphoid.
In our study, radiographs were effective guides for the diagnosis of necrosis of the proximal segment of the scaphoid, i.e. seven of eight radiographs with increased radiological density showed the bone necrosis histologically (86 %).
Although it was initially considered more accurate than radiography, CT did not correlate strongly with a diagnosis of avascular necrosis of the proximal segment of the scaphoid, corroborating other studies that show conflicting results on this topic [14]. This can be explained in part by the absence of a direct measurement of the radiation density, as Hounsfield units. We suggest that this assessment be included in future studies.
Although some studies show that MRI assessment of the vascularity of the proximal scaphoid does not predict whether a fracture will unite after conservative treatment [31], MRI is still considered the most reliable test for the pre-operative diagnosis of avascular necrosis and is the test used most frequently in this setting [19, 32]. According to Donati et al. [33], MRI without contrast better diagnosed avascular necrosis of the proximal segment of the scaphoid compared to MRI with gadolinium contrast, and tests without contrast were simpler and safer [33]. As in our study, Gunal et al. [34] reported incomplete agreement between MRI and histological tests.
All of the MRI T1-weighted images that had a marked low signal intensity were from patients diagnosed with necrosis of the proximal segment of the scaphoid (grades G3 and G4), showing high sensitivity. Likewise, most MRI images that did not show any signal changes were from patients with viable bone.
Regarding the intra-operative assessment of the presence/absence of bleeding in the proximal segment of the scaphoid, there was 90 % agreement with the histological diagnosis.
Interestingly, the histological examination revealed four distinct patterns in the specimens analysed microscopically. Total bone necrosis was seen in 31 % of the cases, with no viable proximal scaphoid pole, while 62 % of the cases were intermediate grade, with variable areas of cellularity (osteoblasts) or necrosis. This situation is rarely described in the literature, and emphasizes the need to evaluate the vascularity of the proximal scaphoid pole better, because most of the cases were intermediate grade, rather than complete necrosis or fully viable bone. Other pathologies that involve avascular necrosis have been studied in more detail, such as Kienböck’s disease or avascular necrosis of the maxilla [35, 36]. Therefore, our data provide prognostic information regarding this difficult condition, and further experimental and clinical studies are required to determine the successful surgical outcome, depending on the histological pattern.
There are no reports of correlations between imaging tests and intra-operative and histological findings. Cerezal et al. [16] reported that this was a limitation of their study.
Conclusion
In scaphoid nonunion, MRI with marked low signal intensities on T1-weighted images and the absence of intra-operative punctate bone bleeding are strong indicators of osteonecrosis of the proximal fragment.
References
Chang M, Bishop A, Moran S (2006) The outcomes and complications of 1,2-intercompartmental supraretinacular artery pedicled vascularized bone grafting of scaphoid nonunions. J Hand Surg [Am] 31:387–396
Dias J, Brenkel I, Finlay D (1989) Patterns of union in fractures of the waist of the scaphoid. J Bone Joint Surg 71B:307–310
Compson J (1998) The anatomy of acute scaphoid fractures. A three-dimensional analysis of patterns. J Bone Joint Surg 80-B:218–224
Taljanovic M, Karantanas A, Griffith JF, DeSilva GL, Rieke JD, Sheppard JE (2012) Imaging and treatment of scaphoid fractures and their complications. Semin Musculoskelet Radiol 16(2):159–174
Geissler W, Adams JE, Bindra RR, Lanzinger WD, Slutsky DJ (2012) Scaphoid fractures: what’s hot, what’s not. Instr Course Lect 61:71–84
Benis J, Turpin F (2010) The role of imaging in the assessment of vascularity at hand and wrist. Chir Main 29(Suppl 1):S21–S27
Schmitt R, Christopoulos G, Wagner M, Krimmer H, Fodor S, van Schoonhoven J et al (2011) Avascular necrosis (AVN) of the proximal segment in scaphoid nonunion: is intravenous contrast agent necessary in MRI. Eur J Radiol 77(2):222–227
Pao V, Chang J (2003) Scaphoid nonunion: diagnosis and treatment. Plast Reconstr Surg 112:1666–1676
Alnot J, Bellan N, Oberlin C, De Cheveigné DC (1988) Fractures and nonunions of the proximal pole of the carpal scaphoid bone internal fixation by a proximal to distal screw. Ann Chir Main 7:101–108
Barton N (1992) Twenty questions about scaphoid fractures. J Hand Surg (Br) 17:289–310
Zaidemberg C, Siebert J, Angrigiani C (1991) A new vascularized bone graft for scaphoid nonunion. J Hand Surg [Am] 16:474–478
Derby B, Murray P, Shin A, Bueno R, Mathoulin C, Ade T, Neumeister M (2013) Vascularized bone grafts for the treatment of carpal bone pathology. J Hand Surg [Am] 8:27–40
Green D (1985) The effect of avascular necrosis on Russe bone grafting for scaphoid nonunion. J Hand Surg [Am] 10:597–605
Imaeda T, Nakamura R, Miura T, Makino N (1992) Magnetic resonance imaging in scaphoid fractures. J Hand Surg (Br) 17:20–27
Smith M (2009) Using computed tomography to assist with diagnosis of avascular necrosis complicating chronic scaphoid nonunion. J Hand Surg [Am] 34:1037–1043
Cerezal L, Abascal F, Canga A, García-Valtuille R, Bustamante M, del Piñal F (2000) Usefulness of gadolinium-enhanced MR imaging in the evaluation of the vascularity of scaphoid nonunions. Am J Roentgenol 174:141–149
Qu G, von Schroeder HP (2008) Trabecular microstructure at the human scaphoid nonunion. J Hand Surg [Am] 33(5):650–655
Ribak S, Medina C, Mattar R, Ulson H, Resende M, Etchebehere M (2010) Treatment of scaphoid nonunion with vascularised and nonvascularised dorsal bone grafting from the distal radius. Int Orthop 34:683–688
Sakuma M, Nakamura R, Imaeda T (1995) Analysis of proximal segment sclerosis and surgical outcome of scaphoid non-union by magnetic resonance imaging. J Hand Surg (Br) 20:201–205
Fondi C, Franchi A (2007) Definition of bone necrosis by the pathologist. Clin Cases Miner Bone Metab 4(1):21–26
Marcus R (1987) Normal and abnormal bone remodeling in man. Annu Rev Med 38:129–141
McClure J, Smith P (1983) Consequences of avascular necrosis of the femoral head in aluminium-related renal osteodystrophy and the role of endochondral ossification in the repair process. J Clin Pathol 36:260–268
Parfitt A, Drezner M, Glorieux F, Kanis J, Malluche H, Meunier P, Ott S, Recker R (1987) Bone histomorphometry: standardization of nomenclature, symbols, and units. Report of the ASBMR histomorphometry nomenclature committee. J Bone Miner Res 2(6):595–610
Schuind F (1999) Prognostic factors in the treatment of carpal scaphoid nonunions. J Hand Surg [Am] 24:761–776
Buijze G, Ochtman L, Ring D (2012) Management of scaphoid nonunion. J Hand Surg [Am] 37(5):1095–1100
Waitayawinyu T, McCallister W, Katolik L, Schlenker J, Trumble T (2009) Outcome after vascularized bone grafting of scaphoid nonunions with avascular necrosis. J Hand Surg [Am] 34(3):387–394
Dinah A, Vickers R (2007) Smoking increases failure rate of operation for established non-union of the scaphoid bone. Int Orthop 31(4):503–505
Buchler U, Nagy L (1995) The issue of vascularity in fractures and nonunion of the scaphoid. J Hand Surg (Br) 20B(6):726–735
Bilic R, Simic P, Jelic M, Stern-Padovan R, Dodig D, van Meerdervoort H, Martinovic S, Ivankovic D, Pecina M, Vukicevic S (2006) Osteogenic protein-1 (BMP-7) accelerates healing of scaphoid non-union with proximal pole sclerosis. Int Orthop 30(2):128–134
Ricardo M (2006) The effect of ultrasound on the healing of muscle-pediculated bone graft in scaphoid non-union. Int Orthop 30(2):123–127
Dawson J, Martel A, Davis T (2001) Scaphoid blood flow and acute fracture healing. A dynamic MRI study with enhancement with gadolinium. J Bone Joint Surg (Br) 83(6):809–814
Paul P, O’Byrne E, Blancuzzi V, Wilson D, Gunson D, Douglas F, Wang LZ, Mezrich R (1991) Magnetic resonance imaging reflects cartilage proteoglycan degradation in the rabbit knee. Skelet Radiol 20(1):31–36
Donati O, Zanetti M, Nagy L, Bode B, Schweizer A, Pfirrmann C (2011) Is dynamic gadolinium enhancement needed in MR imaging for the preoperative assessment of scaphoidal viability in patients with scaphoid nonunion? Radiology 260:808–816
Gunal I, Ozcelik A, Gokturk E, Ada S, Demirtas M (1999) Correlation of magnetic resonance imaging and intraoperative punctate bleeding to assess the vascularity of scaphoid nonunion. Arch Orthop Trauma Surg 119:285–287
Maurer P, Sandulescu T, Kriwalsky M, Rashad A, Hollstein S, Stricker I, Hölzle F, Kunkel M (2011) Bisphosphonate-related osteonecrosis of the maxilla and sinusitis maxillaris. Int J Oral Maxillofac Surg 40(3):285–291
Stahl S, Hentschel PJ, Held M, Manoli T, Meisner C, Schaller HE, Santos Stahl A (2014) Characteristic features and natural evolution of Kienböck’s disease: five years’ results of a prospective case series and retrospective case series of 106 patients. J Plast Reconstr Aesthet Surg 67(10):1415–1426
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Bervian, M.R., Ribak, S. & Livani, B. Scaphoid fracture nonunion: correlation of radiographic imaging, proximal fragment histologic viability evaluation, and estimation of viability at surgery. International Orthopaedics (SICOT) 39, 67–72 (2015). https://doi.org/10.1007/s00264-014-2579-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2579-4