Abstract
Purposes
To determine if liver-to-portal vein contrast ratio (LPC) correlates with liver function in patients with hepatitis B virus (HBV)-related cirrhosis on gadolinium-ethoxybenzyl-diethylenetriamine penta-acetic acid (Gd-EOB-DTPA)-enhanced MR imaging.
Methods
A total of 92 patients with normal (n = 20) or HBV-related cirrhotic livers graded by Child–Pugh class A (n = 50), B (n = 17) or C (n = 5) who underwent Gd-EOB-DTPA-enhanced 3Tesla MR imaging were retrospectively reviewed. LPC was defined as the signal intensity ratio of liver parenchyma to portal vein on hepatobiliary phase (HBP) acquired at 20 min, and it was compared between normal and cirrhotic livers. The correlation between LPC and hepatic function parameters at HBP after injection was quantitatively analyzed as well.
Results
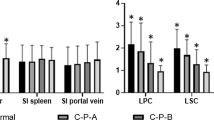
LPC differed between normal and cirrhotic livers significantly (P < 0.001). LPC constantly and significantly decreased from normal to cirrhotic livers with Child–Pugh class C at HBP imaging (P < 0.001). Multiple regression analysis revealed that total bilirubin (P = 0.011), albumin (P < 0.001), and platelet count (P = 0.007) were independent predictors of LPC at HBP imaging. A receiver operating characteristic (ROC) curve analysis revealed that the optimal cutoff value for LPC to distinguish normal group from cirrhotic groups was 2.05 (AUC 0.98) with a sensitivity of 84.1% and a specificity of 100%.
Conclusion
The level of LPC on Gd-EOB-DTPA MR imaging can efficaciously indicate the severity of liver function in patients with HBV-related cirrhosis and was correlated with liver function parameters significantly. It might be used as an alternative imaging biomarker for assessing liver function.




Similar content being viewed by others
References
Van Beers BE, Grandin C, Pauwels S, et al. (1994) Gd-EOB-DTPA enhancement pattern of hepatocellular carcinomas in rats: comparison with Tc-99 m-IDA uptake. J Magn Reson Imaging 4(3):351–354
Weinmann HJ, Bauer H, Frenzel T, Muhler A, Ebert W (1996) Mechanism of hepatic uptake of gadoxetate disodium. Acad Radiol 3(Suppl 2):S232–S234
Schuhmann-Giampieri G, Schmitt-Willich H, Press WR, et al. (1992) Preclinical evaluation of Gd-EOB-DTPA as a contrast agent in MR imaging of the hepatobiliary system. Radiology 183(1):59–64. https://doi.org/10.1148/radiology.183.1.1549695
Reimer P, Rummeny EJ, Daldrup HE, et al. (1997) Enhancement characteristics of liver metastases, hepatocellular carcinomas, and hemangiomas with Gd-EOB-DTPA: preliminary results with dynamic MR imaging. Eur Radiol 7(2):275–280. https://doi.org/10.1007/s003300050150
Pascolo L, Cupelli F, Anelli PL, et al. (1999) Molecular mechanisms for the hepatic uptake of magnetic resonance imaging contrast agents. Biochem Biophys Res Commun 257(3):746–752. https://doi.org/10.1006/bbrc.1999.0454
Muhler A, Heinzelmann I, Weinmann HJ (1994) Elimination of gadolinium-ethoxybenzyl-DTPA in a rat model of severely impaired liver and kidney excretory function. An experimental study in rats. Invest Radiol 29(2):213–216
Purysko AS, Remer EM, Veniero JC (2011) Focal liver lesion detection and characterization with GD-EOB-DTPA. Clin Radiol 66(7):673–684. https://doi.org/10.1016/j.crad.2011.01.014
Hammerstingl R, Huppertz A, Breuer J, et al. (2008) Diagnostic efficacy of gadoxetic acid (Primovist)-enhanced MRI and spiral CT for a therapeutic strategy: comparison with intraoperative and histopathologic findings in focal liver lesions. Eur Radiol 18(3):457–467. https://doi.org/10.1007/s00330-007-0716-9
Akai H, Matsuda I, Kiryu S, et al. (2012) Fate of hypointense lesions on Gd-EOB-DTPA-enhanced magnetic resonance imaging. Eur J Radiol 81(11):2973–2977. https://doi.org/10.1016/j.ejrad.2012.01.007
Kobayashi S, Matsui O, Gabata T, et al. (2012) Relationship between signal intensity on hepatobiliary phase of gadolinium ethoxybenzyl diethylenetriaminepentaacetic acid (Gd-EOB-DTPA)-enhanced MR imaging and prognosis of borderline lesions of hepatocellular carcinoma. Eur J Radiol 81(11):3002–3009. https://doi.org/10.1016/j.ejrad.2012.03.029
Campos JT, Sirlin CB, Choi JY (2012) Focal hepatic lesions in Gd-EOB-DTPA enhanced MRI: the atlas. Insights Imaging 3(5):451–474. https://doi.org/10.1007/s13244-012-0179-7
Tamada T, Ito K, Higaki A, et al. (2011) Gd-EOB-DTPA-enhanced MR imaging: evaluation of hepatic enhancement effects in normal and cirrhotic livers. Eur J Radiol 80(3):e311–e316. https://doi.org/10.1016/j.ejrad.2011.01.020
Fischer MA, Donati OF, Reiner CS, et al. (2012) Feasibility of semiquantitative liver perfusion assessment by ferucarbotran bolus injection in double-contrast hepatic MRI. J Magn Reson Imaging 36(1):168–176. https://doi.org/10.1002/jmri.23611
Verloh N, Haimerl M, Zeman F, et al. (2014) Assessing liver function by liver enhancement during the hepatobiliary phase with Gd-EOB-DTPA-enhanced MRI at 3 Tesla. Eur Radiol 24(5):1013–1019. https://doi.org/10.1007/s00330-014-3108-y
Nishie A, Asayama Y, Ishigami K, et al. (2012) MR prediction of liver fibrosis using a liver-specific contrast agent: superparamagnetic iron oxide versus Gd-EOB-DTPA. J Magn Reson Imaging 36(3):664–671. https://doi.org/10.1002/jmri.23691
Verloh N, Haimerl M, Rennert J, et al. (2013) Impact of liver cirrhosis on liver enhancement at Gd-EOB-DTPA enhanced MRI at 3 Tesla. Eur J Radiol 82(10):1710–1715. https://doi.org/10.1016/j.ejrad.2013.05.033
Verloh N, Utpatel K, Haimerl M, et al. (2015) Liver fibrosis and Gd-EOB-DTPA-enhanced MRI: a histopathologic correlation. Sci Rep 5:15408. https://doi.org/10.1038/srep15408
Lee S, Choi D, Jeong WK (2016) Hepatic enhancement of Gd-EOB-DTPA-enhanced 3 Tesla MR imaging: assessing severity of liver cirrhosis. J Magn Reson Imaging 44(5):1339–1345. https://doi.org/10.1002/jmri.25288
Feier D, Balassy C, Bastati N, et al. (2013) Liver fibrosis: histopathologic and biochemical influences on diagnostic efficacy of hepatobiliary contrast-enhanced MR imaging in staging. Radiology 269(2):460–468. https://doi.org/10.1148/radiol.13122482
Takatsu Y, Kobayashi S, Miyati T, Shiozaki T (2016) A novel method for evaluating enhancement using gadolinium-ethoxybenzyl-diethylenetriamine penta-acetic acid in the hepatobiliary phase of magnetic resonance imaging. Clin Imaging 40(6):1112–1117. https://doi.org/10.1016/j.clinimag.2016.07.001
Lee NK, Kim S, Kim GH, et al. (2012) Significance of the “delayed hyperintense portal vein sign” in the hepatobiliary phase MRI obtained with Gd-EOB-DTPA. J Magn Reson Imaging 36(3):678–685. https://doi.org/10.1002/jmri.23700
Tamada T, Ito K, Sone T, et al. (2011) Gd-EOB-DTPA enhanced MR imaging: evaluation of biliary and renal excretion in normal and cirrhotic livers. Eur J Radiol 80(3):e207–e211. https://doi.org/10.1016/j.ejrad.2010.08.033
Tsuda N, Matsui O (2010) Cirrhotic rat liver: reference to transporter activity and morphologic changes in bile canaliculi–gadoxetic acid-enhanced MR imaging. Radiology 256(3):767–773. https://doi.org/10.1148/radiol.10092065
Tsuboyama T, Onishi H, Kim T, et al. (2010) Hepatocellular carcinoma: hepatocyte-selective enhancement at gadoxetic acid-enhanced MR imaging–correlation with expression of sinusoidal and canalicular transporters and bile accumulation. Radiology 255(3):824–833. https://doi.org/10.1148/radiol.10091557
van Montfoort JE, Stieger B, Meijer DK, et al. (1999) Hepatic uptake of the magnetic resonance imaging contrast agent gadoxetate by the organic anion transporting polypeptide Oatp1. J Pharmacol Exp Ther 290(1):153–157
Geier A, Kim SK, Gerloff T, et al. (2002) Hepatobiliary organic anion transporters are differentially regulated in acute toxic liver injury induced by carbon tetrachloride. J Hepatol 37(2):198–205
Geier A, Dietrich CG, Voigt S, et al. (2003) Effects of proinflammatory cytokines on rat organic anion transporters during toxic liver injury and cholestasis. Hepatology 38(2):345–354. https://doi.org/10.1053/jhep.2003.50317
Planchamp C, Montet X, Frossard JL, et al. (2005) Magnetic resonance imaging with hepatospecific contrast agents in cirrhotic rat livers. Invest Radiol 40(4):187–194
Tschirch FT, Struwe A, Petrowsky H, et al. (2008) Contrast-enhanced MR cholangiography with Gd-EOB-DTPA in patients with liver cirrhosis: visualization of the biliary ducts in comparison with patients with normal liver parenchyma. Eur Radiol 18(8):1577–1586. https://doi.org/10.1007/s00330-008-0929-6
Takao H, Akai H, Tajima T, et al. (2011) MR imaging of the biliary tract with Gd-EOB-DTPA: effect of liver function on signal intensity. Eur J Radiol 77(2):325–329. https://doi.org/10.1016/j.ejrad.2009.08.008
Jiao D, Jin JM (1999) Fast frequency-sweep analysis of RF coils for MRI. IEEE Trans Biomed Eng 46(11):1387–1390
Acknowledgments
No funding was received in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required. This retrospective review of existing data was approved by the institutional review board of The First Affiliated Hospital of Soochow University, and written informed consent was waived for all patients.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, W., Wang, X., Miao, Y. et al. Liver function correlates with liver-to-portal vein contrast ratio during the hepatobiliary phase with Gd-EOB-DTPA-enhanced MR at 3 Tesla. Abdom Radiol 43, 2262–2269 (2018). https://doi.org/10.1007/s00261-018-1462-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1462-y