Abstract
Purpose
This study evaluated the ability of 18F-FDG PET/CT imaging to predict early response to 90Y-radioembolization in comparison with contrast-enhanced CT (CECT) using RECIST and lesion density (Choi) criteria. Progression-free survival (PFS) in patients with liver metastases at 2 years and decline in tumour markers were the primary end-points of the study.
Methods
A total of 121 liver lesions were evaluated in 25 patients (14 men, 11 women) with liver-dominant metastatic colorectal cancer who underwent 18F-FDG PET/CT and CECT before and 6–8 weeks after treatment. Changes in SUVmax, tumour density measured in terms of Hounsfield units and the sum of the longest diameters (LD) were calculated for the target liver lesions in each patient. The patient responses to treatment were categorized using EORTC PET criteria, tumour density criteria (Hounsfield units) and RECIST, and were correlated with the responses of tumour markers and 2-year PFS using Kaplan-Meier plots and the log-rank test for comparison. Multivariate proportional hazards (Cox) regression analysis was performed to assess the effect of relevant prognostic factors on PFS.
Results
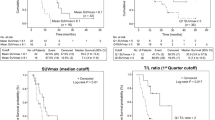
Using 18F-FDG PET/CT response criteria, 15 patients had a partial response (PR) and 10 patients had stable disease (SD), while using RECIST only 2 patients had a PR and 23 had SD. Two patients had a PR, 21 SD and 2 progressive disease using tumour density criteria. The mean changes in SUVmax, sum of the LDs and tumour density after treatment were 2.9 ± 2.6, 7.3 ± 14.4 mm and 1.9 ± 13.18 HU, respectively. Patients who had a PR on 18F-FDG PET/CT had a mean decrease of 44.5 % in SUVmax compared to those with SD who had a decrease of only 10.3 %. The decreases in SUVmax and sum of the LDs were significant (p < 0.0001, p < 0.05, respectively) while the decrease in tumour density was not (p > 0.1065). The responses on the 18F-FDG PET/CT studies were highly correlated with the responses of tumour markers (p < 0.0001 for LDH, p = 0.01 for CEA and p = 0.02 for Ca19-9), while the responses on the CECT studies using both RECIST and tumour density criteria were not significantly correlated with the responses of tumour markers. The responses on 18F-FDG PET/CT studies also significantly predicted PFS (the median PFS in those with a PR was 12.0 months and in those with SD was 5 months, p < 0.0001), while RECIST and tumour density did not significantly predict PFS. Multivariate analysis demonstrated that responses on 18F-FDG PET/CT studies and decreases in SUVmax of ≤2.0 were the strongest predictors of PFS.
Conclusion
Early response assessment to 90Y-radioembolization using 18F-FDG PET/CT is superior to RECIST and tumour density, demonstrating a correlation with tumour markers and significantly predicting PFS in patients with liver metastases. This could enable early response-adapted treatment strategies to be employed.



Similar content being viewed by others
References
Nordlinger B, Guiguet M, Vaillant JC, Balladur P, Boudjema K, Bachellier P, et al. Surgical resection of colorectal carcinoma metastases to the liver. A prognostic scoring system to improve case selection, based on 1568 patients. Association Francaise de Chirurgie. Cancer. 1996;77:1254–62.
Taylor I, Bennett R, Sherriff S. The blood supply of colorectal liver metastases. Br J Cancer. 1978;38:749–56.
Deleporte A, Flamen P, Hendlisz A. State of the art: radiolabeled microspheres treatment for liver malignancies. Expert Opin Pharmacother. 2010;11:579–86.
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–16.
Bruix J, Sherman M, Llovet JM, Beaugrand M, Lencioni R, Burroughs AK, et al. Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol. 2001;35:421–30.
Choi H, Charnsangavej C, Faria SC, Macapinlac HA, Burgess MA, Patel SR, et al. Correlation of computed tomography and positron emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: proposal of new computed tomography response criteria. J Clin Oncol. 2007;25:1753–9.
Weber WA. Positron emission tomography as an imaging biomarker. J Clin Oncol. 2006;24:3282–92.
Larson SM, Schwartz LH. 18F-FDG PET as a candidate for "qualified biomarker": functional assessment of treatment response in oncology. J Nucl Med. 2006;47:901–3.
Weber WA. Use of PET for monitoring cancer therapy and for predicting outcome. J Nucl Med. 2005;46:983–95.
Dierckx R, Maes A, Peeters M, Van De Wiele C. FDG PET for monitoring response to local and locoregional therapy in HCC and liver metastases. Q J Nucl Med Mol Imaging. 2009;53:336–42.
Van den Abbeele AD. The lessons of GIST–PET and PET/CT: a new paradigm for imaging. Oncologist. 2008;13 Suppl 2:8–13.
Young H, Baum R, Cremerius U, Herholz K, Hoekstra O, Lammertsma AA, et al. Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron 'emission tomography: review and 1999 EORTC recommendations. European Organization for Research and Treatment of Cancer (EORTC) PET Study Group. Eur J Cancer. 1999;35:1773–82.
Mac Manus MP, Hicks RJ, Matthews JP, McKenzie A, Rischin D, Salminen EK, et al. Positron emission tomography is superior to computed tomography scanning for response-assessment after radical radiotherapy or chemoradiotherapy in patients with non-small-cell lung cancer. J Clin Oncol. 2003;21:1285–92.
Wahl RL, Jacene H, Kasamon Y, Lodge MA. From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50 Suppl 1:122S–50S.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
Wong CY, Salem R, Raman S, Gates VL, Dworkin HJ. Evaluating 90Y-glass microsphere treatment response of unresectable colorectal liver metastases by [18F]FDG PET: a comparison with CT or MRI. Eur J Nucl Med Mol Imaging. 2002;29:815–20.
Popperl G, Helmberger T, Munzing W, Schmid R, Jacobs TF, Tatsch K. Selective internal radiation therapy with SIR-Spheres in patients with nonresectable liver tumors. Cancer Biother Radiopharm. 2005;20:200–8.
Szyszko T, Al Nahhas A, Canelo R, Habib N, Jiao L, Wasan H et al. Assessment of response to treatment of unresectable liver tumours with 90Y microspheres: value of FDG PET versus computed tomography. Nucl Med Commun. 2007;28:15–20.
Wong CY, Salem R, Qing F, Wong KT, Barker D, Gates V, et al. Metabolic response after intraarterial 90Y-glass microsphere treatment for colorectal liver metastases: comparison of quantitative and visual analyses by 18F-FDG PET. J Nucl Med. 2004;45:1892–7.
Goh V, Padhani AR. Imaging tumor angiogenesis: functional assessment using MDCT or MRI? Abdom Imaging. 2006;31:194–9.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zerizer, I., Al-Nahhas, A., Towey, D. et al. The role of early 18F-FDG PET/CT in prediction of progression-free survival after 90Y radioembolization: comparison with RECIST and tumour density criteria. Eur J Nucl Med Mol Imaging 39, 1391–1399 (2012). https://doi.org/10.1007/s00259-012-2149-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-012-2149-1