Abstract
Fluid overload and prolonged mechanical ventilation lead to worse outcomes in critically ill children. However, the association between these variables in children following congenital heart surgery is unknown. The objectives of this study were to describe the association between fluid overload and duration of mechanical ventilation, oxygen requirement and radiologic findings of pulmonary and chest wall edema. This study is a retrospective chart review of patients who underwent congenital heart surgery between June 2010 and December 2013. Univariate and multivariate associations between maximum cumulative fluid balance and length of mechanical ventilation and OI were tested using the Spearman correlation test and multiple linear regression models, respectively. There were 85 eligible patients. Maximum cumulative fluid balance was associated with duration of mechanical ventilation (adjusted analysis beta coefficient = 0.53, CI 0.38–0.66, P < 0.001), length of stay in the pediatric intensive care unit (Spearman’s correlation = 0.45, P < 0.001), and presence of chest wall edema and pleural effusions on chest radiograph (Mann–Whitney test, P = 0.003). Amount of red blood cells transfused and use of nitric oxide were independently associated with increased duration of mechanical ventilation (P = 0.012 and 0.014, respectively). Fluid overload is associated with prolonged duration of mechanical ventilation and PICU length of stay after congenital heart surgery. Fluid overload was also associated with physiological markers of respiratory restriction. A randomized controlled trial of a restrictive versus liberal fluid replacement strategy is necessary in this patient population, but in the meantime, accumulating observational evidence suggests that cautious use of fluid in the postoperative care may be warranted.
Similar content being viewed by others
Introduction
The postoperative care of children who have undergone congenital heart surgery has significantly improved during the past few years, with dramatic decreases in morbidity and mortality [29]. However, prolonged mechanical ventilation following surgery still remains a problem in these patients, resulting in increased morbidity, mortality, utilization of hospital resources and surgical cancellations [5, 11, 12, 20].
Prolonged mechanical ventilation has been associated with multiple risk factors including fluid overload in congenital heart surgery patients and other critically ill pediatric populations [5, 11, 14, 18, 26]. Fluid overload itself has been associated with negative outcomes in several pediatric critical care settings, including patients on extracorporeal membrane oxygenator (ECMO) therapy for respiratory failure [27], children with multiple organ failure on continuous renal replacement therapy [8, 10], and children with acute lung injury [7].
Fluid overload occurs frequently in the postoperative congenital heart surgery population and is likely multifactorial [5, 14, 26]. It may result from low cardiac output syndrome, capillary leak following cardiopulmonary bypass and postoperative fluid resuscitation. To date, there have been no randomized, controlled trials on the effect of a liberal versus restrictive fluid strategy on clinical outcomes in this patient population. There have been a limited number of observational studies on the association between positive fluid balance and adverse outcomes, including prolonged mechanical ventilation [13, 17, 24]. These studies were limited by the use of secondary analyses of existing data [13], composite outcomes [17] and inclusion of limited age groups. Furthermore, none of these studies used other tools to corroborate the determination of fluid overload such as the presence of pulmonary and chest wall edema, and none of the above studies reported on the relationship between fluid overload and extubation failure.
Therefore, the objective of our study was to determine whether an association exists between length of mechanical ventilation and fluid overload using cumulative fluid balances, radiologic findings (pulmonary edema, chest wall edema and pleural effusion) and the rate of extubation failure in patients following congenital heart surgery.
Materials and Methods
Study Design and Setting
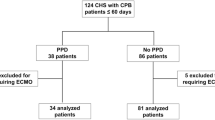
We conducted a single-center, retrospective cohort study at a tertiary care combined medical and surgical pediatric intensive care unit (PICU) at the Children’s Hospital of Eastern Ontario. All patients who underwent cardiovascular surgery and were admitted to PICU during the period from June 2010 to December 2013 had their charts screened for eligibility. The inclusion criteria were (1) patients who underwent surgery for congenital heart disease, (2) newborn to 17-year-olds inclusive, and (3) mechanically ventilated for at least 12 h in PICU. The exclusion criteria were (1) patients who went on ECMO or died before their first extubation attempt, (2) patients with preexistent lung or airway disease, (3) patients who were intubated prior to surgery and (4) patients who were already included in the study. The funding agency had no involvement in the data collection, analysis or interpretation.
Data Collection
The data collected included patient demographics, preoperative, intra-operative and postoperative data. The data collection was censored to a maximum of seven postoperative days. Ten percent of charts were reviewed by two people to ensure accuracy of data.
Length of mechanical ventilation (LMV) in hours was measured as the time from PICU admission to the first extubation attempt. The weight-adjusted cumulative fluid balance was calculated as the difference between total fluid intake since admission (liters), including blood products and total fluid output since admission (liters), divided by weight (kg), and then multiplied by 100 [17, 25]. The cumulative fluid balance was calculated at the end of each 8-h shift. The maximum cumulative fluid balance was defined as the highest level of postoperative fluid accumulation prior to extubation or postoperative day 7 (whichever came first). All patients were ventilated with heated, humidified gas. Extubation failure was defined as the patient requiring re-intubation or noninvasive ventilation within 48 h of the first extubation attempt. Oxygenation support needed was expressed by oxygenation index (OI). OI was calculated as the mean airway pressure multiplied by fraction of inspired oxygen multiplied by 100 divided by arterial partial pressure of oxygen [21], measured at the end of each 8-h shift using the arterial blood gas taken at the closest point to this time. The OI at the time of maximum fluid balance achieved (OIMCFB) and the highest OI (OIMAX) were used in the analysis. All patients who had known right to left shunts postoperatively and/or were expected to have arterial hemoglobin saturation less than 90 % were excluded from the OI analysis.
The presence of pulmonary edema, pleural effusion and chest wall edema as determined from the radiologists’ reports was recorded on every chest radiograph performed on each patient prior to extubation. The presence of these radiographic markers of fluid overload at any point prior to extubation (dichotomized as yes or no) was then correlated with the maximum cumulative fluid balance and LMV. We did not record the degree of pulmonary edema, the size of pleural effusions or the quantification of chest wall thickness as these values are considered subjective, age dependent and relied on comparisons with recent preoperative chest radiographs which were not uniformly available. Radiologists were unaware of patient fluid balances at the time of reading of the chest radiographs.
Other variables recorded included age, presence of trisomy 21, prematurity, use of nitric oxide, cardiopulmonary bypass time (CPB), transfusion requirements (any transfusion received intra- or postoperatively prior to extubation), complexity of the surgical procedure assessed by RACHS-1 [15], delayed chest closure, PRISM-III score measured in the first 12 h after admission [19], the worst vasoactive–inotropic score (VIS) before extubation [9], the maximum serum lactate level prior to extubation, presence of renal failure as defined by RIFLE criteria [23], presence of ventilator-associated pneumonia and non-infectious pulmonary complications (radiologic findings of pneumothorax and atelectasis), use of postoperative diuretics and steroids, and use of peritoneal dialysis. Red blood cell transfusions were used to keep hemoglobin levels ≥9 g/dL for acyanotic congenital heart patients and ≥12 g/dL in cyanotic patients. Nitric oxide was only used in patients with echocardiographic evidence of pulmonary hypertension or in patients with a documented response in PaO2 of ≥5 mmHg or an increase in arterial oxygen saturations of ≥5 % for more than 15 min. Sedation was administered via a standardized protocol that adjusts morphine and lorazepam use depending on the patient’s Modified Comfort Score [2] and State Behavioral Scale [4]. Furosemide was administered to hemodynamically stable patients to achieve adequate urine output as determined by the treating physicians.
Sample Size and Statistical Analysis
Our sample size was powered for our primary objective which was to determine the correlation between maximum cumulative fluid balance and LMV. Previous data from critically ill children with acute lung injury demonstrated a correlation of 0.41 between the presence of fluid overload and LMV [7]. Therefore, given an alpha = 0.05 (two-sided test) and a beta of 0.20, a correlation of r = 0.40 (moderate correlation) would require a sample size of 62 patients. In addition, we wished to examine several risk factors for fluid overload. According to van Belle [28], 10 cases per variable are necessary to obtain reasonably stable estimates of the regression model coefficients. Therefore, in order to analyze up to eight risk factors, we would require a sample of 80 patients. To allow for missing data due to the retrospective nature of this study, we chose a sample size of 85 patients.
Descriptive statistics were be used to summarize the study sample. The univariate associations between maximum cumulative fluid balance and the LMV and OI were tested using Spearman’s correlation test. The univariate associations between fluid balance and other outcomes were tested using: (i) Student’s t-test for continuous variables with normal distribution or (ii) Mann–Whitney or Wilcoxon rank-sum test for continuous variables with skewed distribution.
The unadjusted and adjusted associations between the LMV and the cumulative fluid balance were assessed using simple and multiple linear regression models. Age, complexity of surgical procedure (RACHS-1), cardiopulmonary bypass time, vasotrope–inotrope score (representative of low cardiac output syndrome), use of nitric oxide, transfusion requirements and renal failure were included in the model based on significance of their univariate associations with LMV as well as previous reports of the significance of these specific associations in the literature. Interactions among significant predictors chosen from the literature were also tested [3, 5, 12, 14, 20, 26]. Other diagnostic testing such as residual, covariance and influence analysis was performed to ensure the adequacy of the model. Two-sided P values <0.05 were considered to be statistically significant. The software SPSS was used for the analysis (IBM Corp. Released 2013, IBM SPSS Statistics for Windows, version 22.0. Armonk, NY: IBM Corp).
Results
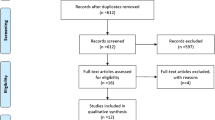
A total of 264 charts were screened, with 129 meeting the inclusion criteria (131 were ventilated <12 h, three were >17 years of age, and one had cardiac but not congenital heart surgery). Of these, 44 were excluded (25 were ventilated prior to surgery, 10 went on ECMO prior to extubation, six had lung or airway disease, one patient died, and two had missing charts). A total of 85 patients were included in the study.
Characteristics of Included Patients
Table 1 summarizes the characteristics of the study population. The median age was 4 months (interquartile range (IQR) 1.3, 5.5), 10.5 % of the patients were born prematurely (9/85) but were all ≥40 weeks of age corrected at the time of surgery, and 14.1 % had trisomy 21 (12/85). Almost half of the surgeries were listed as urgent (39/85, 45.9 %), and almost one-third of patients (28/85, 32.9 %) were on preoperative diuretics for heart failure. The majority of surgeries were of RACHS-1 score 2 (43/85, 50.6 %) or 3 (27/85, 31.8 %), and there were no patients from RACHS-1 category 5 or 6. Seventy-three patients required cardiopulmonary bypass (85.9 %), 64 had aortic cross-clamps applied (75.3 %), and deep hypothermic circulatory arrest was used in 12 patients (14.1 %). The most common cardiac lesions were ASD, tetralogy of Fallot, VSD and PDA (see Table 2 for details of included lesions).
Maximum Cumulative Fluid Balance and Length of Mechanical Ventilation and PICU Length of Stay
The median LMV was 43.1 h (IQR 20.5–86.7). The median maximum cumulative fluid balance was 6.82 % (IQR 3.28–11.71), and the median time to reach this maximum balance was three 8-h shifts (IQR 2–5). Length of mechanical ventilation and maximum cumulative fluid balance were strongly related (Spearman’s test = 0.7, P < 0.001) as shown in Fig. 1. Using a multiple linear regression analysis and adjusting for possible confounders, maximum cumulative fluid balance was still independently associated with LMV (P < 0.01). The use of nitric oxide and transfusion requirement were the only independent risk factors associated with prolonged mechanical ventilation (see Table 3). Maximum cumulative fluid balance was also associated with increased length of stay in PICU [Spearman’s correlation = 0.45, P < 0.001, n = 84 (one patient excluded as an extreme outlier)].
Maximum Cumulative Fluid Balance and Other Outcome Measures
Seventy-six patients were analyzed for the association of maximum cumulative fluid balance and OI (nine patients with postoperative cyanosis due to residual lesions were excluded). Maximum cumulative fluid balance was correlated with maximum OI (Spearman’s test = 0.37, P = 0.01) but not with OI at the time of maximum fluid balance (Spearman’s test = 0.18, P = 0.17, n = 69 excluding cyanotic patients and patients who lost arterial line before maximum fluid balance). The time for maximum OI most often preceded the time to maximum cumulative fluid balance by one 8-h shift (IQR 0–2), and the median time to maximum OI was two 8-h shifts (IQR 1–2). Maximum cumulative fluid balance was associated with the presence of chest wall edema and pleural effusions on chest radiograph at any time prior to extubation (P = 0.003 and 0.012, respectively), and all patients had at least one chest radiograph per day while mechanically ventilated. Prolonged mechanical ventilation was also associated with the presence of chest wall edema and pleural effusions on chest radiographs (P < 0.001 and 0.03, respectively) but not pulmonary edema (P = 0.11).
Extubation failure occurred in 18/85 (21.1 %) patients, five of whom were re-intubated (5.9 %) and 14 of whom required noninvasive ventilation. The maximum cumulative fluid balance was not associated with the rate of extubation failure (P = 0.98) or rate of re-intubation (P = 0.41), and neither was chest wall edema (8/17, 47.1 % versus 10/49, 20.4 %; P = 0.13).
Discussion
Our study found that in congenital heart surgery patients who were ventilated for greater than 12 h, the postoperative maximum cumulative fluid balance was associated with increased duration of mechanical ventilation and increased PICU length of stay but was not associated with an increased rate of extubation failure. Interestingly, longer mechanical ventilation time was also significantly associated with the presence of chest wall edema and pleural effusions on chest radiographs. Our study adds several new important findings to the literature as discussed below.
Previous studies have reported an association between fluid balance and LMV but have used variable definitions of maximum fluid balance making the results difficult to compare [13, 25]. Seguin et al. found that fluid overload peaked by postoperative day 2 and therefore defined fluid overload as the day 2 cumulative fluid overload percent and divided their population into post hoc tertiles of ≤2.7, >2.7 % to <7.1 and ≥7.1 %. Hassinger et al. used a somewhat arbitrary cutoff of a fluid balance 5 % above the preoperative body weight by the end of postoperative day 1. In our study, instead of setting arbitrary cut points to define fluid overload, we used the maximum cumulative fluid balance of each patient regardless of its amount and used this value to determine the association with clinically important outcomes. Using this method, we found that maximum cumulative fluid balance independent of its timing was strongly correlated with the duration of mechanical ventilation and PICU length of stay. Our findings suggest that minimizing fluid balance throughout a patient’s PICU stay may lead to shorter duration of mechanical ventilation and PICU length of stay.
We also found that maximum cumulative fluid balance was significantly associated with the presence of chest wall edema and pleural effusions on chest radiographs, which has not been previously reported. This is an important finding as there has been debate in the literature regarding the value of calculated fluid balances in assessing fluid overload in children and our study is the first to demonstrate that the maximum cumulative fluid balance derived from calculated fluid balances correlates with other independent assessments of patient fluid status [16]. Therefore, the presence of chest wall edema and pleural effusions may serve as a useful adjunct for the assessment of fluid balance and aid clinicians in making decisions regarding extubation in this patient population.
Another important finding in our study is that the association of a positive fluid balance with the duration of mechanical ventilation and PICU length of stay holds true even for patients who have undergone less complex cardiac surgeries (RACHS-1, categories 1–4). This is an important message for smaller centers who may have felt that previous observational studies which included higher-risk congenital heart surgery patients [13, 17, 25] did not apply to their patient population. Furthermore and in contrast to the other studies, we did not find that the length of cardiopulmonary bypass correlated with the duration of mechanical ventilation postoperatively. This may reflect the lower-risk surgeries performed at our center and/or other centers’ specific intra- or postoperative practices.
Like previous studies, this study found an association between a higher maximum cumulative fluid balance and the peak in OI [1, 25]. However, we found that the OI at the time of the maximum cumulative fluid balance and the maximum cumulative fluid balance were not correlated and that the peak in OI often preceded the maximum cumulative fluid balance. These findings suggest that pulmonary edema may occur early postoperatively prior to significant overall fluid overload and that respiratory compromise in these patients may be more related to subsequent perceived restrictive respiratory impairment rather than alveolar disease.
It is interesting to note that in our study, markers of cardiac output (serum lactate and VIS) did not correlate with LMV or maximum cumulative fluid balance. This is in contrast to previous reports suggesting that postoperative cardiac dysfunction is associated with peak cumulative fluid balance (Seguin) and with a composite poor outcome measure that included LMV (Hazle). This difference may be due to performance of higher-risk surgical cases at the other centers with a resulting higher incidence of postoperative low cardiac output syndrome. This is supported by Seguin et al. who found that the need for postoperative inotropes was associated with fluid overload only in patients with the highest peak cumulative fluid balance.
Finally, our study is the first to assess the relationship between maximum cumulative fluid balance and extubation failure and did not show an association between these two variables. It is possible that physicians were reluctant to extubate patients who were perceived as being fluid overloaded and as such delayed their extubations, thus preventing potentially unsuccessful attempts [22]. Although this approach may prevent unsuccessful extubations along with their associated morbidity and mortality [12], it may also result in unnecessary prolongation of mechanical ventilation as fluid overload without pulmonary edema or oxygenation issues has not been definitely shown to result in extubation failure. Future prospective studies are needed to determine whether such patients could be extubated earlier in order to facilitate faster patient recovery and flow through critical care units [20].
A limitation of this study is that it is a small single-center study with a limited sample size and thus may not be generalizable to other institutions. Another potential limitation is that we utilized radiology reports to assess the presence of pulmonary edema, pleural effusions and chest wall thickness rather than separately adjudicating these findings as part of this study. However, we chose to utilize the radiology reports since this was the information available to clinicians at the time and therefore may have influenced their management decisions and subsequent patient outcomes including LMV and OI. In addition, we were only able to determine the association between fluid balance and LMV rather than causation due to the retrospective nature of this study.
Ideally, a randomized controlled trial of a fluid sparing versus liberal fluid strategy would be needed to definitively determine the cause–effect relationship between fluid overload and prolonged mechanical ventilation in postoperative congenital heart surgery patients. However, given the increasing observational evidence suggesting that fluid overload may be associated with adverse clinical outcomes and the challenges inherent in conducting critical care trials in children [6], it would be important to determine whether equipoise still exists on this issue before embarking on such a trial.
We conclude that fluid overload as represented by maximum cumulative fluid balance is associated with prolonged duration of mechanical ventilation and PICU length of stay in patients post-congenital heart surgery. Fluid overload was also associated with physiological markers of respiratory restriction but was not associated with extubation failure in this cohort. A randomized controlled trial of a restrictive versus liberal fluid replacement strategy is necessary in this patient population, but in the meantime, accumulating observational evidence suggests that cautious use of fluid in the postoperative care of these patients may be warranted.
References
Aa Arikan, Zappitelli M, Goldstein SL, Naipaul A, Jefferson LS, Loftis LL (2012) Fluid overload is associated with impaired oxygenation and morbidity in critically ill children. Pediatr Crit Care Med 13:253–258. doi:10.1097/PCC.0b013e31822882a3
Ambuel B, Hamlett KW, Marx CM, Blumer JL (1992) Assessing distress in pediatric intensive care environments: the COMFORT scale. J Pediatr Psychol 17(1):95–109. doi:10.1093/jpepsy/17.1.95
Boone D, Green SB (1991) Predicting with the MMPI the adjustment of juvenile delinquents to institutionalization: does gender make a difference? J Pers Assess 57(1):61–76. doi:10.1207/s15327752jpa5701_9
Curley MA, Harris SK, Fraser KA, Johnson RA, Arnold JH (2006) State Behavioral Scale: a sedation assessment instrument for infants and young children supported on mechanical ventilation. Pediatr Crit Care Med 7(2):107–114. doi:10.1097/01.PCC.0000200955.40962.38
Davis S, Worley S, Mee RB, Harrison AM (2004) Factors associated with early extubation after cardiac surgery in young children. Pediatr Crit Care Med 5(1):63–68. doi:10.1097/01.PCC.0000102386.96434.46
Duffett M, Choong K, Hartling L, Menon K, Thabane L, Cook DJ (2013) Randomized controlled trials in pediatric critical care: a scoping review. Crit Care 17(5):R256. doi:10.1186/cc13083cc13083
Flori HR, Church G, Liu KD, Gildengorin G, Matthay MA (2011) Positive fluid balance is associated with higher mortality and prolonged mechanical ventilation in pediatric patients with acute lung injury. Crit Care Res Pract 2011:854142. doi:10.1155/2011/854142
Foland JA, Fortenberry JD, Warshaw BL, Pettignano R, Merritt RK, Heard ML, Rogers K, Reid C, Tanner AJ, Easley KA (2004) Fluid overload before continuous hemofiltration and survival in critically ill children: a retrospective analysis. Crit Care Med 32(8):1771–1776. doi:10.1097/01.CCM.0000132897.52737.49
Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, Charpie JR, Hirsch JC (2010) Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 11:234–238. doi:10.1097/PCC.0b013e3181b806fc
Goldstein SL, Somers MJ, Baum MA, Symons JM, Brophy PD, Blowey D, Bunchman TE, Baker C, Mottes T, McAfee N, Barnett J, Morrison G, Rogers K, Fortenberry JD (2005) Pediatric patients with multi-organ dysfunction syndrome receiving continuous renal replacement therapy. Kidney Int 67(2):653–658. doi:10.1111/j.1523-1755.2005.67121.x
Harkel AD, van der Vorst MM, Hazekamp MG, Ottenkamp J (2005) High mortality rate after extubation failure after pediatric cardiac surgery. Pediatr Cardiol 26(6):756–761. doi:10.1007/s00246-005-0906-7
Harrison AM, Cox AC, Davis S, Piedmonte M, Drummond-Webb JJ, Mee RB (2002) Failed extubation after cardiac surgery in young children: prevalence, pathogenesis, and risk factors. Pediatr Crit Care Med 3(2):148–152
Hassinger AB, Wald EL, Goodman DM (2014) Early postoperative fluid overload precedes acute kidney injury and is associated with higher morbidity in pediatric cardiac surgery patients. Pediatr Crit Care Med 15(2):131–138. doi:10.1097/PCC.0000000000000043
Ip P, Chiu CSW, Cheung YF (2002) Risk factors prolonging ventilation in young children after cardiac surgery: impact of noninfectious pulmonary complications. Pediatr Crit Care Med 3:269–274
Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI (2002) Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg 123(1):110–118. doi:10.1067/mtc.2002.119064
Lombel RM, Kommareddi M, Mottes T, Selewski DT, Han YY, Gipson DS, Collins KL, Heung M (2012) Implications of different fluid overload definitions in pediatric stem cell transplant patients requiring continuous renal replacement therapy. Intensive Care Med 38(4):663–669. doi:10.1007/s00134-012-2503-6
Ma Hazle, Gajarski RJ, Yu S, Donohue J, Blatt NB (2013) Fluid overload in infants following congenital heart surgery. Pediatr Crit Care Med 14:44–49. doi:10.1097/PCC.0b013e3182712799
Payen V, Jouvet P, Lacroix J (2011) Risk factors associated with increased length of mechanical ventilation in children. Pediatr Crit Care Med 13:152–157. doi:10.1097/PCC.0b013e3182257a24
Pollack MM, Patel KM, Ruttimann UE (1996) PRISM III: an updated Pediatric Risk of Mortality score. Crit Care Med 24(5):743–752
Prakanrattana U, Valairucha S, Sriyoschati S, Pornvilawan S, Phanchaipetch T (1997) Early extubation following open heart surgery in pediatric patients with congenital heart diseases. J Med Assoc Thai 80(2):87–95
Randolph AG (2009) Management of acute lung injury and acute respiratory distress syndrome in children. Crit Care Med 37(8):2448–2454. doi:10.1097/CCM.0b013e3181aee5dd
Randolph AG, Forbes PW, Gedeit RG, Arnold JH, Wetzel RC, Luckett PM, O’Neil ME, Venkataraman ST, Meert KL, Cheifetz IM, Cox PN, Hanson JH (2005) Cumulative fluid intake minus output is not associated with ventilator weaning duration or extubation outcomes in children*. Pediatr Crit Care Med 6:642–647. doi:10.1097/01.PCC.0000185484.14423.0D
Schneider J, Khemani R, Grushkin C, Bart R (2010) Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med 38(3):933–939. doi:10.1097/CCM.0b013e3181cd12e1
Seguin J, Albright B, Vertullo L, Lai P, Dancea A, Bernier PL, Tchervenkov CI, Calaritis C, Drullinsky D, Gottesman R, Zappitelli M (2014) Extent, risk factors, and outcome of fluid overload after pediatric heart surgery*. Crit Care Med 42(12):2591–2599. doi:10.1097/CCM.0000000000000517
Seguin J, Albright B, Vertullo L, Lai P, Dancea A, Bernier P-L, Tchervenkov CI, Calaritis C, Drullinsky D, Gottesman R, Zappitelli M (2014) Extent, risk factors, and outcome of fluid overload after pediatric heart surgery. Crit Care Med 1–9. doi:10.1097/CCM.0000000000000517
Shi S, Zhao Z, Liu X, Shu Q, Tan L, Lin R, Shi Z, Fang X (2008) Perioperative risk factors for prolonged mechanical ventilation following cardiac surgery in neonates and young infants. Chest 134:768–774. doi:10.1378/chest.07-2573
Swaniker F, Kolla S, Moler F, Custer J, Grams R, Barlett R, Hirschl R (2000) Extracorporeal life support outcome for 128 pediatric patients with respiratory failure. J Pediatr Surg 35(2):197–202. doi:10.1016/S0022-3468(00)90009-5
van Belle G (2008) Sample size. In: Statistical rules of thumb. Wiley Series in Probalility and Statistics, Second edn. Wiley, Hoboken. doi:10.1002/9780470377963
Vricella LA, Dearani JA, Gundry SR, Razzouk AJ, Brauer SD, Bailey LL (2000) Ultra fast track in elective congenital cardiac surgery. Ann Thorac Surg 69(3):865–871. doi:10.1016/S0003-4975(99)01306-5
Acknowledgments
This work was funded by a grant from the Children’s Hospital of Eastern Ontario Research Institute.
Conflict of interest
None.
Ethical standard
This research involves human participants. The institutional research ethics board approved this project and did not require informed consent due to its observational and retrospective nature.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sampaio, T.Z.A.L., O’Hearn, K., Reddy, D. et al. The Influence of Fluid Overload on the Length of Mechanical Ventilation in Pediatric Congenital Heart Surgery. Pediatr Cardiol 36, 1692–1699 (2015). https://doi.org/10.1007/s00246-015-1219-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1219-0