Abstract
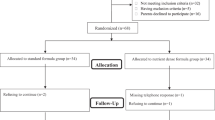
Growth failure is often observed in infants with congenital heart disease (CHD); it is unclear, however, whether growth failure is due to increased total energy expenditure (TEE). An observational study of infants with CHD and surgical intervention within the first 30 days of life and healthy infants of similar age was undertaken. TEE was measured using the doubly labeled water method in 3-month-old infants (n = 15 CHD, 12 healthy) and 12-month-old infants (n = 11 CHD, 12 healthy). Multiple linear regression models were fit to examine the association between health status (CHD vs. healthy) and TEE. The accuracy of equations for calculating TEE was also determined. TEE for CHD infants was not significantly different from healthy infants at 3 and 12 months; TEE in CHD infants was 36.4 kcal/day higher (95 % CI −46.3, 119.2; p = 0.37) and 31.7 kcal/day higher, (95 % CI −71.5, 134.8; p = 0.53) at 3 and 12 months, respectively, compared to healthy infants. The 2002 Dietary Reference Intake (DRI) equation and the 1989 Recommended Dietary Allowance equation over-estimated measured TEE to a lesser extent than CHD specific equations; the 2002 DRI yielded the smallest mean difference between calculated versus measured TEE (difference 79 kcal/day). During the first year of life, TEE of infants with CHD and interventional surgery within the first month of life was not different than age-matched healthy infants. When calculating TEE of ≤12-month-old infants with CHD who have undergone surgical intervention, the 2002 DRI equation may be used as a starting point for estimating initial clinical energy intake goals.

Similar content being viewed by others
References
Academy of Nutrition and Dietetics (2014) Pediatric nutrition care manual, Chicago, IL
Ackerman IL, Karn CA, Denne SC, Ensing GJ, Leitch CA (1998) Total but not resting energy expenditure is increased in infants with ventricular septal defects. Pediatrics 102:1172–1177
Anderson JB, Beekman RH III, Border WL, Kalkwarf HJ, Khoury PR, Uzark K, Eghtesady P, Marino BS (2009) Lower weight-for-age z score adversely affects hospital length of stay after the bidirectional Glenn procedure in 100 infants with a single ventricle. J Thorac Cardiovacs Surg 138:397–404
Barton JS, Hindmarsh PC, Scrimgeour CM, Rennie MJ, Preece MA (1994) Energy expenditure in congenital heart disease. Arch Dis Child 70:5–9
Boctor D, Pilo-Blocka F, McCrindle BW (1999) Nutrition after cardiac surgery for infants with congenital heart disease. Nutr Clin Pract 14:111–115
Burnham N, Ittenbach RF, Stallings VA, Gerdes M, Zackai E, Bernbaum J, Clancy RR, Gaynor JW (2010) Genetic factors are important determinants of impaired growth after infant cardiac surgery. J Thorac Cardiovasc Surg 140:144–149
Centers for Disease Control and Prevention (2014) Congenital heart defects. http://www.cdc.gov/ncbddd/heartdefects/data.html. Accessed 20 Dec 2014
Davis D, Davis S, Cotman K, Worley S, Londrico D, Kenny D, Harrison AM (2008) Feeding difficulties and growth delay in children with hypoplastic left heart syndrome versus d-transposition of the great arteries. Pediatr Cardiol 29:328–333
de Weir J (1949) New methods for calculating metabolic rate with special reference to protein metabolism. J Physiol 109:1–9
Di Maria MV, Glatz AC, Ravishankar C, Quartermain MD, Rush CH, Nance M, William Gaynor J, Goldberg DJ (2013) Supplemental tube feeding does not mitigate weight loss in infants with shunt-dependent single-ventricle physiology. Pediatr Cardiol 34:1350–1356
Dooley KJ, Bishop L (2002) Medical management of the cardiac infant and child after surgical discharge. Crit Care Nurse 25:98–104
Dorfman AT, Marino BS, Wernovsky G, Tabbutt S, Ravishankar C, Godinez RI, Priestley M, Dodds KM, Rychik J, Gruber PJ, Gaynor JW, Levy RJ, Nicolson SC, Montenegro LM, Spray TL, Dominguez TE (2008) Critical heart disease in the neonate: presentation and outcome at a tertiary care center. Pediatr Crit Care Med 9:193–202
Einarson KD, Arthur HM (2003) Predictors of oral feeding difficulty in cardiac surgical infants. Pediatr Nurs 29:315–319
Eskedal LT, Hagemo PS, Seem E, Eskild A, Cvancarova M, Seiler S, Thaulow E (2008) Impaired weight gain predicts risk of late death after surgery for congenital heart defects. Arch Dis Child 93:495–501
Farrell AG, Schamberger MS, Olson IL, Leitch CA (2001) Large left-to-right shunts and congestive heart failure increase total energy expenditure in infants with ventricular septal defect. Am J Cardiol 87:1128–1131 (A10)
Forchielli ML, McColl R, Walker WA, Lo C (1994) Children with congenital heart disease: a nutrition challenge. Nutr Rev 52:348–353
Fuller S, Nord AS, Gerdes M, Wernovsky G, Jarvik GP, Bernbaum J, Zackai E, Gaynor JW (2009) Predictors of impaired neurodevelopmental outcomes at one year of age after infant cardiac surgery. Eur J Cardiothorac Surg 36:40–47
Harrison AM, Davis S, Reid JR, Morrison SC, Arrigain S, Connor JT, Temple ME (2005) Neonates with hypoplastic left heart syndrome have ultrasound evidence of abnormal superior mesenteric artery perfusion before and after modified Norwood procedure. Pediatr Crit Care Med 6:445–447
Hong BJ, Moffett B, Payne W, Rich S, Ocampo EC, Petit CJ (2014) Impact of postoperative nutrition on weight gain in infants with hypoplastic left heart syndrome. J Thorac Cardiovasc Surg 147:1319–1325
Institute of Medicine, Food and Nutrition Board (2005) Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein, and amino acids (macronutrients). National Academies Press, Washington, D.C.
Irving SY, Medoff-Cooper B, Stouffer NO, Schall JI, Ravishankar C, Compher CW, Marino BS, Stallings VA (2013) Resting energy expenditure at 3 months of age following neonatal surgery for congenital heart disease. Congnit Heart Dis 8:343–351
Jadcherla SR, Vijayapal AS, Leuthner S (2009) Feeding abilities in neonates with congenital heart disease: a retrospective study. J Perinatol 29:112–118
Kelleher DK, Laussen P, Teixeira-Pinto A, Duggan C (2006) Growth and correlates of nutritional status among infants with hypoplastic left heart syndrome (HLHS) after stage 1 Norwood procedure. Nutrition 22:237–244
Khalil A, Suff N, Thilaganathan B, Hurrell A, Cooper D, Carvalho JS (2014) Brain abnormalities and neurodevelopmental delay in congenital heart disease: systematic review and meta-analysis. Ultrasound Obstet Gynecol 43:14–24
Knowles RL, Bull C, Wren C, Dezateux C (2012) Mortality with congenital heart defects in England and Wales, 1959–2009: exploring technological change through period and birth cohort analysis. Arch Dis Child 97:861–865
Kogon BE, Ramaswamy V, Todd K, Plattner C, Kirshbom PM, Kanter KR, Simsic J (2007) Feeding difficulty in newborns following congenital heart surgery. Congenit Heart Dis 2:332–337
Kohr LM, Dargan M, Hague A, Nelson SP, Duffy E, Backer CL, Mavroudis C (2003) The incidence of dysphagia in pediatric patients after open heart procedures with transesophageal echocardiography. Ann Thorac Surg 76:1450–1456
Leitch CA, Karn CA, Ensing GJ, Denne SC (2000) Energy expenditure after surgical repair in children with cyanotic congenital heart disease. J Pediatr 137:381–385
Leitch CA, Karn CA, Peppard RJ, Granger D, Liechty EA, Ensing GJ, Denne SC (1998) Increased energy expenditure in infants with cyanotic congenital heart disease. J Pediatr 133:755–760
Lewis A, Hseih V (2005) Congenital heart disease and lipid disorders in children. In: Ekvall S, Ekvall V (eds) Pediatric nutrition in chronic diseases and developmental disorders: prevention, assessment, and treatment, 2nd edn. Oxford University Press, New York, pp 229–235
Licht DJ, Shera DM, Clancy RR, Wernovsky G, Montenegro LM, Nicolson SC, Zimmerman RA, Spray TL, Gaynor JW, Vossough A (2009) Brain maturation is delayed in infants with complex congenital heart defects. J Thorac Cardiovasc Surg 137:529–536; discussion 536–537
Limperopoulos C, Majnemer A, Shevell MI, Rosenblatt B, Rohlicek C, Tchervenkov C (1999) Neurologic status of newborns with congenital heart defects before open heart surgery. Pediatrics 103:402–408
Lohman T, Roche AR, Martorell R (1988) Anthropometric standardization reference manual. Human Kinetics Pub, Champaign
Majnemer A, Limperopoulos C, Shevell MI, Rohlicek C, Rosenblatt B, Tchervenkov C (2009) A new look at outcomes of infants with congenital heart disease. Pediatr Neurol 40:197–204
Malagon I, Onkenhout W, Klok M, van der Poel PF, Bovill JG, Hazekamp MG (2005) Gut permeability in neonates after a stage 1 Norwood procedure. Pediatr Crit Care Med 6:547–549
Marino BS (2013) New concepts in predicting, evaluating, and managing neurodevelopmental outcomes in children with congenital heart disease. Curr Opin Pediatr 25:574–584
Massaro AN, El-Dib M, Glass P, Aly H (2008) Factors associated with adverse neurodevelopmental outcomes in infants with congenital heart disease. Brain Dev 30:437–446
Medoff-Cooper B, Irving SY, Marino BS, Garcia-Espana JF, Ravishankar C, Bird GL, Stallings VA (2011) Weight change in infants with a functionally univentricular heart: from surgical intervention to hospital discharge. Cardiol Young 21:136–144
Medoff-Cooper B, Irving SY (2009) Innovative strategies for feeding and nutrition in infants with congenitally malformed hearts. Cardiol Young 19(Suppl 2):90–95
Menon G, Poskitt EM (1985) Why does congenital heart disease cause failure to thrive? Arch Dis Child 60:1134–1139
Mitchell IM, Davies PS, Day JM, Pollock JC, Jamieson MP (1994) Energy expenditure in children with congenital heart disease, before and after cardiac surgery. J Thorac Cardiovasc Surg 107:374–380
National Research Council (1989) Recommended dietary allowances, 10th edn. National Academies Press, Washington, D.C.
Nicholson GT, Clabby ML, Kanter KR, Mahle WT (2013) Caloric intake during the perioperative period and growth failure in infants with congenital heart disease. Pediatr Cardiol 34:316–321
Racette SB, Schoeller DA, Luke AH, Shay K, Hnilicka J, Kushner RF (1994) Relative dilution spaces of 2H- and 18O-labeled water in humans. Am J Physiol 267:E585–E590
Schoeller DA, Ravussin E, Schutz Y, Acheson KJ, Baertschi P, Jequier E (1986) Energy expenditure by doubly labeled water: validation in humans and proposed calculation. Am J Physiol 250:R823–R830
Schwalbe-Terilli CR, Hartman DH, Nagle ML, Gallagher PR, Ittenbach RF, Burnham NB, Gaynor JW, Ravishankar C (2009) Enteral feeding and caloric intake in neonates after cardiac surgery. Am J Crit Care 18:52–57
Trabulsi J, Ittenbach RF, Schall JI, Olsen IE, Yudkoff M, Daikhin Y, Zemel BS, Stallings VA (2007) Evaluation of formulas for calculating total energy requirements of preadolescent children with cystic fibrosis. Am J Clin Nutr 81:144–151
van der Kuip M, Hoos MB, Forget PP, Westerterp KR, Gemke RJ, de Meer K (2003) Energy expenditure in infants with congenital heart disease, including a meta-analysis. Acta Paediatr 92:921–927
Vogt KN, Manlhiot C, Van Arsdell G, Russell JL, Mital S, McCrindle BW (2007) Somatic growth in children with single ventricle physiology impact of physiologic state. J Am Coll Cardiol 50:1876–1883
World Health Organization (2011) WHO Anthro and macros. http://www.who.int/childgrowth/software/en/. Accessed 20 Dec 2014
Acknowledgements
This research was supported in part from NIH Grants: R01-NR002093, MO1-RR00240, and UL1-RR024134. The authors thank the families who participated in this study and the staff of the Clinical and Translational Research Center (CTRC) for their support.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trabulsi, J.C., Irving, S.Y., Papas, M.A. et al. Total Energy Expenditure of Infants with Congenital Heart Disease Who Have Undergone Surgical Intervention. Pediatr Cardiol 36, 1670–1679 (2015). https://doi.org/10.1007/s00246-015-1216-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1216-3