Abstract
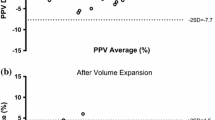
The presence or absence of pulsus paradoxus (PP), defined as an inspiratory decrease greater than 10 mmHg in systolic blood pressure, can have significant diagnostic and therapeutic implications for many clinical conditions including acute asthma, pericardial tamponade, heart failure, hypovolemia, shock states, and the like. However, PP may be difficult to measure in children. Indwelling arterial catheters facilitate the measurement of PP, but this invasive technique generally is reserved for critically ill patients. This study aimed to assess the use of the pulse oximetry plethysmographic waveform (POPW) for the detection of PP in pediatric patients after cardiac surgery. The study enrolled 40 pediatric patients 18 years of age and younger who had invasive blood pressure monitoring with an intraarterial cannula. Systolic pressure variability (SPV) and changes in POPW amplitude (ΔPOPW%), calculated using five consecutive snapshots from every patient’s monitor, were compared using linear regression, Pearson product–moment correlation, the Spearman rank method, and receiver operating characteristic (ROC) curve analysis. A strong correlation existed between respiratory SPV and ΔPOPW% for the detection of PP (r = 0.682; p < 0.0001). A respiratory variation in ΔPOPW% exceeding 25.44% (about one-fourth the amplitude of the tallest POP waveform) allowed detection of PP with a sensitivity of 86.7% and a specificity of 88%. Pulse oximetry is a readily available and easily performed noninvasive means for detecting PP in children.



Similar content being viewed by others
References
Barach P (2000) Pulsus paradoxus. Hosp Physician 1:49–50
Cannesson M, Besnard C, Durand PG et al (2005) Relation between respiratory variations in pulse oximetry plethysmographic waveform amplitude and arterial pulse pressure in ventilated patients. Crit Care 9:R562–R568
Frey B, Butt W (1998) Pulse oximetry for assessment of pulsus paradoxus: a clinical study in children. Intensive Care Med 24:242–246
Gallant SP, Groncy CE, Shaw KC (1978) The value of pulsus paradoxus in assessing the child with status asthmaticus. Pediatrics 61:46–51
Hartert T, Wheeler AP, Sheller JR (1999) Use of pulse oximetry to recognize severity of airflow obstruction in obstructive airway disease, Correlation with pulsus paradoxus. Chest 115:475–481
Holt BD (1995) Pericardial heart disease. Curr Probl Cardiol 22:353–404
Khasnis A, Lokhandwala Y (2002) Clinical signs in medicine: pulsus paradoxus. J Postgrad Med 48:46–49
Knowles GK, Clark TJH (1973) Pulsus paradoxus as a valuable sign indicating severity of asthma. Lancet 2:1356–1359
Kussmaul A (1873) Uber schwielige mediastino-pericarditis und den paradoxen puls. Berl Klin Wochenschr 10:433–435
Martell JA, Lopez JG, Harker JE (1992) Pulsus paradoxus in acute asthma in children. J Asthma 29:349–352
Rebuck AS, Pengelly LD (1973) Development of pulsus paradoxus in the presence of airway obstruction. N Eng J Med 288:66–69
Salyer JW (2003) Neonatal and pediatric pulse oximetry. Respir Care 48:386–396
Shabetai R, Fowler NO, Fenton JC, Masangleay M (1965) Pulsus paradoxus. J Clin Invest 44:1882–1898
Sinex JE (1999) Pulse oximetry: principles and limitations. Am J Emerg Med 17:59–67
Tamburro RF, Ring JC, Womback K (2002) Detection of pulsus paradoxus associated with large pericardial effusions in pediatric patients by analysis of the pulse oximetry waveform. Pediatrics 109:673–677
Acknowledgment
This work was financially supported by the Vice Chancellor for Research of Shiraz University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amoozgar, H., Ghodsi, H., Borzoee, M. et al. Detection of Pulsus Paradoxus by Pulse Oximetry in Pediatric Patients After Cardiac Surgery. Pediatr Cardiol 30, 41–45 (2009). https://doi.org/10.1007/s00246-008-9274-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-008-9274-4