Abstract
Purpose
We examined the prescribing of antiosteoporotic medications pre- and post hospital admission in patients with fragility fractures as well as factors associated with prescribing of these treatments following admission.
Methods
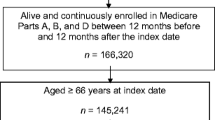
We identified all patients aged ≥55 years at a large teaching hospital between 2005 and 2008 with a fracture using the Hospital In-Patient Enquiry (HIPE) system. These data were linked to prescribing data from the Health Service Executive Primary Care Reimbursement Services (HSE-PCRS) scheme before and after discharge (821 patients). Logistic regression analysis was used to examine the likelihood of prescription of antiosteoporotic medication pre- and post discharge in relation to year of discharge, age, gender, and type of fracture.
Results
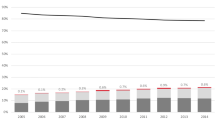
Prescribing of antiosteoporotic treatment before fracture increased from 2.6% [95% confidence interval (CI) 2.23–2.93%] in 2005 to 10.6% (95% CI 9.32–11.86) by 2008, whereas post fracture prescribing increased from 11% (95% CI 9.64–12.36) to 47% (95% CI 43.6–50.3). In patients discharged from hospital in 2007, postfracture prescribing was 31.8% (95% CI 28.66–35.02) at 12 months, increasing to 50.3% (95% CI 46.6–53.9) at 24 months. The highest rate of prescribing was in the 65- to 69-year age group [odds ratio (OR) 8.51, 95% CI 1.75–41.35]. Patients discharged in 2008 were eight times more likely to be treated than patients discharged in 2005 (OR 8.01, 95% CI 4.55–14.09).
Conclusion
The percentage of patients on antiosteoporotic treatment post fracture increased significantly from 2005 to 2008. This may be largely due to the introduction of the Osteoporosis Clinic to the hospital in 2005.

Similar content being viewed by others
References
International Osteoporosis Foundation, http://www.iofbonehealth.org/facts-and-statistics.html#factsheet-category-22.
Haentjens P, Autier P, Collins J, Velkeniers B, Vanderschueren D, Boonen S (2003) Colles fracture, spine fracture, and subsequent risk of hip fracture in men and women: a meta-analysis. J Bone Jt Surg 85A:1936–1943
Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M (2000) Patients with prior fractures have an increased risk of future fractures; a summary of the literature and statistical synthesis. J Bone Miner Res 15:721–739
Schroder HM, Petersen KK, Erlandsen M (1993) Occurrence and incidence of the second hip fracture. Clin Orthop 289:166–169
Report of the National Steering Group on the Prevention of Falls in Older People and the Prevention and Management of Osteoporosis throughout Life, 2008, Strategy to Prevent Falls and Fractures in Ireland's Ageing Population, http://www.hse.ie/eng/Publications/services/Older/Strategy_to_Prevent_Falls_and_Fractures_in_Ireland%e2%80%99s_Ageing_Population_-_Full_report.pdf.
Cheung AM, Feig DS, Kapral M, Diaz-Granados N, Dodin S (2004) Prevention of osteoporosis and osteoporotic fractures in postmenopausal women: recommendation statement from the Canadian Task Force on Preventive Health Care. Can Med Assoc J 170:1665–1667
Epstein S (2006) Update of current therapeutic options for the treatment of postmenopausal osteoporosis. Clin Ther 28:151–173
Mauck KF, Clarke BL (2006) Diagnosis, screening, prevention, and treatment of osteoporosis. Mayo Clin Proc 81:662–672
Bellantonio S, Fortinsky R, Prestwood K (2001) How well are community-living women treated for osteoporosis after hip fracture? J Am Geriatr Soc 49:1197–1204
Castel H, Bonneh DY, Sherf M, Liel Y (2001) Awareness of osteoporosis and compliance with management guidelines un patients with newly diagnosed low-impact fractures. Osteoporos Int 12:559–564
Cuddihy M-T, Gabriel SE, Crowson CS et al (2002) Osteoporosis intervention following distal forearm fractures- a missed opportunity? Arch Intern Med 162:421–426
Elliott-Gibson V, Bogoch ER, Jamal SA, Beaton DE (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int 15:767–778
Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD (2006) Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum 35:293–305
Kamel HK, Hussain MS, Tariq S, Perry HM 111 and Morley JE (2000) Failure to diagnose and treat osteoporosis in elderly patienst hospitalized with hip fracture, Am J Med 109(4):326–328
Khan SA, de Geus C, Russell AS (2001) Osteoporosis follow-up after wrist fractures following minor trauma. Arch Intern Med 161:1309–1312
Pal B (1999) Questionnaire survey of advice given to patients with fractures. BMJ 318:500–501
Smith MD, Ross W, Ahern MJ (2001) Missing a therapeutic window of opportunity: an audit of patients attending a tertiary teaching hospital with potentially osteoporotic hip and wrist fractures. J Rheumatol 28:2504–2508
Solomon DH, Morris C, Cheng H and et al. (2005) Medication use patterns for osteoporosis: an assessment of guidelines, treatment rates, and quality improvement interventions., Mayo Clin Proc, 194-202.
Torgerson DJ, Dolan P (1998) Prescribing by general practionners after an osteoporotic fracture. Ann Rheum Dis 57:378–379
Health Service Executive (2008) Statistical analysis of claims and payments, national shared services primary care reimbursement Service.
Cadarette Suzanne M, Katz Jeffrey N, Alan BM, Raisa L, Stedman Margaret R, Choudhry Niteesh K, Solomon Daniel H (2008) Trends in drug prescribing for osteoporosis after hip fracture, 1995-2004. J Rheumatol 35:319–326
Chakravarthy J, Ali A, Lyengar S, Porter K (2008) Secondary prevention of fragility fractures by orthopaedic teams in the UK: a national survey. Clin Pract 62:382–387
Simonelli C, Killeen K, Mehle S, et al. (2002) Barriers to osteoporosis identification and treatment among primary care physicians and orthopedic surgeons, Mayo Clinic Proc, 334-8.
The National Institute of Clinical Excellence, 2008, Osteoporosis - secondary prevention including strontium ranelate, http://guidance.nice.org.uk/TA161.
The National Institute of Clinical Excellence (2008) Osteoporosis - primary prevention: alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women, http://guidance.nice.org.uk/TA160.
Black DM, Cummings SR, Karpf DB, Cauley JA, Thompson DE, Nevitt MC et al (1996) Randomised trial of effetct of alendronate on risk of fracture in women with existing vertebral fractures. Fracture intervention trial research group. Lancet 348:1535–1541
Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C et al (2002) Meta-analyses of therapies for postmenopausal osteoporosis. 1X. Summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 23:570–578
Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA et al (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the fracture intervention trial. JAMA 280:2077–2082
Harris ST, Watts NB, Genant HK, McKeever CD, Hangartner T, Keller M et al (1999) Effects of risedronate treatment on vertebral and nonvertebral fractures in women with postmenopausal osteoporosis: a randomized controlled trial. Vertebral efficacy with risedronate therapy (VERT) study group. JAMA 282:1344–1352
Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML et al (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral efficacy with risedronate therapy (VERT) study group. Osteoporos Int 11:83–91
Stevenson M, Lloyd Jones M, De Nigris E, Brewer N, Davis S, Oakley J (2005) A systematic review and economic evaluation of alendronate, etidronate, risedronate, raloxifene and teriparatide for the prevention and treatment of postmenopausal osteoporosis. Health Technol Assess 9:1–160
McGowan B, Bennett K, Barry M, Canny M (2008) The utilisation and expenditure of medicines for the prophylaxis and treatment of osteoporosis. IMJ 101:38–41
Bliuc D, Eisman JA, Center JR (2006) A randomized study of two different information-based interventions on the management of osteoporosis in minimal and moderate trauma fractures. Osteoporos Int 17:1309–1317
Jaglal SB, Cameron C, Hawker GA et al (2006) Development of an integrated-care delivery model for post-fracture care in Ontario. Can Osteoporos Int 17:1337–1345
Skedros JG, Holyoak JD, Pitts TC (2006) Knowledge and opinions of orthopaedic surgeons concerning medical evaluation and treatment of patients with osteoporotic fracture. J Bone Joint Surg Am 88:18–24
Kuo I, Ong C, Simmons L, Bliuc D, Eisman J, Center J (2007) Successful direct intervention for osteoporosis in patients with minimal trauma fractures. Osteoporos Int 18:1633–1639
Hawker G, Ridout R, Ricupero M, Jaglal S, Bogoch E (2003) The impact of a simple fracture clinic intervention in improving the diagnosis and treatment of osteoporosis in fragility fracture patients. Osteoporos Int 14:171–178
Tuck SP, Raj N, Summers GD (2002) Is distal forearm fracture in men due to osteoporosis? Osteoporos Int 13:630–636
Acknowledgements
We thank the Health Research Board in Ireland for providing funding for this project. We also thank the HSE-PCRS scheme for providing data on which the study was based, and the staff in the Coding Office at St. James’s Hospital, Dublin, who provided the HIPE data and facilitated the linkage of the data sets.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Distribution of the International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) codes used to identify typical and atypical osteoporotic-type fractures
Rights and permissions
About this article
Cite this article
McGowan, B.M., Bennett, K., Marry, J. et al. Primary-care prescribing of anti-osteoporotic-type medications following hospitalisation for fractures. Eur J Clin Pharmacol 67, 301–308 (2011). https://doi.org/10.1007/s00228-010-0942-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-010-0942-y