Abstract
Introduction
The initially postulated superior neurocognitive effectiveness of second-generation antipsychotics is currently under debate.
Methods
A prospective, randomized, open-label study was carried out to compare the long-term neurocognitive effectiveness of haloperidol, olanzapine, and risperidone in the first episode of schizophrenia spectrum disorders. A final sample of 79 patients randomized to haloperidol (N = 28), olanzapine (N = 23), or risperidone (N = 28) who completed clinical and cognitive evaluations at baseline and 3-year follow-up was included in the final analysis. Forty-one healthy individuals were also included in the final analysis. The main outcome measure was cognitive changes at 3-year follow-up. Due to the fact that some of the patients had switched their initially prescribed antipsychotic medication during the course of the study (6 out of 28 in haloperidol group, 18 out of 23 in olanzapine group, and 24 out of 28 in risperidone group continued with the initial study drug at 3-year assessment), we have also conducted a per protocol analysis.
Results
Overall, cognitive changes were similar in the three treatment groups and controls, although a greater improvement in Rey Auditory Verbal Learning Test, Digit Symbol, and Iowa Gambling Test was found in the treatment groups. The better performance observed on Rey Auditory Verbal Learning Test and Digit Symbol in olanzapine treatment group was likely explained by the lower prevalence of use of antimuscarinic drugs. These results were essentially similar to those found in the intention-to-treat analysis.
Conclusions
The major conclusion of this study is that haloperidol, olanzapine, and risperidone have not demonstrated substantial neurocognitive effectiveness, improving cognitive deficits present in the early phases of the illness. The study also underscores the importance of exploring new drugs for the treatment of cognitive impairments and associated functional disabilities in schizophrenia.
Similar content being viewed by others
Introduction
Cognitive enhancement is a primary goal in treating individuals with schizophrenia. Cognitive deficits are already present at the first break of the illness (Hoff et al. 2005), seem to remain stable during early phases (Bozikas and Andreou 2011), and noticeably influence daily functioning (Green 1996). Differences among antipsychotics in terms of cognitive effectiveness have turned out to be a topic of increasing research interest (Carpenter and Gold 2002). The initially postulated superior neurocognitive effectiveness of second-generation antipsychotics (SGAs) compared to first-generation antipsychotics (FGAs) is currently under debate (Keefe et al. 1999; Woodward et al. 2005), particularly when considering low doses of FGAs in first-episode psychosis (FEP) patients (Keefe et al. 2004; Davidson et al. 2009). The magnitude of cognitive score improvements observed with antipsychotics was compatible with practice effects similarly observed in healthy controls (Goldberg et al. 2007). Short-term clinical trials in which patients undertake several cognitive assessments are particularly vulnerable to the effect of repeated exposure to the tests (Green et al. 2002). Thus, long-term studies would be of great value to evaluate the differential benefits exerted by antipsychotic drugs on cognitive performance (Harvey et al. 2005; Keefe et al. 2006). The aim of this investigation is to investigate the cognitive effects of haloperidol, risperidone, and olanzapine in first-episode psychosis at the long term (3 years). We hypothesized that the three antipsychotic treatments would result in different effectiveness to improve long-term cognitive deficits of psychosis. Some of these differences might be reduced after controlling the impact of extrapyramidal symptoms and antimuscarinic medication.
Methods
Study setting and financial support
Data for the present investigation were obtained from an ongoing epidemiological and 3-year longitudinal intervention program of first-episode psychosis (PAFIP) conducted at the outpatient clinic and inpatient unit at the University Hospital Marqués de Valdecilla, Spain. Conforming to international standards for research ethics, this program was approved by the local institutional review board. Patients meeting inclusion criteria provided written informed consent to be included in the PAFIP. The Mental Health Services of Cantabria provided funding to implement the program. No pharmaceutical company supplied the program with any financial support. A more detailed description of our program has been previously reported (Pelayo-Teran et al. 2008).
Subjects
From February 2001 to February 2005, all referrals to PAFIP were screened for patients who met the following criteria: (1) 15–60 years old; (2) living in the catchment area; (3) experiencing their first episode of psychosis; (4) no prior treatment with antipsychotic medication or, if previously treated, a total life time of adequate antipsychotic treatment of less than 6 weeks; and (5) DSM-IV criteria for brief psychotic disorder, schizophreniform disorder, schizophrenia, or schizoaffective disorder. Patients were excluded for any of the following reasons: meeting DSM-IV criteria for drug dependence, meeting DSM-IV criteria for mental retardation, and having a history of neurological disease or head injury. The diagnoses were confirmed using the Structured Clinical Interview for DSM-IV (First et al. 1996) carried out by an experienced psychiatrist 6 months after the baseline visit. Our operational definition for a “first episode of psychosis” included individuals with a non-affective psychosis (meeting the inclusion criteria defined above) who have not received previously antipsychotic treatment regardless of the duration of psychosis. In the current study, the patients with a diagnosis of schizoaffective disorder at the 6-month diagnostic interview (DSM-IV criteria) were excluded from the analyses.
A group of healthy volunteers who had no current or past history of psychiatric illness, including substance dependence and neurological or general medical disorders, as determined by the abbreviated version of the Comprehensive Assessment of Symptoms and History (Andreasen et al. 1992), was also longitudinally studied. The absence of psychosis in first-degree relatives was assessed by clinical records and family interview. After a detailed description of the study, each healthy subject gave written informed consent to participate, in accordance with the local ethics committee.
Study design
This is a prospective, randomized, open-label study. Patients who agreed to participate underwent a complete evaluation of sociodemographic and clinical variables before random assignment to treatment (olanzapine, risperidone, or haloperidol). We used a simple randomization procedure. A computer-generated randomization list was drawn up by a statistician. At study intake, all but three patients were antipsychotic naïve. Rapid titration schedule (5 day), until optimal dose was reached, was as a rule used unless severe side effects occur. Dose ranges were 5–20 mg/day for olanzapine, 3–6 mg/day for risperidone, and 3–9 mg/day for haloperidol. At the treating physician’s discretion, the dose and type of antipsychotic medication could be changed based on clinical efficacy and the profile of side effects during the follow-up period. Antimuscarinic medications lormetazepam and clonazepam were permitted for clinical reasons. No antimuscarinic agents were administered prophylactically. Antidepressants and mood stabilizers were permitted if clinically needed.
The assessment of adherence to antipsychotic drugs in patients with psychotic illness is complex (Velligan et al. 2010). Although direct or objective measures including pill count, blood or urine analysis, electronic monitoring, and electronic refill records would be desirable, in the real world of the clinical practice, they are difficult to consistently implement. Unfortunately, each method used to assess adherence to oral medications in this population has its own drawbacks. To overcome the limitation of self-report methodologies, we decided to gather information from different sources and assessors. Adherence to antipsychotic drugs was assessed by the information obtained from patients and close relatives by the staff (nurse, social worker, and psychiatrists) involved in the clinical follow-up. For the present investigation, patients were consensually dichotomized into having a good (defined as patients regularly taking at least 90 % of prescribed medication) and a poor adherence (medium or poor compliance) during the 3-year follow-up. Adherence categorization was done at 3-year evaluation and was based on the information gathered from patient and close relatives.
The Scale for the Assessment of Positive Symptoms (SAPS) (Andreasen 1984), Scale for the Assessment of Negative symptoms (SANS) (Andreasen 1983), and Calgary Depression Scale for Schizophrenia (CDSS) (Addington et al. 1994) were used to evaluate clinical symptomatology. The Simpson–Angus Rating Scale (SARS) (Simpson and Angus 1970) and Barnes Akathisia Scale (BAS) (Barnes 1989) were used to assess side effects. The same trained psychiatrist (BC-F) completed all clinical assessments. For the purpose of the present study, baseline and 3-year assessments were considered.
Cognitive functioning was assessed in patients and controls at four points: baseline, 6 months, 1 year, and 3 years after the initialization of antipsychotic treatment. The cognitive assessment at baseline was carried out when clinical status of patients was permitted in order to maximize cooperation. A detailed description of cognitive battery has been described elsewhere (Gonzalez-Blanch et al. 2007). Cognitive testers were blind to medications, adverse event status, and use of concomitant medications. Briefly, the cognitive tests comprised nine cognitive domains, with outcome measures in parenthesis: (1) verbal memory, Rey Auditory Verbal Learning Test (RAVLT) (two measures were obtained: total number of words recalled over learning trials and number of words recalled from the list after delay period); (2) visual memory, Rey Complex Figure Test (long-term recall measure); (3) motor coordination, Grooved Pegboard (GP) (time to complete with dominant hand); (4) executive functions, Trail Making Test B (TMT-B) (time to complete) and FAS, the fluency test (number of words in time limit); (5) working memory, Wechsler Adult Intelligence Scale (WAIS) III-Backward Digits (BD) (total score); (6) speed of processing, WAIS III-Digit Symbol (DS) (standard total score); (7) attention, Continuous Performance Test–Degraded Stimulus (total number of correct responses); and finally, (8) decision-making capacity: Iowa Gambling Task (difference between advantaged and disadvantaged choices); (9) the WAIS III subtest of vocabulary (number of words generated) was used as a covariate to control the effect of premorbid IQ.
In order to calculate a measure of global cognitive functioning (GCF), according to previous methodology (Reichenberg et al. 2008), the raw cognitive scores were converted to Z scores using the mean and standard deviation of a healthy control group. TMT-B and GP scores were multiplied by (−1) previously in order to reverse their raw scores towards the same and positive direction (the higher and the better) as the rest of tests. The Z scores were converted to T scores, which were averaged to obtain the GCF measure.
For the present investigation, baseline and 3-year follow-up evaluations have been analyzed. Cognitive effectiveness of antipsychotics in this sample at short time (1 year) has been previously reported (Crespo-Facorro et al. 2009).
Statistical analyses
Independent sample t tests were used to compare patients and controls on age, years of education, and premorbid IQ. Chi-square (χ 2) tests were utilized to compare frequencies of baseline characteristics. The proportion of patients who were compliant; the frequency of patients who used hypnotics, mood stabilizers, antimuscarinics, benzodiazepines, or antidepressants; and the Barnes Akathisia and Simpson–Angus scales were categorically analyzed among groups by χ 2 test. Observed cases analysis was conducted. Effectiveness analyses were based on intention-to-treat populations, defined as patients who were randomly assigned to a treatment and underwent baseline and 3-year follow-up cognitive assessments. In addition, we have also conducted an analysis based on per protocol populations, defined as patients who maintained their initial antipsychotic treatment throughout the study. Effect size was calculated as a standardized Z score by dividing the difference between assessment means by pooled SD.
Given that the primary aim of this study was to test the hypothesis that the three antipsychotic treatments would result in different effectiveness to improve cognitive deficits, repeated measures analysis of covariance (ANCOVA) was performed for each cognitive variable. For the primary analysis, the between-subject factor was the group (haloperidol, risperidone, and olanzapine), and the within-subject factor was time (baseline and 3 years). Effects of time (longitudinal dimension), group (cross-sectional dimension), and time by group (interaction effect) were examined. All post hoc comparisons were Bonferroni corrected. The Greenhouse–Geisser corrections were used when the assumption of sphericity was violated. Secondly, we compared performance of treatment groups with that of the control group. Using the repeated ANCOVA measures, factors in this model were grouped (haloperidol, risperidone, olanzapine, and controls) as the between-subject factor and time (baseline and 3 years) as the within-subject factor. A main effect for time in absence of a significant group–time interaction would be interpreted as representing practice effects.
In an additional set of analyses, we attempted to control the effect of cognitive baseline scores and other relevant sociodemographic variables on cognitive score changes. Treatment groups were compared by means of univariate ANCOVA in change scores. These change scores were calculated for each cognitive domain by subtracting basal from 3-year scores. In this analysis, baseline performance was used as the covariate.
Other secondary variables might have affected cognitive changes. Pearson’s exploratory correlational analysis was used to determine the potential associations between cognitive and clinical change scores (total scores of SAPS, SANS, and CDSS) and the severity of adverse effects (BAS and SARS) at 3 years. Owing to the large amount of correlations conducted, the level of significance was set at p < 0.01 for the analysis of correlates.
The Statistical Package for the Social Sciences, version 15.0, was used for statistical analyses. All statistical tests were two tailed, and significance was determined at the 0.05 level, but in the analysis of correlations.
Results
Description of study cohort
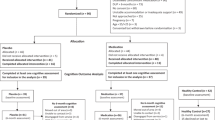
Figure 1 shows the trial profile. Of 243 individuals who were referred to PAFIP, 174 patients met inclusion criteria and gave written consent to their participation in the study and were randomly assigned to treatment. At the baseline, 1.7 % (N = 3) of patients reported some prior treatment. The mean self-reported duration of prior treatment was 4 weeks (SD = 2; range = 2–6). All (N = 173), but one Hispanic, were white Caucasian.
Demographic and clinical characteristics
Demographic and clinical characteristics of patients and controls are shown in Table 1. There were no statistically significant differences in relevant sociodemographic and clinical characteristics between the treatment groups and healthy volunteers (all ps > 0.06). The three groups had a similar severity of psychopathology at baseline, and there were no differences in the amount of clinical improvement at 3 years. Demographic data of each subgroup and controls which completed a given cognitive domain are available under request.
Pharmacological treatments
Patients were initially randomized to haloperidol (N = 56), olanzapine (N = 55), and risperidone (N = 63). Twenty-eight haloperidol, 23 olanzapine, and 28 risperidone individuals completed baseline and 3-year cognitive assessments (see Fig. 1). Mean (SD) and median antipsychotic doses during follow-up were at 3 years: for olanzapine, a mean of 8.7 (4.6) and a median of 7.5 mg/day; for risperidone, a mean of 2.9 (1.4) and a median of 3 mg/day; and for haloperidol, a mean of 3.2 (1.9) and a median of 2.5 mg/day At 3-year assessment, the mean daily antipsychotic dose in chlorpromazine equivalents (Andreasen et al. 2010) was 254.98 mg/day (haloperidol group, 228.26 mg/day; risperidone group, 293.06 mg/day; olanzapine group, 241.15 mg/day). In overall, a greater proportion of haloperidol and risperidone required antimuscarinics during follow-up (χ 2 = 7.22; p = 0.03). At 3-year assessment, two haloperidol, zero olanzapine, and four risperidone patients required antimuscarinics; zero haloperidol, four olanzapine, and two risperidone required benzodiazepines; just one haloperidol required stabilizers; one haloperidol, zero olanzapine, and two risperidone required antidepressants; and no one required hypnotics.
Comparison of cognitive change between treatment groups
The results of cognitive performances and ANCOVA intention-to-treat analysis are described in Table 2. As in the case of patients, the control sample size varies from one test to another due to some cognitive test being sporadic, unfinished, or missing. The analysis of group effects in the ANCOVA revealed that olanzapine group outperformed haloperidol group in RAVLT (long-term recall) (p = 0.026), and also, olanzapine patients significantly outperformed risperidone individuals in Digit Symbol (p = 0.03) at 3-year assessment.
The longitudinal follow-up analysis showed that a significant score increases in all cognitive domains (all p values of <0.05) with the exception of Continuous Performance Test (CPT) (p = 0.37). The mean performance for all three treatment groups significantly improved at 3-year follow-up, with effect sizes ranging from −0.417 to 0.407 in the haloperidol group, from −0.451 to 0.267 for olanzapine, and from −0.301 to 0.264 in the risperidone group. Time–group interactions did not reach significance in any cognitive domain (all p values of ≥0.17).
The results of univariate ANCOVA comparing change scores between treatment groups showed that RAVLT (long-term recall) and Iowa Gambling Task performance increases from baseline to 3-year evaluation were greater in olanzapine group than those in haloperidol individuals. In addition, Digit Symbol change scores showed a greater increase in olanzapine than in risperidone group (p = 0.02).
Due to the fact that some of the patients had switched their initially prescribed antipsychotic medication during the course of the study, we have also conducted a per protocol analysis. The results of the repeated measures ANCOVA and univariate ANCOVA of those patients who maintained their initial antipsychotic medications (per protocol analysis) are described in Table 3. These results were essentially similar to those found in the intention-to-treat analysis; a significant between-group difference on univariate ANCOVA was observed in change score of RAVLT (long-term recall) (p = 0.03). This difference was due to the fact that olanzapine increased performance from baseline to 3 years in a greater degree than the other two groups, although pairwise comparison significance was not reached [olanzapine vs. haloperidol (p = 0.07) and olanzapine vs. risperidone (p = 0.07)].
Patterns of cognitive changes in controls and treatment groups
In a set of secondary analyses, we sought to determine whether the above-mentioned cognitive changes over time in patients were equivalent to practice effects in healthy volunteers. Cognitive performance in patients and healthy controls is shown also in Table 2.
The analysis of between-group effects (haloperidol, risperidone, olanzapine, and controls) revealed that the control group had a better cognitive performance than treatment groups in all cognitive tasks (all p values are ≤0.02) with the exception of FAS (p = 0.53), Rey Complex Figure (p = 0.11), and Iowa Gambling Task (p = 0.20). The within-group analysis observed that the four groups improved in all cognitive scores at 3 years (all p values of <0.001), but in FAS (p = 0.46) and in CPT (p = 0.33). Finally, the analysis of the time–group interaction did not show significance differences in any cognitive domain except in the global score (p = 0.03). The difference was determined by controls showing a minor global cognitive improvement over patient groups. Once baseline performance was controlled in the univariate ANCOVA of change scores, this differential evolution of global score faded away (p = 0.38; see Table 4).
The univariate ANCOVA showed that there were overall differences between groups in the magnitude of changes in RAVLT (learning) (p = 0.001) where controls increased their performance in a greater degree than haloperidol and olanzapine patients. In the case of RAVLT (long-term recall), haloperidol was the only group that increased scores in a lesser degree (p = 0.001) than controls. Similarly, the magnitude of change (increase) in controls was also greater in the case of Digit Symbol (p < 0.001), when compared to haloperidol (p = 0.006) and risperidone (p < 0.001).
Relationship between cognitive change, clinical efficacy, and adverse events
We next explored the association of treatment-related changes in cognitive variables and clinical symptom improvements (from baseline to 3 years) through Pearson’s correlational analyses. In the risperidone group, improvements in positive symptoms correlated with greater improvements in the Rey Complex Figure (r = −0.415; p = 0.03). No other significant correlations were found (data are available upon request).
The proportion of patients with treatment-emergent extrapyramidal symptoms (EPS) at 3 years (a total score higher than 2 on the Simpson–Angus Rating Scale at 3 years, given a total score of 2 or less at baseline) was the same in the three treatment groups (χ 2 = 1.98; p = 0.37).
The percentage of patients with treatment-emergent akathisia at 3 years (Barnes Rating Scale global score of 2 or more at 3 years, given a global score of less than 2 at baseline visit) was neither different among treatment groups nor at 3 years (χ 2 = 3.06; p = 0.22).
We also examined the association of the severity of akathisia (mean global score of BARS) at 3 years with cognitive changes through Pearson’s correlational analyses. The severity of akathisia showed a slight association with cognitive score changes in FAS (r = −0.25; p = 0.03), Iowa Gambling Task (IGT) (r = −0.25; p = 0.03), and Global Cognitive Score (r = 0.31; p = 0.02).
Relationship between cognitive change and concomitant medications
The feasible contribution of concomitant medications on cognitive changes in the three groups of treatments was also explored. A different proportion of patients in each treatment group received antimuscarinic medication at most time points. More specifically, olanzapine patients received antimuscarinics in a lesser proportion than the other two groups (see Table 2). A stratification based on antimuscarinic use at 3 months (the moment with the highest proportion of patients with antimuscarinics) was made, and then, change scores were compared with covariation of baseline performance; patients with antimuscarinic treatment (at 3 months) improved less on RAVLT (long-term recall) from baseline to 3 years (F = 6.55; p = 0.01) (see Table 4).
Finally, the cumulative rate of use of antidepressants, mood stabilizers, hypnotics, and benzodiazepines did not differ from one treatment group to another at 3 years. Similar rates of substance abuse, alcohol, tobacco, cannabis, cocaine, amphetamine, LSD, and other drugs were found in the three treatment groups (data are available upon request).
Discussion
In a 3-year follow-up treatments comparison of patients with FES, we found that (1) cognitive effectiveness between the three randomized antipsychotics was similar;(2) the better performance observed on RAVLT and Digit Symbol in olanzapine treatment group was likely explained by the lower prevalence of use of antimuscarinic drugs; (3) cognitive score improvements in patients were overall similar to those found in healthy volunteers (practice effect); and (4) changes in clinical symptoms and the emergence of motor side effects did not significantly mediate cognitive changes.
First- and second-generation antipsychotic long-term effects on cognitive performance
Consistent with earlier long-term investigations of patients with FES treated with low doses of haloperidol (Green et al. 2002; Davidson et al. 2009), our patients treated with haloperidol showed cognitive score improvements similar to those found in patients treated with risperidone or olanzapine. Similarly, haloperidol, olanzapine, and risperidone were found to be equally effective in treating cognitive deficits at medium term (1 year) (Crespo-Facorro et al. 2009). No differences in cognitive effectiveness between risperidone and olanzapine were found either by Cuesta and colleagues (2009) after 6 months of treatment. In contrast, the short-term analysis (12 weeks) from this sample had revealed a significant benefit of olanzapine compared to haloperidol (Keefe et al. 2004). Harvey and colleagues (2005) in a 12-week follow-up study also reported that risperidone was significantly more beneficial than haloperidol. A couple of additional short-term studies have also found a greater improvement of risperidone relative to haloperidol (Schuepbach et al. 2002; Lee et al. 2007). Purdon et al. described a significantly greater benefit in the general cognitive index (six cognitive domains) of olanzapine relative to haloperidol and risperidone at short term (Purdon et al. 2000b). Consistently, Keefe and colleagues observed that olanzapine produced significantly more cognitive benefits than haloperidol at short term (12 weeks), but they failed to demonstrate cognitive changes at 1 and 2 years (Keefe et al. 2004, 2006). Taken together, the results from aforementioned studies seem to indicate that the greater cognitive improvements associated to SGAs in short-term studies are no longer significant when lengthy periods of follow-up are considered.
High doses of haloperidol might mask practice effects, and therefore, the previously reported positive effects of SGAs may be due to too high doses of haloperidol in the control arms. Woodward et al. in a recent meta-analysis found no evidence that higher doses of haloperidol may perhaps be associated with lower cognitive score improvements (Woodward et al. 2005). However, the dose of haloperidol used in our study (3.64 mg) is relatively low compared to the range of doses used in previous investigations in FEP (Davidson et al. 2009). Thus, in agreement with Buchanan et al. recommendations (Buchanan et al. 2010), there is insufficient evidence to support a recommendation for the preferential use of SGAs over FGAs to achieve gains in the treatment of cognitive impairments.
Practice effects in the assessment of cognitive improvement
A secondary goal of this study was to investigate whether cognitive changes in the three groups of patients might be attributed to repeated exposure to cognitive tests. Most cognitive score changes in our treatment groups are similar to those found in healthy controls and, therefore, might be due to practice effects rather than true improvements in the compromised neurocognitive function. The weight of practice effects has been not widely examined in previous studies of first-episode schizophrenia, investigating the differential effects of antipsychotic medications on cognition. Goldberg and colleagues (2007) observed that cognitive score improvements found in first-episode patients treated with risperidone or olanzapine were consistent in magnitude with practice effects observed in healthy controls. Short-term clinical trials in which patients undergo cognitive assessments with short intervals are especially vulnerable to practice effect (McCaffrey and Westervelt 2000). Haloperidol may exert subtle negative effects on cognition that interfere with practice effects (Carpenter and Gold 2002). In a meta-analysis study conducted by Woodward et al. (2007), they concluded that haloperidol may contribute to circumscribed reductions in the practice effects observed in processing speed and working memory (verbal fluency) tests. It is likely that deleterious effects of haloperidol found in short-term studies might be mediated by the greater interference with practice effect when short intervals between assessments are established. In long-term studies in which the weight of multiple testing would be diminished, owing to the lengthy intervals between assessments, these detrimental effects of haloperidol would vanish. We have also explored the likelihood that the presence of a ceiling effect in the cognitive performance of the control group would produce type II error inflation. Consistently, the analysis of effect size (ES) of differences between baseline and 3 years showed that ES in the control group are in a similar range than patients (see Table 2).
Cognitive impairment and concomitant factors
It is of note that a stratification based on antimuscarinics used in our sample revealed that those patients receiving antimuscarinics at 3 years showed lower cognitive score changes in memory tests than patients who had not taken them. Thus, we suggest that the antimuscarinic medications may differentially interfere with memory in longitudinal studies depending on the weight of practice effects on cognitive test performance. Human and animal studies have consistently shown that drugs with antimuscarinic characteristics impair learning and memory (Levin 1988). The greater frequency of emergent EPS, the higher use of antimuscarinics to treat EPS, and the marked D2 receptor blockade in the dorsal striatum may interfere with procedural learning and memory (Kumari et al. 1997; Ramaekers et al. 1999; Kapur et al. 2000). Relatively higher doses of haloperidol at the first break of the illness may bias the results of short-term cognitive studies towards revealing deleterious cognitive effects owing to the higher prevalence of EPS and the consequent greater use of antimuscarinic medications. McGurk and colleagues (2004) described that the relative benefits of risperidone on spatial working memory performance at short term were related to the higher use of antimuscarinics in haloperidol-treated patients. Harvey et al. (2005) also described significantly greater EPS and use of adjunctive medication in the haloperidol group compared to the risperidone-treated patients. Similarly, Purdon et al. (2000a, b) had also described that a significantly greater proportion of patients on haloperidol (73.3 %) and risperidone (45 %) required antimuscarinic treatment relative to olanzapine (15 %).
Limitations
This study has several limitations. First, it is important to keep in mind that the lack of a group of drug-free patients in which practice effects would have been assessed limits our capacity to fully ascertain to what extent cognitive score changes are related to practice effects, medication effects, or illness itself. Hence, our results herein should be considered as inferential. Second, the fact that our study was the open-label design, as this would have led to some data bias and potentially to some bias in the interpretation of the results. Third, the small number of patients in each group who completed the 3-year evaluation may increase the risk of making type II errors. This caveat seems to be even more relevant in the per protocol analysis. Despite these limitations, to the best of our knowledge, this is the first controlled clinical trial that compares long-term (3-year follow-up) cognitive effectiveness of SGAs (olanzapine and risperidone) and FGAs (low-dose haloperidol) in which a group of healthy subjects has also been repeatedly assessed to examine the potential effects of practice.
Conclusions
Haloperidol, olanzapine, and risperidone have not demonstrated substantial neurocognitive effectiveness in improving the cognitive deficits present in the early phases of the illness. The use of antimuscarinic drugs may interfere with specific cognitive functions. Our results clearly underscore the importance of exploring the cognitive efficacy of new antipsychotic drugs, while playing a crucial role in rehabilitation, psychotherapeutic, and psychosocial interventions, for the treatment of cognitive impairments in long-term schizophrenia patients.
References
Addington D, Addington J, Maticka-Tyndale E (1994) Specificity of the Calgary Depression Scale for schizophrenics. Schizophr Res 11(3):239–244
Andreasen NC (1983) Scale for the assessment of negative symptoms (SANS). University of Iowa, Iowa City
Andreasen NC (1984) Scale for the assessment of positive symptoms (SAPS). University of Iowa, Iowa City
Andreasen NC, Flaum M, Arndt S (1992) The Comprehensive Assessment of Symptoms and History (CASH). An instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry 49(8):615–623
Andreasen NC, Pressler M, Nopoulos P, Miller D, Ho BC (2010) Antipsychotic dose equivalents and dose-years: a standardized method for comparing exposure to different drugs. Biol Psychiatry 67(3):255–262
Barnes TR (1989) A rating scale for drug-induced akathisia. Br J Psychiatry 154:672–676
Bozikas VP, Andreou C (2011) Longitudinal studies of cognition in first episode psychosis: a systematic review of the literature. Aust N Z J Psychiatry 45(2):93–108
Buchanan RW, Kreyenbuhl J, Kelly DL, Noel JM, Boggs DL, Fischer BA, Himelhoch S, Fang B, Peterson E, Aquino PR, Keller W (2010) The 2009 schizophrenia PORT psychopharmacological treatment recommendations and summary statements. Schizophr Bull 36(1):71–93
Carpenter WT, Gold JM (2002) Another view of therapy for cognition in schizophrenia. Biol Psychiatry 51(12):969–971
Crespo-Facorro B, Rodriguez-Sanchez JM, Perez-Iglesias R, Mata I, Ayesa R, Ramirez-Bonilla M, Martinez-Garcia O, Vazquez-Barquero JL (2009) Neurocognitive effectiveness of haloperidol, risperidone, and olanzapine in first-episode psychosis: a randomized, controlled 1-year follow-up comparison. J Clin Psychiatry 70(5):717–729
Cuesta MJ, Jalon EG, Campos MS, Peralta V (2009) Cognitive effectiveness of olanzapine and risperidone in first-episode psychosis. Br J Psychiatry 194(5):439–445
Davidson M, Galderisi S, Weiser M, Werbeloff N, Fleischhacker WW, Keefe RS, Boter H, Keet IP, Prelipceanu D, Rybakowski JK, Libiger J, Hummer M, Dollfus S, Lopez-Ibor JJ, Hranov LG, Gaebel W, Peuskens J, Lindefors N, Riecher-Rossler A, Kahn RS (2009) Cognitive effects of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: a randomized, open-label clinical trial (EUFEST). Am J Psychiatry 166(6):675–682
First MB, Spitzer, Robert L, Gibbon Miriam, and Williams, Janet BW (1996) Structured Clinical Interview for DSM-IV Axis I Disorders. Washington, D.C.
Goldberg TE, Goldman RS, Burdick KE, Malhotra AK, Lencz T, Patel RC, Woerner MG, Schooler NR, Kane JM, Robinson DG (2007) Cognitive improvement after treatment with second-generation antipsychotic medications in first-episode schizophrenia: is it a practice effect? Arch Gen Psychiatry 64(10):1115–1122
Gonzalez-Blanch C, Crespo-Facorro B, Alvarez-Jimenez M, Rodriguez-Sanchez JM, Pelayo-Teran JM, Perez-Iglesias R, Vazquez-Barquero JL (2007) Cognitive dimensions in first-episode schizophrenia spectrum disorders. J Psychiatr Res 41(11):968–977
Green MF (1996) What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry 153(3):321–330
Green MF, Marder SR, Glynn SM, McGurk SR, Wirshing WC, Wirshing DA, Liberman RP, Mintz J (2002) The neurocognitive effects of low-dose haloperidol: a two-year comparison with risperidone. Biol Psychiatry 51(12):972–978
Harvey PD, Rabinowitz J, Eerdekens M, Davidson M (2005) Treatment of cognitive impairment in early psychosis: a comparison of risperidone and haloperidol in a large long-term trial. Am J Psychiatry 162(10):1888–1895
Hoff AL, Svetina C, Shields G, Stewart J, DeLisi LE (2005) Ten year longitudinal study of neuropsychological functioning subsequent to a first episode of schizophrenia. Schizophr Res 78(1):27–34
Kapur S, Zipursky R, Jones C, Remington G, Houle S (2000) Relationship between dopamine D(2) occupancy, clinical response, and side effects: a double-blind PET study of first-episode schizophrenia. Am J Psychiatry 157(4):514–520
Keefe RS, Silva SG, Perkins DO, Lieberman JA (1999) The effects of atypical antipsychotic drugs on neurocognitive impairment in schizophrenia: a review and meta-analysis. Schizophr Bull 25(2):201–222
Keefe RS, Seidman LJ, Christensen BK, Hamer RM, Sharma T, Sitskoorn MM, Lewine RR, Yurgelun-Todd DA, Gur RC, Tohen M, Tollefson GD, Sanger TM, Lieberman JA (2004) Comparative effect of atypical and conventional antipsychotic drugs on neurocognition in first-episode psychosis: a randomized, double-blind trial of olanzapine versus low doses of haloperidol. Am J Psychiatry 161(6):985–995
Keefe RS, Seidman LJ, Christensen BK, Hamer RM, Sharma T, Sitskoorn MM, Rock SL, Woolson S, Tohen M, Tollefson GD, Sanger TM, Lieberman JA (2006) Long-term neurocognitive effects of olanzapine or low-dose haloperidol in first-episode psychosis. Biol Psychiatry 59(2):97–105
Kumari V, Corr PJ, Mulligan OF, Cotter PA, Checkley SA, Gray JA (1997) Effects of acute administration of d-amphetamine and haloperidol on procedural learning in man. Psychopharmacology (Berl) 129(3):271–276
Lee SM, Chou YH, Li MH, Wan FJ, Yen MH (2007) Effects of antipsychotics on cognitive performance in drug-naive schizophrenic patients. Prog Neuropsychopharmacol Biol Psychiatry 31(5):1101–1107
Levin ED (1988) Psychopharmacological effects in the radial-arm maze. Neurosci Biobehav Rev 12(2):169–175
McCaffrey RJ, D K, Westervelt HJ 2000. Practitioner’s Guide to evaluating change with neuropsychological assessment instruments. New York.
McGurk SR, Green MF, Wirshing WC, Wirshing DA, Marder SR, Mintz J, Kern R (2004) Antipsychotic and anticholinergic effects on two types of spatial memory in schizophrenia. Schizophr Res 68(2–3):225–233
Pelayo-Teran JM, Perez-Iglesias R, Ramirez-Bonilla M, Gonzalez-Blanch C, Martinez-Garcia O, Pardo-Garcia G, Rodriguez-Sanchez JM, Roiz-Santianez R, Tordesillas-Gutierrez D, Mata I, Vazquez-Barquero JL, Crespo-Facorro B (2008) Epidemiological factors associated with treated incidence of first-episode non-affective psychosis in Cantabria: insights from the Clinical Programme on Early Phases of Psychosis. Early Interv Psychiatry 2(3):178–87
Purdon SE, Jones BD, Stip E, Labelle A, Addington D, David SR, Breier A, Tollefson GD (2000a) Neuropsychological change in early phase schizophrenia during 12 months of treatment with olanzapine, risperidone, or haloperidol. The Canadian Collaborative Group for research in schizophrenia. Archives of general psychiatry 57(3):249–258
Purdon SE, Jones BD, Stip E, Labelle A, Addington D, David SR, Breier A, Tollefson GD (2000b) Neuropsychological change in early phase schizophrenia during 12 months of treatment with olanzapine, risperidone, or haloperidol. The Canadian Collaborative Group for research in schizophrenia. Arch Gen Psychiatry 57(3):249–258
Ramaekers JG, Louwerens JW, Muntjewerff ND, Milius H, de Bie A, Rosenzweig P, Patat A, O'Hanlon JF (1999) Psychomotor, Cognitive, extrapyramidal, and affective functions of healthy volunteers during treatment with an atypical (amisulpride) and a classic (haloperidol) antipsychotic. J Clin Psychopharmacol 19(3):209–221
Reichenberg, A, Harvey, P D, Bowie, C R, Mojtabai, R, Rabinowitz, J, Heaton, R K, Bromet, E (2008) Neuropsychological function and dysfunction in schizophrenia and psychotic affective disorders. Schizophr Bull
Schuepbach D, Keshavan MS, Kmiec JA, Sweeney JA (2002) Negative symptom resolution and improvements in specific cognitive deficits after acute treatment in first-episode schizophrenia. Schizophr Res 53(3):249–261
Simpson GM, Angus JW (1970) A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl 212:11–19
Velligan DI, Weiden PJ, Sajatovic M, Scott J, Carpenter D, Ross R, Docherty JP (2010) Assessment of adherence problems in patients with serious and persistent mental illness: recommendations from the Expert Consensus Guidelines. J Psychiatr Pract 16(1):34–45
Woodward ND, Purdon SE, Meltzer HY, Zald DH (2005) A meta-analysis of neuropsychological change to clozapine, olanzapine, quetiapine, and risperidone in schizophrenia. Int J Neuropsychopharmacol 8(3):457–472
Woodward ND, Purdon SE, Meltzer HY, Zald DH (2007) A meta-analysis of cognitive change with haloperidol in clinical trials of atypical antipsychotics: dose effects and comparison to practice effects. Schizophr Res 89(1–3):211–224
Acknowledgments
The present study was performed at the Hospital Marqués de Valdecilla, University of Cantabria, Santander, Spain, under the following grant support: Instituto de Salud Carlos III PI020499, PI050427; Plan Nacional de Drogas Research Grant 2005, Orden sco/3246/2004; SENY Fundació Research Grant CI 2005-0308007; and Fundación Marqués de Valdecilla API07/011. No pharmaceutical company supplied any financial support towards it. The study, designed and directed by B C-F and JL V-B, conformed to international standards for research ethics and was approved by the local institutional review board. We wish to thank the PAFIP researchers who helped with data collection and specially acknowledge César González-Blanch and Mrs. Gema Pardo for data collection and their research assistance. In addition, we acknowledge the participants and their families for enrolling in this study.
Conflict of Interest
Prof. Vazquez-Barquero and Prof. Crespo-Facorro have received unrestricted research funding from AstraZeneca, Pfizer, Bristol-Myers Squibb, and Johnson & Johnson that were deposited into research accounts at the University of Cantabria. Prof. Vazquez-Barquero has received honoraria for his participation as a speaker at educational events from Johnson & Johnson. Prof. Crespo-Facorro has received honoraria for his participation as a speaker at educational events from Pfizer, Bristol-Myers Squibb, and Johnson & Johnson and consultant fees from Pfizer. Prof. Tabarés-Seisdedos has received grants from or acted as a consultant for the following companies: AstraZeneca, Janssen, Eli Lilly, Lundbeck, Novartis, Pfizer, Sanofi-Aventis, and Wyeth that were deposited into research accounts at the University of Valencia. The remaining authors report no competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ayesa-Arriola, R., Rodríguez-Sánchez, J.M., Pérez-Iglesias, R. et al. Long-term (3-year) neurocognitive effectiveness of antipsychotic medications in first-episode non-affective psychosis: a randomized comparison of haloperidol, olanzapine, and risperidone. Psychopharmacology 227, 615–625 (2013). https://doi.org/10.1007/s00213-013-2994-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-013-2994-z