Abstract
Summary
We determined if nurses can manage osteoporotic fractures in a fracture liaison service by asking a rheumatologist and an internist to assess their clinical decisions. Experts agreed on more than 94 % of all nurses’ actions for 525 fragility fracture patients, showing that their management is efficient and safe.
Introduction
A major care gap exists in the investigation of bone fragility and initiation of treatment for individuals who have sustained a fragility fracture. The implementation of a fracture liaison service (FLS) managed by nurses could be the key in resolving this problem. The aim of this project was to obtain agreement between physicians’ and nurses’ clinical decisions and evaluate if the algorithm of care is efficient and reliable for the management of a FLS.
Methods
Clinical decisions of nurses for 525 subjects in a fracture liaison service between 2010 and 2013 were assessed by two independent physicians with expertise in osteoporosis treatment.
Results
Nurses succeeded in identifying all patients at risk and needed to refer 27 % of patients to an MD. Thereby, they managed autonomously 73 % of fragility fracture patients. No needless referrals were made according to assessing physicians. Agreement between each evaluator and nurses was of >97 %. Physicians’ decisions were the same in >96 %, and Gwet AC11 coefficient was of >0.960 (almost perfect level of agreement). All major comorbidities were adequately managed.
Conclusions
High agreement between nurses’ and physicians’ clinical decisions indicate that the independent management by nurses of a fracture liaison service is safe and should strongly be recommended in the care of patients with a fragility fracture. This kind of intervention could help resolve the existing care gap in bone fragility care as well as the societal economic burden associated with prevention and treatment of fragility fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a chronic disease with fractures as its main outcome. It has been widely documented that this condition is treatable and the fractures preventable [1, 2]. Nevertheless, approximately 30 % of women will be diagnosed with osteoporosis and about half of this proportion will receive treatment following a fragility fracture [3, 4]. Moreover, costs associated with the treatment of fragility fractures are high worldwide, ranging from $2.3 billion in Canada (2008), $15 to 20 billion in the USA, and $37 billion in the European Union (2010) annually [5–7]. Ageing of the population can only exacerbate the problem [8].
A lot of effort has been put into the development of management models for the prevention of subsequent fractures [9, 10]. A high intensity of intervention model of care, such as a fracture liaison service (FLS), has proven to be one of the best approaches in reducing the care gap in osteoporosis [11]. A FLS is characterized by three main interventions (3i): identification of patients at risk for fracture, investigation for bone fragility, and initiation of treatment for subsequent fracture prevention [12, 13]. Our FLS consists in a 4i management, the fourth “i” being integration of follow-up. Indeed, after the initiation of treatment, a thorough follow-up of patients was undertaken to ensure persistence, compliance, safety, and prevention of subsequent fractures. A nurse case manager (NCM) is the dedicated health care professional usually designated to manage a FLS in collaboration with orthopedic surgeons or other specialists [14, 15]. Still, the need to assess the management of a FLS by nurses remains.
The main goal of the present project was to develop and implement an algorithm based on the clinical guidelines of Osteoporosis Canada that could be applied independently by nurses through an order set. Therefore, the objective of this study was to determine if nurses can carry out the role of a NCM in a FLS while ensuring safety of the clinical decisions regarding identification of patients at risk, investigation for bone fragility, initiation of treatment, referral to a specialist when needed, and follow-up.
Methodology
Study design
We conducted a cross-sectional study as part of a larger prospective cohort study that aimed to determine the incidence of subsequent fractures following initiation of a FLS. Between 2010 and 2013, men and women were identified by NCMs at the outpatient orthopedic clinic of Hôpital du Sacré-Coeur de Montréal and Hôpital Jean-Talon. NCMs looked through medical files to identify patients (1) aged 40 years and older and (2) with a fracture sustained following a low-energy trauma such as a fall from standing height, from a chair, a bed, and even from a severe cough or a sneeze [16]. Only patients from the outpatient orthopedic clinic were identified and recruited. Exclusion criteria include (1) patients less than 40 years old, (2) with an open fracture, (3) a fracture from a high energy trauma, (4) a fracture of the skull/face/little bones under the wrist or ankle, (5) a pathological fracture, (6) severe kidney failure, (7) pregnant or breastfeeding, (8) with dementia, or (9) unable to fill a questionnaire in English or French.
Informed consent was obtained from all participants included in the study. This study was approved by the Hôpital Sacré-Coeur de Montréal and Centre Hospitalier de l’Université de Montréal ethic research committees.
Data collection
Patients enrolled in the FLS are followed over a 10-year period with systematic follow-ups (3, 6, 12, 18, 24 months, and each year). During the baseline evaluation, the NCM collected the following information: age, sex, body mass index (BMI), fracture site, number of previous fractures, medications, medical history, and family history. Patients were provided with a requisition for serum (total blood count, creatinine, thyroid-stimulating hormone, parathyroid hormone, calcium, protein electrophoresis, C-reactive protein, alkaline phosphatase, 25-hydroxy vitamin D, osteocalcin, and C-telopeptide) and bone mineral density (BMD) testing. Patients were referred to a bone specialist at baseline for the following reasons: (1) patients that experienced treatment failure, defined as a fragility fracture sustained while taking an anti-resorptive agent for at least a year, (2) aged between 40 and 49 years, or (3) presenting a contraindication to treatment. The management algorithm of care followed by NCMs was based on Osteoporosis Canada guidelines for the prevention of fragility fractures. This algorithm is summarized in Fig. 1.
Fracture liaison service personnel
This program was managed by a clinical nurse specialist (CNS) with the help of two clinical nurses. A CNS with a graduate level of studies and extensive clinical experience was responsible for the clinical nurses’ training, guidance, and case discussion with physicians. The training of clinical nurses for the FLS included a 6-h theoretical presentation mainly on osteoporosis physiopathology, the management of fragility fractures, and pharmacological/non-pharmacological treatment for bone fragility. This was followed by a 2-month training period with the CNS.
Intervention
Two physicians, a rheumatologist and an internist, with expertise in osteoporosis management and clinical research (JPR and SNM) evaluated if nurses’ actions in terms of referral decision and treatment initiation were consistent with the algorithm of care for the 543 subjects (Fig. 2).
Data collected included age, sex, site of fracture, number of previous fractures, medical history, medication list, blood biochemistry test results, BMD T-scores, BMI, decision of referral, reason of referral, and initiation of treatment at baseline. Blood tests included serum bone turnover biomarkers (CTX-1 and osteocalcin), protein electrophoresis, creatinine, creatinine clearance, calcium, 25-hydroxy vitamin D, and parathyroid hormone (PTH). All cases were attributed with a number as their only mean of identification.
Statistical analysis
To ensure a precise and reliable raw agreement between the nurses and the evaluators, a sample size of subjects to be reviewed was calculated based on the purpose of the probability to obtain a statistically significant kappa coefficient. Because we assumed no bias between the two raters, the calculations based on the Donner and Eliasziw goodness-of-fit formula was used with a type I probability of error of 0.05, 90 % of power, an expected proportion of positive ratings of 0.9, a kappa to detect of 0.8, and a null value of 0.6 [17]. For a two-tailed test, we needed a sample size of 449 needed «observations» to agree on or not. Therefore, the whole study population (n = 543) yielded sufficient statistical power.
The primary outcome, the raw agreement between the nurses and each evaluator, was calculated as the proportion of nurses’ decisions agreed upon by the evaluators. The same was done for raw agreement between both evaluators (agreement and disagreement for the same cases). Pearson’s chi-squared test was used to determine if there was a significant association between the experts’ answers. A one-proportion z test with a 95 % confidence interval was used to observe the difference, if one present, between the obtained total agreement and the hypothesized one, which was of 90 %. No measure of reliability was calculated for the total agreement because it included two types of decisions per subject, leaving a contingency table as not feasible. We considered a p value of ≤0.05 as statistically significant.
Inter-rater reliability was calculated with Cohen’s kappa coefficient (κ) with 95 % confidence intervals. This statistic allows to measure raw agreement by adjusting for chance agreement [18]. The obtained coefficient varies between 1 and −1, where 1 is a perfect agreement, 0 indicates no agreement, and −1 means a perfect disagreement [19]. It was possible to use this reliability measure with the production of contingency tables since our variables are dichotomous nominal ones. However, it was necessary to use an alternative to this measure because of Feinstein and Cicchetti’s «paradox of kappa» (1990) [20]. It is a possible bias generated by the agreement distribution in the population, presenting as a low value of kappa when the agreement is high or the opposite. To address this problem, a «paradox resistant» option exists, Gwet’s AC1 coefficient [21]. Here are the formulas of both coefficients:
where p is the global proportion of agreement and e(K) and e(γ) represent the agreement probability attributed to chance [22, 23]. The AC1 coefficient also determines inter-rater reliability by adjusting agreement for chance but differs in agreement probability of chance calculation. Instead of estimating the probability that an answer is attributed to chance, the AC1 coefficient estimates the probability of an observer to agree even if the answer is random. Interpretation of kappa and AC1 coefficients is based on the Landis and Koch scale (1977) [19].
Results
Population characteristics
A total of 525 subjects’ data was reviewed by the two physicians. Studied population characteristics according to sex are shown in Table 1. A significant number of patients had a diagnosis of osteoporosis, digestive disorders, hypercholesterolemia, and hypertension. Main fracture sites included the wrist, ankle, and humerus. Thirty-two percent of patients had sustained a fragility fracture prior to the index fracture. Overall, nurses referred almost 27 % of patients to a specialist mainly for treatment failure and for age 49 years or less, as pre-specified.
Agreement
Table 2 shows raw agreement between nurses and physicians as well as the raw agreement between both physicians. Inter-rater reliability is also presented in this table. More than 97 % of referral and initiation of treatment decisions by the nurses were agreed on by either evaluator. Overall, near 95 % of all nurses’ decisions were agreed on by both evaluators («yes-yes» answers) (95 % CI [0.925 à 0.964]). There was a significant positive association between answers of the two physicians for the types of decision (p < 0.05). Both evaluators disagreed on the nurses’ clinical decisions in 5/525 cases (<1 %). Twenty two out of 525 clinical decisions were disagreed on by one of the two evaluators, mainly for non-referral of some patients (under 65 years of age with a major fracture, on hormonal therapy, low BMD in young patients) or that were recruited for a stress fracture of the foot.
Our kappa values for inter-rater variability were very low (<0.370). The paradox of kappa was corrected by calculating Gwet’s AC1 coefficient where values are higher (>0.960). These results are consistent with an almost perfect level of agreement on the scale of Landis and Koch.
Management of major comorbidities and contraindications/intolerances
When looking at referred patients, three of them were referred for abnormal screening (high PTH level or a T-score lower than −5.0). Two patients were referred for very low levels of bone turnover biomarkers. Fourteen subjects were referred for contraindication to treatment or intolerance to medication. Other reasons of referral were major comorbidities.
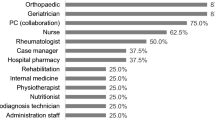
Regarding non-referred patients, some of them had a medical diagnosis that required particular attention even if a referral was not necessary (see Fig. 3). Patients with these medical conditions were not referred to a bone specialist for one of the following reasons: (1) They were followed by a specialist before joining the FLS, (2) were prescribed an alternate anti-resorptive agent when they were contraindicated (chronic renal failure or gastric problems), or (3) dropped out before a meeting with our specialist.
Discussion
The main objective of this study was to obtain agreement between physicians and nurses’ clinical decisions in a FLS. It was important to determine if nurses can identify a fragility fracture from a trauma fracture and inform patients about available care (first i), propose appropriate investigation in order to rule out causes of secondary osteoporosis (second i), initiate pharmacological treatment when appropriate (third i), and follow the patient (fourth i). If so, we also needed to determine whether a nurse can identify specific health conditions other than the bone fragility, which could require the intervention of a physician. It was the secondary objective of this study to assess the algorithm of care used in this program.
Our results show that the overall agreement between the nurses and both physicians was high (95 %) and significantly higher than hypothesized (90 %). Individually, the two types of clinical decisions (referral to specialist and initiation of treatment) were agreed on by each evaluator up to 97 % and more. The inter-rater reliability was also a lot higher than projected, reaching an almost perfect level of agreement according to the Landis and Koch scale [19]. Thus, the experts had a very similar management path and clinical decision process for patients with fragility fractures. When acknowledging that the physicians practice different specialities (rheumatology and internal medicine), the results confirm that the management of bone fragility is approximately the same between health professionals. These results suggest that nurses can efficiently manage a FLS. All patients with major comorbidities were adequately managed with a referral to a physician or by insuring that the patient is already followed by the appropriate health professional. Patients aged between 40 and 49 years were automatically referred to a physician because they met all the bone fragility criteria except for the cutoff age of intervention recommended by Osteoporosis Canada, which is 50 years or more. Patients with treatment failure had to be referred to a physician since alternative treatments are exceptional medications for which nurses would not have the authorization to prescribe in an order set.
Since less than 1 % of decisions were not agreed upon by both evaluators, the management algorithm was found to be usable in an FLS managed by nurses. These guidelines include not only the 3i of an FLS (identification, investigation, initiation of treatment) but also the fourth i: integration.
A high-intensity intervention model is required for the prevention of fragility fractures according to study results throughout scientific literature [11, 15]. A high-intensity model of care matches the definition of a fracture liaison service but omits the monitoring of results and follow-up of patients (fourth i) [12, 13, 24]. Many studies have demonstrated the effectiveness of such a service with a NCM as its main contributor [14, 15]. All studies with the aim to determine efficacy of a FLS listed the interventions done and measured clinical outcomes as results. All assumed that the NCM was a professional with the appropriate skills and qualifications to handle the management of fragility fracture patients. None assessed the safety and efficacy nor described the necessary training for such a professional. Furthermore, several studies used a registered nurse as the NCM [25–28], while the other half used a specialized nurse [14, 15, 29]. Thus, there was a need to define which professional should be attributed the NCM role for a proper and secure intervention.
The difference between registered and specialized nurses resides in the level of scholar graduation and the number of years of clinical experience. Depending on the country’s policies and states/provinces’ regulations, several nursing diplomas or roles exist [30]. In general, a registered nurse has a college degree and a specialized nurse has an advanced studies degree with a lot of expertise. The best-known roles of specialized nurses are the nurse practitioner (NP) and the CNS. They ensure that there is improvement in the management of patients, that nurses’ work is optimized, and to the development of functional, reliable, and effective systems [31, 32]. Moreover, an expert panel determined in 2011 the most efficient preventive approach in the management of osteoporosis. They indicated that a NCM should be the designated professional for the management of a fragility fracture system [33]. A literature review and meta-analysis gathering the results of physician substitution studies showed that a high level of skills leads to a better management [34].
In the FLS studied, a CNS works in collaboration with two clinical nurses, which ensure the first-line intervention with patients. A pattern of hierarchy was observed; the CNS stood out with her leadership and management of other nurses’ abilities. As clinical nurses would ensure the recruitment of patients, data collection, the scheduling of appointments, the requests for laboratory and radiology tests, referrals to a physician, and follow-ups with patients, the CNS would guide the nurses with their clinical decisions and help in recognizing major comorbidities to be taken care of.
This study’s main strength lies in the high number of cases or “observations” reviewed by our experts. Also, we were able to have the participation from two physicians with different specialities, which was an advantage in demonstrating the homogeneity of interventions to treat fragility fractures within health professionals. A possibility of bias exists because of the physician evaluator no. 1 who was the referral specialist consulted by six patients included in the study. However, all patients included for the evaluation by experts were attributed a number for identification in order to preserve confidentiality. This reduces the possibility of the evaluator no. 1 recognizing one of the six patients. It would also have been an option to exclude these patients of the study, this without affecting its power. Moreover, this evaluator has reviewed the guidelines used by nurses in this FLS. However, he was not part of the group of experts who created the algorithm of care. This study could not help determine if subsequent fractures could be prevented by the early intervention of nurses in a 4iFLS. Losses to follow-up and compliance to treatment are issues that could not be assessed in the present project. Longitudinal analyses are yet to come.
This study shows that nurses can efficiently and safely manage patients with fragility fractures. The implementation of FLSs (4i), such as the Lucky Bone™ program, with nurses as case managers with the help of a specialized nurse for management is feasible and could have a major impact on health care accessibility. This approach could greatly contribute on closing the care gap of the underlying osteoporosis in patients that sustained a fragility fracture.
References
North American Menopause Society (2010) Position statement: management of osteoporosis in postmenopausal woman: 2010. Menopause 17:25–54. doi:10.1097/gme.0b013e3181c617e, quiz 55–6
Kanis JA, McCloskey EV, Johansson H, Cooper C, Rizzoli R, Reginster JY et al (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 24(1):23–57. doi:10.1007/s00198-012-2074-y
Bessette L, Ste-Marie LG, Jean S, Davison KS, Beaulieu M, Baranci M et al (2008) The care gap in diagnosis and treatment of women with a fragility fracture. Osteoporos Int 19(1):79–86
Giangregorio L, Papaioannou A, Cranney A, Zytaruk N, Adachi JD (2006) Fragility fractures and the osteoporosis care gap: an international phenomenon. Semin Arthritis Rheum 35(5):293–305
Tarride JE, Hopkins RB, Leslie WD, Morin S, Adachi JD, Papaoiannou A et al (2012) The burden of illness of osteoporosis in Canada. Osteoporos Int 23(11):2591–2600. doi:10.1007/s00198-012-1931-z
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475
Hernlund E, Svedbom A, Ivergård M, Compston J, Cooper C, Stenmark J et al (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8(1–2):136. doi:10.1007/s11657-013-0136-1
United Nations, Department of Economic and Social Affairs, Population Division (2013) World population ageing 2013. ST/ESA/SER.A/348.
Sale JE, Beaton D, Posen J, Elliot-Gibson V, Bogoch E (2011) Systematic review on interventions to improve osteoporosis investigation and treatment in fragility fracture patients. Osteoporos Int 22(7):2067–2082. doi:10.1007/s00198-011-1544-y
Skorupski N, Alexander IM (2013) Multidisciplinary osteoporosis management of post low-energy trauma hip-fracture patients. J Am Assoc Nurse Pract 25(1):3–10. doi:10.1111/1745-7599.12002
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR et al (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24(2):393–406. doi:10.1007/s00198-012-2090-y
British Orthopaedic Association (2007) The care of patients with fragility fracture. Chandlers Printers Ltd. East Sussex, England. http://www.bgs.org.uk/index.php?option=com_content&view=article&id=338:bluebookfragilityfracture&catid=47:fallsandbones&Itemid=307. Accessed 22 June 2014
Osteoporosis Canada (2013) Make the first break the last with fracture liaison service. Toronto.http://www.osteoporosis.ca/fracture-liaison%20service/?utm_source=Home+Page&utm_medium=Menu+Button&utm_campaign=FLS. Accessed 3 June 2014
Gardner MJ, Brophy RH, Demetrakopoulos D, Koob J, Hong R, Rana A et al (2005) Interventions to improve osteoporosis treatment following hip fracture. A prospective, randomized trial. J Bone Joint Surg Am 87(1):3–7
El Miedany Y, Gardiner A, El Gaafary M, Toth M (2006) Outcomes of a nurse-led osteoporosis and falls assessment. Br J Nurs 15(19):1070–1076
Brown JP, Josse RG (2002) 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ 167(10 Suppl):S1–S34
Donner A, Eliasziw M (1992) A goodness-of-fit approach to inference procedures for the kappa statistic: confidence interval construction, significance-testing and sample size estimation. Stat Med 11(11):1511–1519
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46
Landis JR, Koch GG (1977) Measurement of observer agreement for categorical. Biometrics 33:159–174
Cicchetti DV, Feinstein AR (1990) High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol 43(6):551–558
Gwet KL (2008) Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol 61(Pt 1):29–48. doi:10.1348/000711006X126600
Wongpakaran N, Wongpakaran T, Wedding D, Gwet KL (2013) A comparison of Cohen’s Kappa and Gwet’s AC1 when calculating inter-rater reliability coefficients: a study conducted with personality disorder samples. BMC Med Res Methodol 13:61. doi:10.1186/1471-2288-13-61
Gwet KL (2012) Handbook of inter-rater reliability: the definitive guide to measuring the extent of agreement among multiple raters. Advanced Analytics Press, Gaithersburg
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD et al (2013) Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int 24:2135–2152. doi:10.1007/s00198-013-2348-z
Giles M, Van Der Kallen J, Parker V, Cooper K, Gill K, Ross L et al (2011) A team approach: implementing a model of care for preventing osteoporosis related fractures. Osteoporos Int 22(8):2321–2328. doi:10.1007/s00198-010-1466-0
Majumdar SR, Beaupre LA, Harley CH, Hanley DA, Lier DA, Juby AG et al (2007) Use of a case manager to improve osteoporosis treatment after hip fracture: results of a randomized controlled trial. Arch Intern Med 167(19):2110–2115
Harrington JT, Lease J (2007) Osteoporosis disease management for fragility fracture patients: new understandings based on three years’ experience with an osteoporosis care service. Arthritis Rheum 57(8):1502–1506
Inderjeeth CA, Glennon DA, Poland KE, Ingram KV, Prince RL, Van VR et al (2010) A multimodal intervention to improve fragility fracture management in patients presenting to emergency departments. Med J Aust 193(3):149–153
Huntjens KM, van Geel TC, Geusens PP, Winkens B, Willems P, van den Bergh J et al (2011) Impact of guideline implementation by a fracture nurse on subsequent fractures and mortality in patients presenting with non-vertebral fractures. Injury 42(Suppl 4):S39–S43. doi:10.1016/S0020-1383(11)70011-0
Bryant-Lukosius D, Carter N, Kilpatrick K, Martin-Misener R, Donald F, Kaasalainen S et al (2010) The clinical nurse specialist role in Canada. Nurs Leadersh (Tor Ont) 23(Spec No 2010):140–166
American association of colleges of nursing (2008) Consensus model for APRN regulation: licensure, accreditation, certification and education. APRN Joint Dialogue Group Report. Washington (DC). http://www.aacn.nche.edu/education-resources/APRNReport.pdf. Accessed 31 May 2014
Canadian nurses association (2008) Advanced nursing practice, a national framework. Ottawa (ON). http://cna-aiic.ca/~/media/cna/page-content/pdf-en/anp_national_framework_e.pdf. Accessed 15 May 2014
Adler RA, Bates DW, Dell RM, LeBoff MS, Majumdar SR, Saag KG et al (2011) Systems-based approaches to osteoporosis and fracture care: policy and research recommendations from the workgroups. Osteoporos Int 22(Suppl 3):495–500. doi:10.1007/s00198-011-1708-9
Martínez-González NA, Djalali S, Tandjung R, Huber-Geismann F, Markun S, Wensing M et al (2014) Substitution of physicians by nurses in primary care: a systematic review and meta-analysis. BMC Health Serv Res 14:214. doi:10.1186/1472-6963-14-214
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and animal rights and informed consent
All procedures performed in this study involving human participants were in accordance with the ethical standards of the Hôpital Sacré-Coeur de Montréal and Centre Hospitalier de l’Université de Montréal ethic research committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflicts of interest
Ms. Andréa Senay, Ms. Josée Delisle, and Dr. Julio C Fernandes report grants from Eli Lilly, educational grants from Sanofi Aventis, Novartis, and Amgen Canada during the conduct of this study. Ms. Josée Delisle also reports support for personal fees from Amgen Canada and Eli Lilly outside of the conducted work. Dr. Jean-Pierre Raynauld reports fees as an advisory board member for Amgen Canada outside of the conducted work. Dr. Suzanne Morin reports grants from Amgen Canada and Merck, support as an advisory board member from Amgen Canada and Eli Lilly outside of the conducted work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Senay, A., Delisle, J., Raynauld, J.P. et al. Agreement between physicians’ and nurses’ clinical decisions for the management of the fracture liaison service (4iFLS): the Lucky Bone™ program. Osteoporos Int 27, 1569–1576 (2016). https://doi.org/10.1007/s00198-015-3413-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3413-6