Abstract
Hip fracture is one of the most common orthopedic conditions and is associated with significant morbidity and mortality. With a progressively aging population, the annual incidence of hip fracture is expected to increase substantially. Emerging evidence suggests that early surgery (<24 h) minimizes complications secondary to immobilization, including orthostatic pneumonia and venous thromboembolism. Delayed surgical repair (>48 h) has been consistently demonstrated to be associated with an increased risk of 30-day and 1-year mortality. Nonetheless, early surgery necessitates a shorter time for preoperative medical preparation, in particular cardiac assessment. Patients who undergo emergent orthopedic surgery are therefore at greater risk of perioperative cardiac events than those who undergo elective surgery. In addition, the prompt triage system for preoperative cardiac assessment not only identifies patients at high risk of perioperative cardiac complications but also reduces unnecessary cardiac consultations for low-risk patients. We review the current recommendations for preoperative cardiac assessment adapted for patients with hip fracture and describe our current triage system for preoperative cardiac consultation.
Similar content being viewed by others
Introduction
Hip fracture is one of the most common orthopedic conditions that requires hospital admission and is associated with significant morbidity and mortality. The annual incidence of hip fracture was estimated to be 1.66 million worldwide in 1990 and is expected to reach 6.26 million by 2050 due to the aging population [1]. The majority of hip fractures occur in geriatric patients: approximately 80% of women and 50% of men with hip fractures are aged ≥70 years [2]. More importantly, up to one third of patients will die within 1 year of sustaining a hip fracture repair [3–6], and half will have permanent loss of function [7]. Early surgery (<24 h) can minimize complications secondary to immobilization including orthostatic pneumonia and venous thromboembolism and is expected to be beneficial for the majority of patients with a fractured hip. Delayed surgery (>48 h) has been consistently demonstrated by several studies to be associated with an increased risk of 30-day and 1-year mortality [8]. It is thus generally recommended that patients with hip fracture should undergo surgery as soon as possible (within 24 h of admission), during standard daytime working hours, including weekends, and provided they are medically fit [9].
Minimizing the time between admission and surgery nonetheless allows less time to evaluate and optimize patient’s underlying medical conditions. While this is not a concern for young individuals with no underlying medical problems, most patients with a hip fracture are frail and elderly with multiple pre-existing medical conditions that warrant comprehensive preoperative evaluation by physicians and/or cardiologists [10]. The goals of preoperative assessment should be (1) to identify patients at high risk of perioperative cardiac events and (2) to reduce their risks of complications and mortality. The American College of Cardiology (ACC) and the American Heart Association (AHA) guidelines for perioperative cardiovascular evaluation for non-cardiac surgery published in 2007 are invaluable protocols for cardiologists; nonetheless, it does not alert primary clinicians as to when a cardiac consultation is required. As a result, orthopedic surgeons, often the key member of the team, may face a clinical dilemma: to injudiciously consult a cardiologist for all elderly patients with a hip fracture, to proceed to timely surgery without a comprehensive preoperative cardiac assessment, or to delay surgery until a cardiac evaluation is complete. Based on the published international guidelines, we present a clinical protocol for preoperative cardiac assessment tailored for the geriatric patient with hip fracture from an orthopedic surgeon’s perspective.
Surgical risk of hip fracture repair
The nature of the surgery, including urgency, magnitude, type, and duration of the operation, is an important determinant in perioperative cardiac complications as well as in mortality. In general, the estimated cardiac risk of major orthopedic surgeries including hip and spine surgery is intermediate, i.e., estimated 30-day cardiac event rate (cardiac death and myocardial infarction) of 1–5% [11]. This stratification is based on the premise that most orthopedic procedures are electively performed in relatively young, healthy patients. In a stark contrast, elderly patients with a hip fracture who undergo surgical repair often have known predictors of cardiac disease, and the procedure performed is semi-urgent, not elective (<24 h). The risk profile thus differs. In a retrospective study of 8,930 patients aged ≥60 years who underwent hip fracture repair [12], 30-day and 1-year mortality was 4% and 16%, respectively. Of the,720 patients (8%) with postoperative cardiac complications, 178 patients (2%) were considered to have serious postoperative cardiac complications.
Stepwise approach to preoperative cardiac assessment
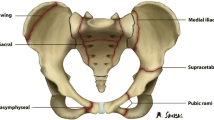
In 2007, the ACC and the AHA published a stepwise approach to preoperative cardiac assessment for patients undergoing non-cardiac surgery [11]. The guidelines consist of five decision-making steps that take into account urgency and risk of the surgery, presence of an active cardiac condition, functional capacity of the patient, and the associated cardiovascular risk factors. This helps determine whether to proceed with the planned surgery [11]. As mentioned, hip fracture repair can be considered a non-emergency (but semi-urgent) surgery with a moderate cardiac risk (~5% perioperative cardiac events and mortality); the original five-step approach could then be adapted to a three-step algorithm for this clinical context. Figure 1 depicts the clinical pathway for preoperative cardiac assessment of patients with a hip fracture. In order to determine whether a patient is medically fit for the surgery, patients with a hip fracture should have complete history and physical examination; in addition, chest X-ray and standard 12-lead electrocardiography should be obtained.
Cardiac evaluation and care algorithm for semi-urgent hip repair (adapted from [13]for geriatric hip fracture repair)
-
Step 1
Does the patient have any active cardiac conditions? (modified from [11])
The ACC/AHA guidelines have identified four groups of active cardiac conditions that signify major perioperative risk for surgery and that warrant preoperative workup (Table 1). Patients with one or more of these active cardiac conditions require further diagnostic evaluation and, possibly, therapeutic intervention. Of note, patients with underlying coronary artery disease are at higher than average risk of perioperative cardiac events. According to the ACCC/AHA guidelines, a coronary artery disease patient is defined as one with a history of myocardial infarction, percutaneous coronary intervention, coronary artery bypass grafting, or coronary arterial luminal obstruction documented by coronary angiography [11]. A patient with stable coronary artery disease and a functional capacity of four metabolic equivalents (METs) or above (Table 2) is considered medically fit for hip fracture repair surgery although elective surgery should be delayed for at least 6 months in patients with recent acute myocardial infarction. In a case series of 11 patients (mean age 78.2 years, female 73%) with recent myocardial infarction (3 to 23 days) who underwent hip fracture repair, 1- and 6-month mortality was 45.4% and 63.5%, respectively; the impact of recent ACS on the risk of perioperative cardiovascular events nonetheless remains unknown.
Table 1 Active cardiac conditions (modified from [13]) Table 2 Evaluation of the degree of activity in daily life (modified from [13]) As with coronary artery disease, heart failure is commonly associated with hip fracture. It has recently been shown in a cohort of 5,613 persons from the Cardiovascular Health Study with average follow-up of 11.5 years that patients with heart failure have a much higher incidence of hip fracture compared with those without heart failure (14/1,000 vs. 6.8/1,000 person-years). More importantly, patients with both heart failure and hip fracture have a twofold increase in risk of death compared with those with heart failure alone [13]. Patients with heart failure who undergo non-cardiac surgery have a poorer outcome than those without heart failure [14]. It is thus essential to identify patients with heart failure and optimize their cardiac condition prior to surgery. In addition, the presence of significant valvular disease, in particular, severe aortic stenosis, confers a substantial risk of perioperative cardiac events in patients who undergo non-cardiac surgery [11, 15–17]. Aortic stenosis is relatively common in geriatric patients (>65 years) [18, 19] and is often associated with hip fracture. In a retrospective study that included 3,997 consecutive patients with a hip fracture, 272 (6.8%) were confirmed to have a previously undiagnosed aortic stenosis as a result of echocardiography to investigate a previously undiagnosed heart murmur [20]. While it is recommended that echocardiography should be performed as part of a preoperative assessment if aortic stenosis is suspected, to allow confirmation of diagnosis, risk stratification, and possible cardiac intervention [21], the clinical decision on whether to operate on such patients remains a challenge due to the scarcity of clinical outcome data. In a retrospective study by Adunsky and colleagues involving 56 patients with hip fracture and aortic stenosis (mean valve area 0.97 ± 0.64 cm2) who underwent surgical repair [22], in-hospital and 1-year mortality was 6.5% and 17.7%, respectively.
-
Step 2
Does a patient have a functional capacity greater than or equal to 4 METSs without symptoms? (modified from [11])
Table 2 summarizes the estimated energy requirement for various common daily activities. It has been extensively confirmed that a patient’s functional status reliably predicts perioperative and long-term cardiac events [23–26]. For asymptomatic patients with a functional capacity of 4 METs or above, the need for any active preoperative cardiac intervention to lower the perioperative risk is unlikely [11].
-
Step 3
If the patient has poor functional capacity, is symptomatic, or has unknown function, then the presence of clinical risk factors including [1] coronary artery disease [2], compensated heart failure [3], previous cerebrovascular accident [4], diabetes mellitus, and [5] renal insufficiency, will determine the need for further evaluation (modified from [11]).
As hip repair surgery is considered intermediate-risk surgery, even in the presence of risk factors, further cardiac investigations are not generally considered necessary.
While fulfilling these three steps mentioned above provides cardiac clearance for surgery, underlying medical conditions may still warrant medical attention and cardiac consultation, for example, patients with medical assistance devices (permanent pacemaker and automatic implantable cardioverter defibrillator), and those prescribed dual antiplatelet agents or oral anticoagulants.
Clinical pathway for hip fracture management
While the above-described guidelines provide an invaluable tool for the attending cardiologist to determine perioperative risk for a patient with hip fracture, it does not alert the primary clinician, often an orthopedic surgeon, as to when a cardiac consultation should be initiated. Surgery may be delayed because cardiac clearance cannot be promptly obtained. In order to “fast-track” hip fracture patients for a timely surgery (within the first 24 h), a clinical pathway for hip fracture management has been implemented at our hospital since 2008. The frontline orthopedic surgeon and/or intern evaluates the patient’s cardiovascular status according to a checklist (Appendix 1) and determines whether a cardiac consultation is required, even prior to the anesthetist’s assessment. As a result, cardiac clearance is usually obtained within the same day. When further investigations, such as echocardiography, are required, they can be scheduled for the following morning. Surgery can still be performed within 24 h of admission.
Summary
Hip fracture represents one of the major medical problems faced by our aging society. Early surgery may reduce in-hospital, short-term, and long-term morbidity and mortality. Careful screening of patients with hip fracture to enable prompt cardiac assessment can improve overall outcome by minimizing unnecessary delays for cardiac clearance.
References
Cooper C, Campion G, Melton LJ 3rd (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2:285–289
Lauritzen JB, Schwarz P, Lund B, McNair P, Transbol I (1993) Changing incidence and residual lifetime risk of common osteoporosis-related fractures. Osteoporos Int 3:127–132
Goldacre MJ, Roberts SE, Yeates D (2002) Mortality after admission to hospital with fractured neck of femur: database study. BMJ 325:868–869
Miller CW (1978) Survival and ambulation following hip fracture. J Bone Joint Surg Am 60:930–934
Roberts SE, Goldacre MJ (2003) Time trends and demography of mortality after fractured neck of femur in an English population, 1968–98: database study. BMJ 327:771–775
Wolinsky FD, Fitzgerald JF, Stump TE (1997) The effect of hip fracture on mortality, hospitalization, and functional status: a prospective study. Am J Public Health 87:398–403
Woolf AD, Pfleger B (2003) Burden of major musculoskeletal conditions. Bull World Health Organ 81:646–656
Shiga T, Wajima Z, Ohe Y (2008) Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth 55:146–154
Network SIG (2002) Prevention and management of hip fracture in older people: a national clinical guideline. pp 1–40
Cooney LM Jr (1997) Hip fracture outcomes. Arch Intern Med 157:485–486
Fleisher LA, Beckman JA, Brown KA, Calkins H, Chaikof E, Fleischmann KE, Freeman WK, Froehlich JB, Kasper EK, Kersten JR, Riegel B, Robb JF, Smith SC Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Buller CE, Creager MA, Ettinger SM, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Lytle BW, Nishimura R, Ornato JP, Page RL, Tarkington LG, Yancy CW (2007) ACC/AHA 2007 guidelines on perioperative cardiovascular evaluation and care for noncardiac surgery: a report of the American college of cardiology/American heart association task force on practice guidelines (writing committee to revise the 2002 guidelines on perioperative cardiovascular evaluation for noncardiac surgery): developed in collaboration with the American society of echocardiography, American society of nuclear cardiology, heart rhythm society, society of cardiovascular anesthesiologists, society for cardiovascular angiography and interventions, society for vascular medicine and biology, and society for vascular surgery. Circulation 116:e418–e499
Lawrence VA, Hilsenbeck SG, Noveck H, Poses RM, Carson JL (2002) Medical complications and outcomes after hip fracture repair. Arch Intern Med 162:2053–2057
Carbone L, Buzkova P, Fink HA, Lee JS, Chen Z, Ahmed A, Parashar S, Robbins JR (2010) Hip fractures and heart failure: findings from the Cardiovascular Health Study. Eur Heart J 31:77–84
Lee TH, Marcantonio ER, Mangione CM, Thomas EJ, Polanczyk CA, Cook EF, Sugarbaker DJ, Donaldson MC, Poss R, Ho KK, Ludwig LE, Pedan A, Goldman L (1999) Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 100:1043–1049
Detsky AS, Abrams HB, Forbath N, Scott JG, Hilliard JR (1986) Cardiac assessment for patients undergoing noncardiac surgery. A multifactorial clinical risk index. Arch Intern Med 146:2131–2134
Goldman L, Caldera DL, Nussbaum SR, Southwick FS, Krogstad D, Murray B, Burke DS, O’Malley TA, Goroll AH, Caplan CH, Nolan J, Carabello B, Slater EE (1977) Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 297:845–850
Chambers J (2005) Aortic stenosis. Bmj 330:801–802
Lindroos M, Kupari M, Heikkila J, Tilvis R (1993) Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol 21:1220–1225
Stewart BF, Siscovick D, Lind BK, Gardin JM, Gottdiener JS, Smith VE, Kitzman DW, Otto CM (1997) Clinical factors associated with calcific aortic valve disease. Cardiovascular health study. J Am Coll Cardiol 29:630–634
McBrien ME, Heyburn G, Stevenson M, McDonald S, Johnston NJ, Elliott JR, Beringer TR (2009) Previously undiagnosed aortic stenosis revealed by auscultation in the hip fracture population—echocardiographic findings, management and outcome. Anaesthesia 64:863–870
Network SIG (2009) Management of hip fracture in older people. pp 1–48
Adunsky A, Kaplan A, Arad M, Mizrahi EH, Gottlieb S (2008) Aortic stenosis in elderly hip fractured patients. Arch Gerontol Geriatr 46:401–408
Bartels C, Bechtel JF, Hossmann V, Horsch S (1997) Cardiac risk stratification for high-risk vascular surgery. Circulation 95:2473–2475
Myers J, Do D, Herbert W, Ribisl P, Froelicher VF (1994) A nomogram to predict exercise capacity from a specific activity questionnaire and clinical data. Am J Cardiol 73:591–596
Nelson CL, Herndon JE, Mark DB, Pryor DB, Califf RM, Hlatky MA (1991) Relation of clinical and angiographic factors to functional capacity as measured by the Duke activity status index. Am J Cardiol 68:973–975
Older P, Hall A, Hader R (1999) Cardiopulmonary exercise testing as a screening test for perioperative management of major surgery in the elderly. Chest 116:355–362
Conflicts of interest
Dr. Leung is the speaker for Synthes and has received research support from Synthes. None of the other authors has a real or perceived conflict of interest or a disclosure of any personal or financial support.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 52 kb)
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Siu, C.W., Sun, N.C.H., Lau, T.W. et al. Preoperative cardiac risk assessment in geriatric patients with hip fractures: an orthopedic surgeons’ perspective. Osteoporos Int 21 (Suppl 4), 587–591 (2010). https://doi.org/10.1007/s00198-010-1393-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1393-0