Abstract
Adequate intraoperative infusion therapy is essential for the perioperative outcome of a patient. Both hypo- and hypervolemia can lead to an increased rate of perioperative complications and to a worse outcome. Perioperative infusion therapy should therefore be needs-based. The primary objective is the maintenance of preoperative normovolemia using a rational infusion strategy. Perioperative fluid losses should be differentiated from volume losses due to surgical bleeding or protein losses into the interstitial space. Fluid loss via urine excretion or insensible perspiration (0.5–1.0 ml/kg/h) should be replaced with balanced, isooncotic, crystalloid infusion solutions in a ratio of 1:1. Volume therapy stage 1: intraoperative volume losses up to a blood loss corresponding to 20% of the patient’s total blood volume are compensated for by balanced crystalloids in a ratio of 4–5:1. Stage 2: blood losses exceeding this level are to be treated with isooncotic colloids (preferably balanced) in a 1:1 ratio. In this regard taking into consideration the contraindications, e. g., sepsis, burns, critical illness (usually patients in the intensive care unit), impaired renal function or renal replacement therapy, intracranial hemorrhage, or severe coagulopathy, artificial colloids such as hydroxyethyl starch (HES) can be used perioperatively for volume replacement. Stage 3: if an allogeneic blood transfusion is indicated, blood and blood products are applied in a differentiated manner.
Zusammenfassung
Eine adäquate intraoperative Infusionstherapie ist wesentlich für das perioperative Outcome eines Patienten. Sowohl Hypo- als auch Hypervolämie können zu einer erhöhten Rate perioperativer Komplikationen führen und somit zu einem schlechteren Behandlungsergebnis. Daher sollte die perioperative Flüssigkeitstherapie bedarfsgerecht und zielorientiert durchgeführt werden. Das Hauptziel ist die präoperative Normovolämie durch eine rationale Infusionstherapie aufrechtzuerhalten. Perioperative Flüssigkeitsverluste sollten dabei von Volumenverlusten durch chirurgische Blutungen oder Proteinverlusten ins Interstitium differenziert werden. Flüssigkeitsverluste via Urinexkretion oder Perspiratio insensibilis (0,5–1,0 ml/kg/h) sollten 1:1 mit balancierten, isoonkotischen, kristalloiden Infusionslösungen ausgeglichen werden. Volumentherapie, Stufe 1: Intraoperative Volumenverluste bis zu einem Blutverlust von 20 % des Gesamtblutvolumens werden mit balancierten Kristalloiden im Verhältnis 4–5:1 ausgeglichen. Stufe 2: Darüber hinausgehende Blutverluste sind im Verhältnis 1:1 mit isoonkotischen Kolloiden (bevorzugt balanciert) zu behandeln. In dieser Hinsicht und unter Beachtung der Kontraindikationen wie Sepsis, Verbrennungen, kritische Erkrankung (i. d. R. Patienten auf Intensivstation), eingeschränkte Nierenfunktion oder Nierenersatztherapie, intrakranielle Blutung oder schwere Gerinnungsstörungen können perioperativ auch künstliche Kolloide, wie z. B. HES, zum Volumenersatz verwendet werden. Stufe 3: Wenn die Indikation zur Gabe von Fremdblut besteht, erfolgt ein differenzierter Einsatz von Blut und Blutprodukten.
Similar content being viewed by others
Prologue
Water is a friendly element for anyone who is familiar with it and knows how to handle it.Footnote 1
Johann Wolfgang von Goethe
Adequate infusion therapy represents a challenge for modern surgical, emergency, and intensive care medicine. Volume replacement solutions have been used for this purpose for decades. As their name indicates, these solutions serve as a volume replacement, which is their original and also essential indication. As with all medications, volume replacement products have dose-dependent side effects too and should therefore only be applied in the presence of the corresponding indication. In recent years, several multicenter studies have stimulated an intense and sometimes emotional debate on the benefits and risks of hitherto existing pathophysiology-based treatment concepts.
But what is the objective of an adequate volume therapy?
In healthy individuals, blood volume remains constant within very tight limits during the course of a day. The objective must be to maintain the patient’s normovolemia (Fig. 1) as far as possible. Normovolemia is the prerequisite for ensuring that, for example, cardiac output and oxygen supply are always sufficient and can increase in response to stress at any time. Traditionally, a liberal fluid regime was propagated: “In doubt, give volume!” However, various publications indicate that “restrictive” volume management has advantages over “liberal” volume management. This effect has been impressively demonstrated for major abdominal surgery: the incidence of potentially life-threatening complications, such as pulmonary edema, anastomotic insufficiency, impaired wound healing, and coagulation problems could be reduced by fluid restriction, and postoperative intestinal motility significantly increased [1–6]. However, in this context it is important to note that the terms “restrictive” and “liberal” are not standardized, and their use is unfortunately not uniform. Therefore, when speaking of volume therapy, “restrictive” is being increasingly replaced by the term “needs-based”.
Correlation between fluid balance and perioperative outcome. ANP atrial natriuretic peptide. (Modified from Glassford NJ et al. [7])
The primary goal of perioperative fluid therapy is the extracellular space, which is divided into two functional compartments by the intact vascular barrier [2]. The intention behind adequate volume therapy is maintaining normovolemia, extracellular homeostasis between the intra- and extravascular spaces (Fig. 1). In the perioperative period it seems reasonable to distinguish between fluid losses (extravascular space) without colloid-osmotically active molecules (such as urine and perspiratio) and volume losses (intravascular space), i. e., fluid with oncotically active macromolecules (blood or plasma losses from the intravascular space). These different entities are treated by the differentiated application of infusion solutions, crystalloids, and colloids [8]. The way this can be successfully achieved is described below by a fundamental presentation of therapeutic options and their significance in terms of the risk–benefit ratio and by consideration of a practical case that could be encountered in daily practice. The concept of loss-adapted fluid and volume therapy is based on the patient’s preoperative normovolemia. This is normally present in patients without internal medicine complaints, despite fasting [9]. As mentioned above, under normal conditions, the blood volume of a healthy individual remains physiologically very constant over the course of the entire day; it varies by only a few deciliter. Drinking is by no means the only regulatory factor: the permanent filtering and reabsorption of fluid out of and from the interstitial space plays a major role. A detailed description of the perioperative changes in hemodynamics induced by volume deficit or expansion would exceed the scope of this article; thus, this is intentionally not presented. However, in an illustrative case example of a situation that can arise any day in the operating room the effect of hypovolemia on hemodynamics and organ perfusion is exemplarily portrayed.
The foundation: efficiency, effectiveness, and evidence
Careful evaluation of efficiency, effectiveness, and evidence is essential for successful application of a particular medical treatment. To enable the reader to make his/her own best possible evaluation of the current data on fluid therapy, including understanding a viable infusion strategy, the genuine meanings of the terms efficiency, effectiveness, and evidence are explained in the following: Efficiency is the effort, in relation to completeness and accuracy, that is required to attain a particular objective. In contrast, effectiveness describes the degree to which the objective is attained (efficacy and quality). To enable these two terms to be understood more easily, the following practical example may be considered: After sport and sweating correspondingly, a fluid deficit of 500 ml can be efficiently and effectively treated by drinking water. Leaving aside cost considerations, drinking 500 ml of prosecco or even whiskey would be just as efficient in this instance. In terms of treatment of the fluid deficit alone, all three “therapeutic” regimens can be considered equally efficient and effective; however, drinking prosecco or whisky is associated with additional “side effects.” The effectiveness of a treatment must, thus, always be seen broader than as an achievement of the therapeutic goal. Efficiency is important, but if the wrong things are efficiently accomplished, then this constitutes a waste of resources and a risk for the patient. Strategy (effectiveness) thus comes before efficiency in fluid therapy, too. Completing the circle, the question of the safety of a therapy and the corresponding evidence demonstrating that the benefits outweigh the risks always arises, too. Evidence – and this is very important – means “proof.” Evidence in medicine refers to the empirical verification of the benefit of a diagnostic or therapeutic action. This forms the basis of evidence-based medicine.
Evidence in medicine must not be confused with the German word “Evidenz” which means obviousness/no proof is required and therefore just describes the cognitive comprehensibility of a possible relationship. This is illustrated by the following simple example: Two potentially nephrotoxic infusion solutions are tested by comparing them with one another in two study arms. No differences are found in renal function or renal replacement therapy, so there is nothing to obviously imply a kidney-damaging effect of the two substances. However, this of course does not prove the safety (no damaging side effects in terms of renal function) of either of the solutions. In order to produce “evidence,” a valid control group is necessary, as are appropriate function tests, observation periods, and patient/control numbers (“power”). This of course represents a significant challenge, and not all questions can be answered with the help of evidence-based medicine particularly in view of limited resources. The Cochrane Collaboration has set itself the task of describing evidence-based medicine and works to generate, update, and disseminate systematic review articles. The analyses are based on the “Cochrane Database of Systematic Reviews,” which is renewed quarterly as part of the Cochrane Library. The Cochrane Collaboration defined the types of Cochrane evidence listed in Table 1. Systematic reviews based on data from randomized controlled trials (RCTs) of sufficient size and power represent the highest level of evidence. The opinions and recommendations of reputable authorities and expert panels represent the lowest level of evidence according to this list, and can neither replace nor refute the results and findings of large RCTs [10]. Recommendations based on low-level evidence frequently find their way into guidelines, which may also be related to the experts’ conflicts of interests. Although these must be disclosed, the declaration does not balance out or even negate the conflicts of interests:
Standards for the evaluation and management of conflicts of interests in guidelines are lacking and should be urgently developed Footnote 2 [11].
Therefore, it can not be excluded that guidelines are, to some extent, influenced by the evaluations or even wishes of pharmaceutical companies.
There are two fundamental principles for the use of evidence-based medicine:
-
1.
“Absence of evidence is not evidence of absence!” This means: If there is no evidence for a therapy, this still is not a license to proceed at will. Consider the following currently relevant example of liver transplant and alcohol consumption, which also has to do with fluids: In light of the fact that there is no evidence demonstrating the benefit of abstinence from alcohol prior to transplantation, its importance is currently the subject of debate. “The required 6‑month period of abstinence from alcohol excludes patients from a potentially life-saving treatment. In light of the far-reaching consequences of this regulation, special demands are to be placed on the reliability of the underlying evidence: The data should demonstrate clearly that the survival times of relapsed patients are significantly reduced by the renewed consumption of alcohol” [12]. The concept of evidence-based medicine is misunderstood here: It is well known that alcohol (even in small quantities) can have hepatotoxic effects. Clinical experience has shown that in a nonnegligible number of patients a rapid improvement in organ function due to alcohol abstinence because of their potential listing for a potential liver transplant renders the transplant no longer necessary. Furthermore, it cannot be doubted that alcohol will continue to have an hepatotoxic effect after the transplantation – a transplanted liver is not “alcohol resistant.” Purely because no “evidence” is available, i. e., there are no sufficiently large controlled studies clearly proving these correlations in this special population, the universally valid pathophysiology or “common knowledge” must not be ignored. This is also true for infusion therapy, e. g., gelatin: There is a lack of large controlled trials with the corresponding long-term follow-up to prove that gelatin is not safe (see also below “Evidence in volume therapy: Gelatin”). However, the lack of these data of course does not prove the safety of this infusion solution.
-
2.
“Presence of evidence is evidently present!” For example, if it has been shown in controlled studies, i. e., blinded prospective randomized trials, that the adverse effects of a treatment outweigh the benefits in a particular patient collective, this result cannot be “topped” or refuted by studies of a lower-level evidence type, such as register or observational studies. Available evidence cannot be negated in this manner, even if certain representatives of profit-oriented pharmaceutical companies would understandably wish to see it otherwise.
Since in clinical routine there are sometimes situations in which clinicians occasionally do not know what to do, volume therapy is sometimes not performed according to the findings of the large studies and metaanalyses, but rather empirically, based on “gut feeling.” However, which sustained findings concerning infusion therapy can be provided by physiology and evidence-based medicine?
Physiology and effectiveness in infusion therapy
Fluid therapy comprises administration of crystalloids and colloids. Crystalloids are solutions of water and electrolytes; colloids also contain substances with water-binding properties, e. g., albumin, hydroxyethyl starch (HES), or gelatin. The type and composition of the solution to be infused should be adapted to the fluid compartment that is the target of therapy. This is the reason for the development of, e. g., isotonic infusion solutions. As already mentioned, it must be discriminated between fluid losses with and without loss of oncotically active macromolecules. From this results the differentiation of volume losses out of the intravascular and interstitial spaces (loss of oncotically active macromolecules, e. g., albumin) from fluid losses such as urine, insensible perspiration (quantitative 0.5 ml/kg/h, with maximal eventration 1 ml/kg/h), or preoperative dehydration (no loss of oncotically active macromolecules, but pure fluid deficit). With each episode of blood loss, patients lose a sometimes considerable amount of protein – depending on the amount of blood loss. Therefore, if blood loss is compensated for to a large extent using pure crystalline solutions, the colloid osmotic pressure in the blood vessel system will drop significantly. Moreover, during major tumor surgeries, considerable quantities of macromolecules – protein and HES – are lost into the interstitial space, the so-called protein [13] or HES shift [14–16]. These are losses of protein or HES that can not be explained by surgical bleeding or urine. For example, in ovarian cancer patients, in addition to the protein loss resulting from surgical bleeding (1700 ml, 67 g protein loss), a mean intraoperative protein shift of 49 g occurred [13]. In patients with radical hysterectomy, it was shown that 30% of the applied HES molecules left the vascular bed (mean loss via surgical bleeding: 18 g, mean excretion of HES in urine: 18 g, mean HES shift: 30 g) [16]. Both HES or protein loss via surgical bleeding and the shift of protein or HES into the interstitial space reduces the intravascular colloid osmotic pressure, thus, exacerbating edema formation due to extravasation of fluid.
In order to develop a viable strategy to replace all of these fluid and colloid osmotic pressure losses in a demand-oriented manner, it is important to know how effective the various available infusion solutions are.
The “volume effect” of infusion solutions refers to the proportion of the infusion solution that remains in the vascular system after intravenous application. If this is 100%, the entire infusion remains in the intravascular space; if the value is 20%, this indicates a high degree of extravasation (80%), with the danger of interstitial edema. If the volume effect is 180%, this means that the infusion solution draws fluid from the interstitial space back into the vascular system due to the high intrinsic colloid osmotic pressure. Many data are available on this effect and evidence of this effect is listed in Table 2. The most reliable method for investigating the actual volume effect has proved to be direct measurement of blood volume before and after the application of an infusion solution (Table 2; [8, 14, 16–20]). The crucial pharmacodynamic property of the colloids is their relatively large volume effect [8]. These are represented in clinical routine by human albumin (HA), HES, and gelatin preparations. The application of colloids for the treatment of volume losses can thus be considered very effective. As can be seen in Table 2, the volume effects of isooncotic colloids applied to replace blood losses (acute normovolemic hemodilution, ANH) are about five times those of crystalloids. This means that in order to approximately maintain normovolemia, 4–5 l of crystalloid have to be infused to replace a blood loss of 1 l. Therefore, the application of crystalloids alone is not only not very effective, it also leads to a pronounced positive fluid balance (interstitial edema), particularly in case of large blood losses. This, in turn, has an unfavorable impact on treatment outcome. In contrast, a blood loss of 1 liter can be adequately treated using only 1 l of isooncotic HES or albumin. The volume effect of colloids is, however, crucially dependent on the integrity of the vascular barrier.
The vascular barrier
The vascular barrier separating the blood vessels from the interstitial space is a double barrier. It is composed of endothelial cells and the endothelial glycocalyx, a layer of proteoglycans and glycosaminoglycans at the luminal side of the endothelial cells (Fig. 2a). Due to its charge properties, this layer binds albumin and concentrates it, such that the glycocalyx develops its own colloid osmotic competence. This layer is responsible for the maintenance of the Starling colloid osmotic pressure gradient. Directly beneath the glycocalyx, the colloid – osmotic pressure is very low. In the interstitial space itself, it once again corresponds approximately to the colloid – osmotic pressure of the intravascular space [22, 23]. Provided the endothelial glycocalyx is intact, the volume effects of colloids are very large, as described above. However, if the glycocalyx has been destroyed (Fig. 2b), as can occur, e. g., in sepsis, then the volume effects of colloids are greatly reduced. It is likely that the effectiveness of isooncotic colloids in this situation is no longer five times, but rather only about twice that of crystalloid solutions. An inappropriate infusion therapy can also be the cause of a leaky vascular barrier. Volume loading is associated with small volume effects, but also with adverse events [24]. This owes to the fact that volume loading (infusion in the absence of corresponding fluid loss) causes expansion of the atria and thus release of atrial natriuretic peptide (ANP) [25–27]. This peptide alters the endothelial glycocalyx, thus, increasing extravasation of macromolecules (colloids) and fluid. The release of glycocalyx components into the circulation can also impair coagulation due to the heparinoid effect of the released heparan sulfate. This can increase the postoperative risk of thrombosis as the freely circulating glycocalyx components are excreted via the kidneys. Afterwards, plasmatic coagulation is no longer impaired by these components; however, continuously uncovered by the glycocalyx endothelial cells promote adhesion of thrombocytes. Once destroyed, it likely takes 7–10 days for the glycocalyx to be completely rebuilt. Volume loading is thus not recommended under normovolemic conditions. In the absence of an intact vascular barrier (e. g., in sepsis), extravasation, particularly extravasation of synthetic colloids, should be kept at a minimum (to avoid undesired deposition of colloids in tissue) [28]. Based on pathophysiological considerations, albumin should be preferred to the artificial colloids HES or gelatin in this situation. However, this raises the following question: Is the application of infusion solutions, particularly colloids, safe?
a Structure of the intact endothelial glycocalyx. The integration and concentration of plasma proteins generates a high colloid – osmotic pressure in the glycocalyx, which retains fluid in the vascular system. b Pathophysiologic situation following degradation of the endothelial glycocalyx. Release of the plasma proteoglycans leads to adhesion of blood cells and efflux of macromolecules from the vascular system. vWF von Willebrand Factor, ICAM intercellular adhesion molecule, VCAM vascular adhesion molecule, HES hydroxyethyl starch. (Modified from [29])
Evidence in fluid therapy
Crystalloids
Perioperatively and in the intensive care units, the use of balanced isotonic crystalline solutions is increasing. This is because physiologic saline solution causes hyperchloremic acidosis in a dose-dependent manner [30]. In comparison to balanced solutions, this reduces splanchnic bed and renal perfusion, reduces urine excretion, and increases the incidence of nausea and vomiting [31]. There are also indications that balanced solutions are associated with advantages in terms of patient survival [32]. But in contrast, a recently published study found no survival benefit of balanced solution compared to saline solution [33]; however, the applied amount of infusion was so small in this study (<2 l applied slowly during the course of several days) that neither the chloride concentration nor the pH in the saline group could increase above or drop below the respective normal values. At ISICEM 2016, Kellum presented results from a very large cohort of patients demonstrating that larger amounts of saline solution were associated with increased mortality compared to balanced solutions. These results were published as the current article was in press [34]. Contrary to widespread belief, the potassium content of balanced solutions does not cause hyperkalemia in renal insufficiency patients [35, 36]. In fact, it has been shown for kidney transplantation that even in the anuric phase a potassium-containing (up to 5 mmol/l) balanced solution is superior to 0.9% NaCl [35]. This is because the hyperchloremic acidosis caused by saline solution promotes potassium drift from the intracellular space into the intravascular space, which favors hyperkalemia. Even infused in large amounts, a balanced infusion solution with a potassium content of 4–5 mmol/l cannot cause hyperkalemia, since it is not hyperkalemic. Only if the patient has a pronounced pure water diuresis could balanced solutions theoretically lead to hyperkalemia (concentration effect due to water loss via the kidneys). In summary, it therefore appears rational to use balanced infusion solutions in intensive care medicine and in the OR, and to apply isotonic saline solutions only in special situations, e. g., cholera (substained losses of chloride and sodium).
Albumin
Albumin is a 585-amino acid protein with a molecular weight of 69 kDa. Albumin-containing infusion solutions are extracted from human blood (and thus require a batch manufacturing record), are considered as virus safe, and can be used to treat hypoalbuminemia. Although albumin level is a frequently measured clinical parameter, no generally valid minimum limit can at present be defined below which replacement should take place. It has been repeatedly demonstrated that pronounced hypoalbuminemia in critically ill patients is associated with poor outcome [37]. Whether or not hypoalbuminemia was indeed the cause of the poor outcome or rather symptomatic of the severity of each particular disease (e. g., nutritional status, degree of inflammation) is still controversially discussed. However, in cases of severe hypoalbuminemia (<2.5 g/dl), there are many indications that albumin administration seems to be beneficial in terms of mortality, organ function, the amount of fluid to be applied (fluid balance), and tolerance of enteral nutrition [37–41]. The endothelial glycocalyx requires a low but nevertheless basal albumin concentration for maintenance of its barrier function. For a long time, albumin was considered the virtually ideal volume substitute, due to its colloid osmotic properties and long intravascular retention time. The volume effect of 20% albumin solution is 185%, which means that this infusion solution can recruit fluid from the interstitial space for the intravascular space. The volume effect is higher than the entire volume of the infused solution. Albumin 5% has a volume effect of 85%, meaning that almost all of the infused fluid remains in the vascular system. Albumin was thus used for decades as the reference substance during development of artificial colloidal plasma replacement products. Since the development of cheaper artificial colloids, the application of albumin as a volume replacement product has decreased considerably. An older Cochrane analysis demonstrating increased mortality among critically ill patients receiving albumin contributed significantly to this trend [42]. Volume replacement with albumin was subsequently investigated in several large-scale prospective trials. The Australian SAFE trial investigated the safety of infusion therapy with human albumin in intensive care patients [43, 44] and was unable to show any severe adverse effects compared to 0.9% saline infusion; nor, however, was the outcome of the albumin-treated patients better [43, 44]. The ALBIOS trial evaluated a patient collective with severe sepsis or septic shock. The experimental group received albumin replacement (not for volume therapy, but rather to increase the serum albumin concentration to ≥3 g/dl) and the control group received only crystalloid solution [45]. There was no difference in terms of mortality between the two groups [45]. In the similarly conceived EARSS trial, a reduction in absolute and relative mortality of 2.2% and 8.4%, respectively, was observed in the human albumin group compared to the crystalloid group after 28 days (p > 0.05) [46]. Wiedermann’s meta-analysis [47] of pooled data from the SAFE, EARSS, and ALBIOS trials reported that albumin application in patients with severe sepsis or septic shock was associated with significantly reduced mortality (p = 0.046). An almost simultaneously published meta-analysis did not arrive at this result (p = 0.08); however, this study also included patients from two other very small studies, which were not designed and standardized for addressing the endpoint “outcome” (unfortunately, this is a frequent shortcoming of meta-analyses). Additionally, this study did not use the correct patient numbers from the original ALBIOS study publication [48]. In contrast to hyperoncotic HES solution, no negative impact of albumin on renal function could be shown [49].
Whether the positive effects of infusions are realized or are outweighed by their adverse effects, however, always depends on the applied dose and a correctly established indication. It was shown that mortality in children with a severe infection significantly increased following application of a large fluid bolus (albumin or isotonic saline solution; 20–40 ml/kg). However, in comparison over 90% of the children had no clinical signs of hypovolemia [50]. Application of high doses of infusion solutions in the absence of volume requirements must be viewed critically, irrespective of the type of solution. However, use of human albumin as volume replacement for stabilization of hemodynamics is nowadays widely accepted.
In summary, the base of high-quality data (level of evidence Ia) confirms the effectiveness, efficiency, and safety of human albumin. These data are not only available from sufficiently large RCTs, but also from significant meta-analyses of these RCTs (Table 1). Compared to synthetic colloids, human albumin is a very expensive treatment option [51]. For this reason, albumin should not be used where other therapeutic alternatives (e. g., crystalline solutions or synthetic colloids) are possible. Two post hoc analyses demonstrated reduced mortality in severe sepsis (SAFE) and septic shock (ALBIOS) achieved by albumin application. It would be wrong to conclude that this demonstrates that albumin is an effective treatment for sepsis. Administration of antibiotics as early as possible and a causal treatment (e. g., curing of infection) is undoubtedly far more effective. However, many available data indicate that hypoalbuminemia (<2.5 g/dl) in sepsis patients should be treated early by appropriate administration of albumin [43, 47, 52, 53]. Therapeutic target should be an albumin concentration of over 2.5 g/dl, which is most effectively achieved with a hyperoncotic albumin solution (albumin 20%).
Hydroxyethyl starch (HES)
HES solutions are synthesized from plant-derived starch (waxy corn or potato starch). A proportion of the cyclic glucose rings in the starch is substituted with hydroxyethyl groups. For example, the indication 130,000/0.4 means that the starch, with a molecular weight of 130,000 Da, carries hydroxyethyl groups on 40% of the glucose rings. The volume effect of HES 130,000 is almost 100% and can thus be described as ideal in terms of volume replacement. Although various smaller studies in different patient cohorts found no negative effects due to the application of HES as part of a combined HES and electrolyte solution therapy, studies in intensive care medicine have revealed a different picture. The VISEP trial in patients with severe sepsis found a negative effect on renal function, which was frequently observed only at later time points (observation time was 90 days) [54]. In this study, an older HES preparation was used in a hyperoncotic form (10%) and administered to a high cumulative dose. The blinded randomized prospective 6S trial [55] compared treatment with 6% HES 130,000/0.42 with Ringer’s acetate application in sepsis patients. This study also revealed an increased rate of renal replacement therapy and, furthermore, increased mortality following HES therapy. Another blinded randomized prospective study, the CHEST trial, investigated a large mixed cohort of patients requiring postoperative intensive care, but of whom the majority were not septic patients [56]. This study showed an increased rate of renal replacement therapy following HES treatment (p = 0.04) and no difference in mortality after 90 days, although circulatory stabilization was achieved more quickly using HES volume replacement. Also the CRYSTMAS trial [57] investigated a sepsis patient cohort and demonstrated that HES 130,000/0.4-based volume replacement therapy resulted in more rapid hemodynamic stabilization compared to 0.9% saline solution. This trial found no significant difference between the groups in terms of renal function and mortality, which may be due to the comparatively small number of patients (n = 174).
Meta-analyses containing these intensive care medicine RCTs (level of evidence Ia) demonstrate that in critically ill patients, particularly in those suffering from sepsis or septic shock, application of HES is associated with an increased incidence of renal failure and a higher rate of renal replacement therapies [58–60]. Subsequently, on the basis of these results, in October 2013, the Pharmacovigilance Risk Assessment Committee (PRAC) of the European Medicines Agency issued the recommendation that HES should no longer be used in critically ill patients as well as those suffering from sepsis or burns. Additionally, it was also recommended not to continue HES treatment for more than 24 h and to monitor renal function for 90 days [61, 62].
However, the controversial debate surrounding the safety of HES was not silenced by these measures. On the contrary, the available studies were criticized for their lack of comparability (patient cohort, patients’ status at randomization, use of volume products, maximum HES dose). Meybohm et al. [63] reevaluated the prospective randomized studies and defined a six-point catalog of criteria that should be fulfilled by future studies in order to be able to be used for comparison of different infusion regimes:
-
short time interval between shock event and randomization,
-
limited use of initial fluid therapy,
-
consistent use of a fixed infusion algorithm until hemodynamic stabilization,
-
reproducible criteria for hypovolemia,
-
maximum doses of HES,
-
exclusion of patients with preexisting impaired renal function or renal replacement therapy.
The studies mentioned above only partially fulfill these criteria [63]. So far, controlled trials fulfilling all criteria mentioned above, with high case numbers and long observation period of at least 90 days, are unfortunately not available. Whether HES 130,000/0.4 has a more favorable safety profile in sepsis patients and is thus associated with a lower rate of renal function-related adverse events in long-term follow-up compared to older starch preparations is currently unclear [58]. Therefore, no HES preparations at all should be used in this special patient collective (see also section “Practical conclusion – the synopsis”). By way of precaution, the German Society of Anesthesiology and Intensive Care Medicine (DGAI) recommends that the application of modern low molecular HES solutions in intensive care patients should be evaluated critically on an individual basis and that their use should be restricted to patients with acute life-threatening blood and volume losses not manageable by other means. This means, for example, that a patient having undergone aortic stent grafting, who is postoperatively only in the intensive care unit for monitoring purposes and suddenly suffers massive hypovolemic shock due to aortic rupture, can of course receive larger amounts of HES as an already initially lifesaving treatment, even though the situation takes place in the intensive care unit.
Do these considerations also apply to the use of HES preparations as a volume replacement solution in the OR?
After the regulatory authorities initially suspended the entire approval for HES preparations, it was also no longer permitted to use these during surgery for a while. In two industry-supported meta-analyses, the safety of cornstarch 130,000/0.4 was investigated in a large number of surgical patients. The authors found no significant difference to the control group and attested to the safety of this cornstarch. However, the majority of the included studies had insufficiently long observation periods and no real control group. A further study without industry funding came to the same conclusion with the same shortcomings of the included studies [64]. To prove the safety of HES in the OR – analogous to intensive care medicine – correspondingly conceived, randomized, controlled, and blinded trials are also required. Results from studies of this type are not yet available [65].
Where evidence is insufficient, pathophysiologic considerations will help: The potential nephrotoxic properties of HES 130,000/0.4 have almost exclusively been demonstrated in seriously ill intensive care patients to date. It seems highly likely (even though this may be speculative) that patients with normal renal function are considerably less sensitive to the potential nephrotoxic effects of HES 130,000/0.4 than intensive care patients who are already seriously ill. If these patients are not treated with colloids in the event of loss of larger amounts of blood, either very large amounts of crystalloids are required – with all the adverse effects of the resulting positive fluid balance – or the unavoidably arising hypovolemia with hypotension and subsequent vasopressor application will very likely endanger renal function. However, this dilemma can be solved by considering the effectiveness: If a nephrotoxic effect of HES 130,000/0.4 is present at all in otherwise healthy patients in the OR, then the data from intensive care medicine indicate that HES-associated perioperative renal failure is likely to be a rare event, since even in this patient collective very high case numbers are required in order to detect this effect. In contrast, prerenal acute kidney failure is much more likely to be caused by severe hypovolemia. This “effect-based” risk analysis clearly favours the use of HES 130,000/0.4 for correctly indicated treatment of larger blood losses in the OR. If one wishes to eliminate every risk, even a theoretical risk, then the expensive albumin preparations discussed above must also be used in the OR.
A further potential adverse effect of HES 130,000 is its – albeit minor – negative impact on blood coagulation, which goes beyond the effect of simple dilution of coagulation factors [51]. This and the potential impairment of renal function provide the reason for dose limitation (30 ml/kg). A recently published meta-analysis showed that HES application can result in a larger intraoperative blood loss compared to crystalloid therapy alone [66]. However, it must be noted that larger blood losses are often not appropriately treated by the sole application of crystalloid. The drop in blood pressure caused by hypovolemia can itself decrease blood losses. Slightly reduced blood losses should not be an argument for neglecting the objective of demand-oriented maintenance of normovolemia, since the predominant application of vasopressors for the compensation of a volume deficit can seriously impair perfusion of organs such as the kidneys.
The concept propagated in the past, namely that patients be prophylactically “volume loaded” prior to surgery, e. g., by HES application, should also be viewed critically, due to the possible impairment of the vascular barrier function [8]. This also applies to Caesarean section patients, since the safety of artificial colloids for mother and child has not yet been sufficiently proven (by RCTs with high case numbers and long-term follow-up). Pregnant women generally have a high normal blood volume prior to parturition per se, which does not have to be and should not be expanded by artificial colloids. In summary, considering the contraindications, the use of HES preparations for compensation of larger blood losses in the OR can be endorsed. As long as sufficiently large controlled studies with long-term follow-up are lacking for the perioperative phase, it is impossible to exclude completely a residual risk (e. g., for renal function).
Gelatin
Alongside HES, gelatin is another artificial colloid employed in the clinical use. Gelatin is a very heterogeneous polypeptide mixture made from the collagenous connective tissue of cattle specially bred for this purpose. Since a part of the applied amount is eliminated via the kidneys already during its infusion, a volume effect of 50–100% can be expected, depending on the preparation [20, 51]. However, this volume effect is only maintained for a maximum of 2 h. The effects on blood coagulation are even less pronounced than with HES preparations. However, intolerance reactions of all degrees of severity have been described for gelatin preparations. It is certain that gelatin preparations elicit the highest rate of anaphylactic reactions of all artificial and natural colloids [61]. Due to the bovine raw material, contamination of gelatin with the agent responsible for causing the new variant of Creutzfeldt-Jakob disease cannot be completely ruled out. Although a chemically very aggressive manufacturing procedure can massively reduce the prions, it cannot completely eliminate them. In the era preceding the first cases of bovine spongiform encephalopathy (BSE) in Germany, the theoretic risk of BSE transmission via gelatin was calculated to be <1:1000000 [61]. In the USA, gelatin solutions are no longer approved; in Germany an obligation for batch documentation is discussed. Animal experiments have shown that gelatin can cause histopathologic changes in the kidneys, such as vacuolization of tubule cells (“osmotic nephrosis-like lesions”) [61]. In critically ill patients, a cumulative gelatin dose >33 ml/kg body weight, is associated – as for HES – with a higher incidence of renal failure [61].
In contrast to the large amount of data available for HES preparations or albumin, there are currently no large randomized studies demonstrating the safety and benefit of treatment with gelatin preparations [67, 68]. According to a 2012 Cochrane analysis, data from RCTs are available for HES from 9147 patients and for albumin from 9920; gelatin, however, has only been subject to controlled investigation in this context in 506 patients [69]. “Absence of evidence” of course does not mean that the preparations can be applied in intensive care medicine or in the OR without hesitation. The fact that there is currently no sufficient evidence for the safety of gelatin solutions – neither in intensive care units nor in OR – does not support their use, but must be assessed as a considerable disadvantage of gelatin compared to albumin and HES [61, 67].
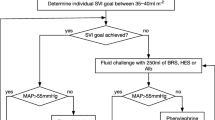
The three-stage concept of volume therapy
As mentioned in the introduction, fluid therapy should be target-directed and loss-adapted, and thus performed in a needs-based manner. The objective of treatment must be normovolemia. There is currently no evidence that volume replacement with colloids reduces patient mortality compared to volume replacement with crystalloids [69]. However, if the volume effects of crystalloids and colloids are considered, colloids are five times more effective than crystalloids, provided they are used to treat the appropriate indication of hypovolemia. This is also confirmed by the results of the CRISTAL trial, which could show a reduction in mortality in patients with hypovolemic shock achieved by volume replacement with colloids [70]. The perioperative infusion therapy comprises different phases, for which different recommendations have to be given:
-
Stage one: basal crystalloid therapy
Fluid losses (urine and insensible perspiration) are replaced in a 1:1 ratio with a balanced crystalloid infusion solution. Additionally, intravascular blood loss must be replaced in a 4–5:1 ratio. This is where the limitation of basal crystalloid therapy is encountered, since this means at the same time the infusion of 80% “interstitial edema”. As already mentioned, establishment of a highly positive fluid balance should not be considered harmless [1, 3–5, 8, 24, 71]. A limit must therefore be defined, above which basal crystalloid therapy is replaced by a treatment of higher effectiveness, in order to avoid the complications and adverse events associated with fluid overload. As a rule of thumb, blood loss corresponding to 20% of the initial blood volume can be stated as the limit. Since most patients in the OR only experience blood losses within this order of magnitude, according to this concept, the majority of patients can be treated without colloid.
-
Stage two: blood losses exceeding 20% of the initial blood volume
Blood loss should be replaced by an effective colloid therapy to prevent the fluid balance becoming too positive. Fluid losses (urine and insensible perspiration) are still replaced in a 1:1 ratio with crystalloids. The largest volume effect has been described for 20% human albumin (Table 2). However, this is also by far the most expensive colloid. Considering the contraindications, artificial isooncotic colloids such as HES may also be used in stage two (1:1 ratio in relation to the blood losses exceeding that of stage 1).
-
Stage three: for very large blood losses
The use of infusion solutions (stages 1 and 2) is limited by the increasing development of anemia and impairment of blood coagulation resulting from the dilution. In addition to the dilution of coagulation factors by the maintenance of normovolemia with decreasing blood volume, gelatin and HES 130,000 also have direct negative effects on blood coagulation. Anemia and the loss of coagulation factors necessitate a differentiated and demand-oriented transfusion of blood products (erythrocyte concentrates, EC; fresh frozen plasma, FFP; thrombocyte concentrates; coagulation factors).
Application of this staged concept ensures a loss-adapted and therefore needs-based volume therapy. However, the three stages should not be followed too dogmatically! For example, should one of the large veins suddenly tear – leading to loss of a large amount of blood within just a few minutes – stage 2 should and must be implemented immediately, since the volume loss must be treated with infusion solutions of high effectiveness without delay. In this scenario, sufficient amounts of colloids should be applied immediately (e. g., 1–2 l of HES) to prevent intraoperative hypovolemia. Blood products may also be administered early.
The example in the following section highlights the importance of correctly defining the fluid and volume requirements; it illuminates the perils of intraoperative infusion therapy on one hand, but also provides important simple hints and tricks on the other.
A practical example – volume therapy explained using simple math
Consider a 52-year-old ovarian cancer patient undergoing exploratory laparotomy. The procedure is conducted under general anesthesia with a previously placed epidural catheter. The patient has no cardiovascular complaints and still does sports; she weighs 67 kg with a height of 168 cm. During surgery the anesthetist endeavors to maintain normovolemia and the mean arterial blood pressure is kept at 60 mm Hg at least. The events, balance status, and laboratory parameters (hemoglobin concentration, Hb and hematocrit, Hct) at various time points during surgery are listed below:
-
Induction:
-
general anesthesia and administration of epidural anesthesia
-
Hb 12.3 g/dl, Hct 39.3%
-
norepinephrine 0.3 mg/h
-
-
1 h after the beginning of surgery:
-
Hb 9.2 g/dl, Hct 29.4%
-
norepinephrine 0.5 mg/h
-
cumulative 1500 ml of crystalloid infused
-
-
2 h after the beginning of surgery:
-
estimated blood loss in towels and aspirators 1500 ml
-
urine excretion 500 ml
-
Hb 8.2 g/dl, Hct 26.2%
-
norepinephrine 1.5 mg/h
-
cumulatively 5000 ml of crystalloid infused
-
-
3 h after the beginning of surgery:
-
surgeon complains of impaired blood coagulation and sustained surgical bleeding
-
administration of three fresh frozen plasma (FFP) (750 ml)
-
Hb 7.0 g/dl, Hct 22.4%
-
norepinephrine 1.8 mg/h
-
infusion of another 1000 ml of crystalloid solution
-
administration of four red cell concentrates (cumulative total of 1200 ml)
-
-
4 h after the beginning of surgery:
-
Hb 7.7 g/dl, Hct 24.6%
-
norepinephrine 1.2 mg/h
-
administration of another three FFP (cumulative total of 1500 ml)
-
thereafter Hb 7.5 g/dl and Hct 24.0%
-
estimated total blood loss 3000 ml
-
total urine excretion 700 ml
-
-
End of surgery 5 h after the beginning of surgery:
-
Hb 7.9 g/dl, Hct 25.3%
-
norepinephrine 0.6 mg/h
-
The patient is extubated and moved to the intensive care unit with noradrenaline 0.7 mg/h. Due to increasing retention parameters, renal replacement therapy is initiated. This has to be continued for 3 days due to acute renal failure. Renal function normalizes hereafter, and after 11 days in the intensive care unit the patient is transferred to a general ward (Table 3).
Why did circulatory / cardiovascular instability and renal failure develop in this patient?
The mathematical solution of this case
Preoperative situation
Based on the patient’s height and weight, a body surface area (BSA) of 1.76 m2 can be calculated [72].
It is assumed that the patient had a normal preoperative blood volume, since patients with a healthy cardiopulmonary status generally have an even high normal morning blood volume despite several hours of fasting [9]. Using the measured normal blood volumes per ml2 of BSA (listed in Table 4; normal female BV: 2245 ml/m2), the blood volume (BV) can be calculated .
Practical tip: BSA can be calculated using tools available online. For a simplified calculation of blood volume, BV =60 ml/kg can be used, although this is less precise than calculations using BSA.
From the Hct value, the red cell volume (RCV) can be calculated.
Practical tip: if only Hb values are available, Hct can be calculated using: Hb (g/dl) × 3.2 = Hct. This requires a normal mean corpuscular hemoglobin concentration (MCHC), which, however, is the case in the vast majority of patients.
Provided the patient remains indeed normovolemic, using the blood volume, it is possible to calculate at every particular timepoint the corresponding erythrocyte volume and thus the change in erythrocyte volume (∆EV) as well as blood loss using the mean Hct value.
For example, the situation 2 h after the beginning of surgery:
Mean Hct (Hctm) is calculated from the sum of all Hct measurements made up until the point in time 2 h after incision divided by the number of measurements. In this example, Hct had been determined n = 3 times by the point in time 2 h after incision
Via Hctm, the blood loss can be calculated from the erythrocyte loss (blood = erythrocytes and plasma):
resulting in
Evaluation of volume therapy at the point in time 2 h after incision
The estimated and the calculated blood loss values were almost identical at this point in time. With a cumulative administration of 5000 ml crystalloid solution, the fluid balance was +2727 ml (calculation: 5000 ml of crystalloid − 134 ml of perspiration − 500 ml of urine − 1639 ml of blood loss). However, despite this, the administered volume therapy was not sufficient.
The following balance 2 h after the start of surgery considers the volume effect of the volume replacement therapy selected in this example and demonstrates the intravascular volume balance. In this case, crystalloids replacing fluid loss due to urine or perspiration are accredited in full, but those replacing blood losses are only accredited to 20%, since only 20% remain intravascularly (the remainder leads to interstitial edema, Table 5 ).
Therefore: At this point in time the patient had a pronounced intravascular hypovolemia (756 ml), which explains the cardiovascular instability and the requirement for 1.5 mg/h of norepinephrine. According to the three-stage concept (see section “The three-stage concept of volume therapy”), the critical value of blood loss corresponding to 20% of the preoperative blood volume should have been calculated first. In a patient with an approximate blood volume of 4000 ml, this corresponds to a blood loss of 800 ml. In stage 1, 4–5-times this amount of blood loss, plus the losses due to urine excretion and perspiration, should have been replaced with crystalloid. This corresponds to approximately 4600 ml (5 × 800 ml + 637 ml). Thereafter, stage 2 should have been observed and further blood losses should have been replaced with colloids. In this example, 800 ml of HES would have been indicated.
Situation at the end of surgery
The calculation of blood loss proceeds analogously to the calculation above for the time point 2 h after the start of surgery.
First the loss of erythrocyte volume is calculated:
To be able to finally calculate the loss of red cells, in addition to the change in red cell volume, the administered red cell concentrates now have to be added to the equation. One unit of a red cell concentrate, having a volume of 300 ml and a Hct of 65%, corresponds to about 200 ml of red cells.
The mean Hct value now enables the blood loss to be calculated from the loss of red cells:
To calculate the final total blood loss, the total loss of red cells is divided by the Hctm value calculated from measurements made throughout the entire surgery. This was
Overall evaluation: Target missed! Pronounced hypovolemia despite a highly positive fluid balance
At +4665 ml, the mere perioperative fluid administration appears very generous; however, the total blood loss was underestimated by 1900 ml. The following overview again considers the volume effect of the selected volume replacement therapy and thus represents the intravascular volume balance (Table 6).
The patient had a severe hypovolemia postoperatively (over 1200 ml volume lacking)! Furthermore, in addition to bleeding during these surgical procedures, large intraoperative protein losses also occur, which have not been included in the calculations presented here.
In summary, in this situation with a blood loss of almost 5 l, the administered volume therapy was not demand-oriented. Less crystalloid but considerably more “volume” (colloid) would have been loss-adapted and the infusion of 2000 ml of HES appropriate. The presented example also demonstrates something fundamental: In patients without internal medicine complaints, if during major surgery a gradual pronounced increase in catecholamine requirement is observed, this is a very strong indication that blood loss is being treated inadequately! The following is, however, speculative: The pronounced hypovolemia with correspondingly high catecholamine requirement had a more severe impact on renal function than “defense” of normovolemia using HES would have had in this renally healthy, noncritically ill patient.
Important comments for bedside blood loss calculation
The calculation presented above is valid for each and every point in time during surgery. Particularly in apparently unclear situations (larger blood losses, transfusion of blood) this calculation will bring clarity. As demonstrated in Fig. 3, the calculation of blood loss always assumes a normovolemic patient. The corresponding volume replacement thus results in dilution; otherwise Hct does not sink logarithmically upon blood loss, as would be the case if normovolemia was maintained. It is important to realize that the blood volume can only increase slightly due to infusions [24]. ANP is released immediately, the vascular barrier becomes permeable, and the blood volume quickly returns to normal high [25–27, 74]. In the case of larger blood losses, a moderate – sometimes considerable, as demonstrated by the presented example – hypovolemia is much more frequent, caused by an apparently generous but in fact inadequate volume therapy. If blood loss is calculated, e. g., at a point in time at which the blood volume is 500 ml less than at the start of surgery, then 500 ml has to be added to the calculated blood loss. If, due to hypovolemia and hemoconcentration, the Hct increases, the result of blood loss calculation will be a negative value and gives an approximation of the extent of hypovolemia.
As shown in Fig. 3, in the incidence of bleeding and normovolemic dilution with infusion solutions, Hct decreases logarithmically [75]. Owing to the simpler mathematics, the calculation of blood loss presented above is not logarithmic, but rather linear. If, for example, only two Hct measurements are made during a bleeding (example 1), then Hctm will be considerably too high and the calculated blood loss therefore too low. It is thus always preferable to input several Hct values into the calculation. In the discussed example, seven Hct measurements were performed (Fig. 3, example 2). Although this is a sufficiently high number, the Hctm will still be somewhat too high and the calculated blood loss will therefore be an underestimation of the actual blood loss. This means that potential hypovolemia and the linearity of the calculation can result in the calculated blood loss being lower than the actual blood loss. However, as the example demonstrates, even a blood loss calculated still too low provides a far better overview than a pure estimation of blood loss, which is unfortunately a very unreliable parameter. Factors contributing to this unreliability include the fact that the losses in towels are very difficult to estimate, blood can flow into unseen regions which the surgeon does not aspirate, and even the blood content of aspirators is difficult to estimate due to rinsing solutions, particularly in case of large blood losses. Unfortunately, considerable underestimation of intraoperative blood losses is thus a frequent event [76]. Therefore, the bedside blood loss calculation presented herein is extremely useful and can even be implemented in anesthesia documentation programs.
Practical conclusion – the synopsis
An adequate intraoperative infusion therapy:
-
should be needs-based, with the aim of normovolemia,
-
should be loss-adapted and distinguish between fluid and volume losses,
-
should balance out fluid losses (urine and insensible perspiration 0.5–1.0 ml/kg/h) with a balanced crystalloid infusion solution in a 1:1 ratio,
-
should first compensate volume losses (intraoperative blood loss) corresponding to up to 20% of the total blood volume with balanced crystalloids in a 4–5:1 ratio, and treat blood losses exceeding this level with isooncotic colloids in a 1:1 ratio.
Considering the contraindications
-
sepsis,
-
burns,
-
critically ill patient (usually in the intensive care unit),
-
impaired renal function or renal replacement therapy,
-
intracranial or cerebral bleeding,
-
severe coagulation disorder
HES can also be used for volume replacement. In patients with a contraindication to HES, albumin solutions should be preferred to gelatin solutions, since there are data available supporting the safety of albumin infusions.
The three-stage concept for loss-adapted and needs-based volume therapy:
-
Stage 1: basal crystalloid therapy. Fluid losses (urine and insensible perspiration) are replaced by a balanced crystalloid infusion solution in a 1:1 ratio. Intravascular blood loss must be additionally compensated in a 4–5:1 ratio.
-
Stage 2: blood losses exceeding 20% of the initial blood volume. Application of colloids (preferably balanced) in a 1:1 ratio for replacement of blood losses exceeding those of stage 1. Fluid losses (urine and insensible perspiration) continue to be replaced in a 1:1 ratio by a balanced crystalloid infusion solution.
-
Stage 3: very large blood losses. Differentiated and needs-based transfusion of blood products, i. e., red cell concentrates and FFPs (adapted to the present coagulation), as well as coagulation factors and thrombocyte concentrates as required.
Bedside blood loss calculation based on normal blood volume and intraoperative Hb or Hct measurements provides the anesthetist with a very good orientation, which renders the objective – maintenance of normovolemia in the patient – easier to achieve. Disregarding coincidences, a fluid and volume therapy can only be needs based if the patients’ requirements are known.
Notes
Quote is translated from German.
Quote is translated from German.
References
Brandstrup B, Tonnesen H, Beier-Holgersen R et al (2003) Effects of intravenous fluid restriction on postoperative complications: Comparison of two perioperative fluid regimens: A randomized assessor-blinded multicenter trial. Ann Surg 238:641–648
Jacob M, Chappell D (2009) Rehm M The ‘third space’ – fact or fiction? Best Pract Res Clin Anaesthesiol 23:145–157
Holte K, Kehlet H (2006) Fluid therapy and surgical outcomes in elective surgery: A need for reassessment in fast-track surgery. J Am Coll Surg 202:971–989
Lobo DN, Bostock KA, Neal KR, Perkins AC, Rowlands BJ, Allison SP (2002) Effect of salt and water balance on recovery of gastrointestinal function after elective colonic resection: A randomised controlled trial. Lancet 359:1812–1818
Nisanevich V, Felsenstein I, Almogy G, Weissman C, Einav S, Matot I (2005) Effect of intraoperative fluid management on outcome after intraabdominal surgery. Anesthesiology 103:25–32
Parquin F, Marchal M, Mehiri S, Herve P, Lescot B (1996) Post-pneumonectomy pulmonary edema: analysis and risk factors. Eur J Cardiothorac Surg 10:929–932 (discussion 33)
Glassford NJ, Myles P, Bellomo R (2012) The Australian approach to peri-operative fluid balance. Curr Opin Anaesthesiol 25:102–110
Chappell D, Jacob M, Hofmann-Kiefer K, Conzen P, Rehm M (2008) A rational approach to perioperative fluid management. Anesthesiology 109:723–740
Jacob M, Chappell D, Conzen P, Finsterer U, Rehm M (2008) Blood volume is normal after pre-operative overnight fasting. Acta Anaesthesiol Scand 52:522–529
Fachgesellschaften_AAWM (2014) Intravasle Volumentherapie beim Erwachsenen (Registernummer 001–020)
Langer T, Conrad S, Fishman L et al (2012) Interessenkonflikte bei Autoren medizinischer Leitlinien. Eine Analyse der Leitlinien deutscher Fachgesellschaften 2009–2011. Dtsch Arztebl 109:836–842
Marckmann G (2015) Alkoholabstinenz vor Lebertransplantation: Contra. Dtsch Arztebl 112:A 279
Rehm M, Haller M, Brechtelsbauer H, Akbulut C, Finsterer U (1998) Extra protein loss not caused by surgical bleeding in patients with ovarian cancer. Acta Anaesthesiol Scand 42:39–46
Rehm M, Haller M, Orth V et al (2001) Changes in blood volume and hematocrit during acute preoperative volume loading with 5 % albumin or 6 % hetastarch solutions in patients before radical hysterectomy. Anesthesiology 95:849–856
Jacob M, Chappell D, Hofmann-Kiefer K, Conzen P, Peter K, Rehm M (2007) Determinants of insensible fluid loss. Perspiration, protein shift and endothelial glycocalyx. Anaesthesist 56(747–58):60–64
Rehm M, Orth VH, Kreimeier U et al (2001) Changes in blood volume during acute normovolemic hemodilution with 5 % albumin or 6 % hydroxyethylstarch and intraoperative retransfusion. Anaesthesist 50:569–579
Rehm M, Orth V, Kreimeier U et al (2000) Changes in intravascular volume during acute normovolemic hemodilution and intraoperative retransfusion in patients with radical hysterectomy. Anesthesiology 92:657–664
Jacob M, Rehm M, Orth V et al (2003) Exact measurement of the volume effect of 6 % hydoxyethyl starch 130/0.4 (Voluven) during acute preoperative normovolemic hemodilution. Anaesthesist 52:896–904
Rehm MHM, Brechtelsbauer H, Akbulut C, Finsterer U (1998) Changes in plasma volume in immediate pre- and postoperative periods in patients major gynecologic surgery. Infusionsther Transfusionsmed 25:222–228
Rehm M, Orth VH, Weninger E et al (2001) Acute “normovolemic” hemodilution with 3.5 % polygel (Haemaccel) for patients in the Wertheim-Meigs-operation. Blood loss of 87 % blood volume without perioperative blood transfusion. Anaesthesist 50:580–584
Jacob M, Chappell D, Hofmann-Kiefer K et al (2012) The intravascular volume effect of Ringer’s lactate is below 20 %: a prospective study in humans. Crit Care 16:R86
Jacob M, Bruegger D, Rehm M et al (2007) The endothelial glycocalyx affords compatibility of Starling’s principle and high cardiac interstitial albumin levels. Cardiovasc Res 73:575–586
Hu X, Adamson RH, Liu B, Curry FE, Weinbaum S (2000) Starling forces that oppose filtration after tissue oncotic pressure is increased. Am J Physiol Heart Circ Physiol 279:H1724–36
Jacob M, Chappell D, Rehm M (2007) Clinical update: Perioperative fluid management. Lancet 369:1984–1986
Bruegger D, Jacob M, Rehm M et al (2005) Atrial natriuretic peptide induces shedding of endothelial glycocalyx in coronary vascular bed of guinea pig hearts. Am J Physiol Heart Circ Physiol 289:H1993–H1999
Bruegger D, Schwartz L, Chappell D et al (2011) Release of atrial natriuretic peptide precedes shedding of the endothelial glycocalyx equally in patients undergoing on- and off-pump coronary artery bypass surgery. Basic Res Cardiol 106:1111–1121
Chappell D, Bruegger D, Potzel J et al (2014) Hypervolemia increases release of atrial natriuretic peptide and shedding of the endothelial glycocalyx. Crit Care 18:538
Wiedermann CJ (2014) Joannidis M Accumulation of hydroxyethyl starch in human and animal tissues: A systematic review. Intensive Care Med 40:160–170
Nieuwdorp M, Meuwese MC, Vink H, Hoekstra JB, Kastelein JJ, Stroes ES (2005) The endothelial glycocalyx: A potential barrier between health and vascular disease. Curr Opin Lipidol 16:507–511
Scheingraber S, Rehm M, Sehmisch C, Finsterer U (1999) Rapid saline infusion produces hyperchloremic acidosis in patients undergoing gynecologic surgery. Anesthesiology 90:1265–1270
Orbegozo Cortes D, Rayo Bonor A, Vincent JL (2014) Isotonic crystalloid solutions: a structured review of the literature. Br J Anaesth 112:968–981
Shaw AD, Bagshaw SM, Goldstein SL et al (2012) Major complications, mortality, and resource utilization after open abdominal surgery: 0.9 % saline compared to Plasma-Lyte. Ann Surg 255:821–829
Young P, Bailey M, Beasley R et al (2015) Effect of a buffered crystalloid solution vs saline on acute kidney injury among patients in the intensive care unit: The SPLIT randomized clinical trial. JAMA 314:1701–1710
Senn A et al (2017) Chloride content of fluids used for large-volume resuscitation is associated with reduced survival. Crit Care Med 45:e146–e153
O’Malley CM, Frumento RJ, Hardy MA et al (2005) A randomized, double-blind comparison of lactated Ringer’s solution and 0.9 % NaCl during renal transplantation. Anesth Analg 100:1518–1524
Potura E, Lindner G, Biesenbach P et al (2015) An acetate-buffered balanced crystalloid versus 0.9 % saline in patients with end-stage renal disease undergoing cadaveric renal transplantation: a prospective randomized controlled trial. Anesth Analg 120:123–129
Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM (2003) Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg 237:319–334
Dubois MJ, Orellana-Jimenez C, Melot C et al (2006) Albumin administration improves organ function in critically ill hypoalbuminemic patients: A prospective, randomized, controlled, pilot study. Crit Care Med 34:2536–2540
Haynes GR, Navickis RJ, Wilkes MM (2003) Albumin administration – what is the evidence of clinical benefit? A systematic review of randomized controlled trials. Eur J Anaesthesiol 20:771–793
Martin GS, Moss M, Wheeler AP, Mealer M, Morris JA, Bernard GR (2005) A randomized, controlled trial of furosemide with or without albumin in hypoproteinemic patients with acute lung injury. Crit Care Med 33:1681–1687
Vincent JL (2009) Relevance of albumin in modern critical care medicine. Best Pract Res Clin Anaesthesiol 23:183–191
Cochrane Injuries Group Albumin Reviewers (1998) Human albumin administration in critically ill patients: Systematic review of randomised controlled trials. BMJ 317:235–240
Investigators SS, Finfer S, Bellomo R et al (2006) Effect of baseline serum albumin concentration on outcome of resuscitation with albumin or saline in patients in intensive care units: analysis of data from the saline versus albumin fluid evaluation (SAFE) study. BMJ 333:1044
Finfer S, Bellomo R, Boyce N et al (2004) A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 350:2247–2256
Caironi P, Tognoni G, Masson S et al (2014) Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 370:1412–1421
Charpentier JJ-PM (2011) Efficacy and tolerance of hyperoncotic albumin administration in septic shock patients: The EARSS study. Intensive Care Med 37:115
Wiedermann CJ, Joannidis M (2014) Albumin replacement in severe sepsis or septic shock. N Engl J Med 371:83
Patel A, Laffan MA, Waheed U, Brett SJ (2014) Randomised trials of human albumin for adults with sepsis: Systematic review and meta-analysis with trial sequential analysis of all-cause mortality. BMJ 349:g4561
Wiedermann CJ, Dunzendorfer S, Gaioni LU, Zaraca F, Joannidis M (2010) Hyperoncotic colloids and acute kidney injury: A meta-analysis of randomized trials. Crit Care 14:R191
Maitland K, Kiguli S, Opoka RO et al (2011) Mortality after fluid bolus in African children with severe infection. N Engl J Med 364:2483–2495
Rehm M, Paptistella M, Dieterich HJ (2012) Volumenersatzlösungen, 3 edn. Springer, Berlin, Heidelberg
Vincent JL, De Backer D, Wiedermann CJ (2016) Fluid management in sepsis: The potential beneficial effects of albumin. J Crit Care 35:161–167
Delaney AP, Dan A, McCaffrey J, Finfer S (2011) The role of albumin as a resuscitation fluid for patients with sepsis: A systematic review and meta-analysis. Crit Care Med 39:386–391
Brunkhorst FM, Engel C, Bloos F et al (2008) Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med 358:125–139
Perner A, Haase N, Guttormsen AB et al (2012) Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med 367:124–134
Myburgh JA, Finfer S, Bellomo R et al (2012) Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med 367:1901–1911
Guidet B, Martinet O, Boulain T et al (2012) Assessment of hemodynamic efficacy and safety of 6 % hydroxyethylstarch 130/0.4 vs. 0.9 % NaCl fluid replacement in patients with severe sepsis: the CRYSTMAS study. Crit Care 16:R94
Dart AB, Mutter TC, Ruth CA, Taback SP (2010) Hydroxyethyl starch (HES) versus other fluid therapies: Effects on kidney function. Cochrane Database Syst Rev. doi:10.1002/14651858
Wiedermann CJ (2008) Systematic review of randomized clinical trials on the use of hydroxyethyl starch for fluid management in sepsis. BMC Emerg Med 8:1
Zarychanski R, Turgeon AF, Fergusson DA et al (2009) Renal outcomes and mortality following hydroxyethyl starch resuscitation of critically ill patients: systematic review and meta-analysis of randomized trials. Open Med 3:e196–209 (ATTENTION: The analysis and conclusions of this article are being revised by the authors. This is due to the journal Anesthesia and Analgesia’s retraction of a paper by Dr. Joachim Boldt, an author in seven of the studies analyzed in this review. As such, the editors of Open Medicine recommend interpreting this review with extreme caution until Zarychanski et al. publish a new analysis and interpretation in Open Medicine. For more information, see Anesthesia and Analgesia’s press release)
Rehm M (2013) Limited applications for hydroxyethyl starch: Background and alternative concepts. Anaesthesist 62:644–655
European Medicines Agency. Assessement report for solutions for infusion containing hydroxyethyl starch. EMA/667553/2013
Meybohm P, Van Aken H, De Gasperi A et al (2013) Re-evaluating currently available data and suggestions for planning randomised controlled studies regarding the use of hydroxyethyl starch in critically ill patients – a multidisciplinary statement. Crit Care 17:R166
Gillies MA, Habicher M, Jhanji S et al (2014) Incidence of postoperative death and acute kidney injury associated with i. v. 6 % hydroxyethyl starch use: systematic review and meta-analysis. Br J Anaesth 112:25–34
Kammerer T, Klug F, Schwarz M et al (2015) Comparison of 6 % hydroxyethyl starch and 5 % albumin for volume replacement therapy in patients undergoing cystectomy (CHART): Study protocol for a randomized controlled trial. Trials 16:384
Rasmussen KC, Secher NH, Pedersen T (2016) Effect of perioperative crystalloid or colloid fluid therapy on hemorrhage, coagulation competence, and outcome: A systematic review and stratified meta-analysis. Medicine (Baltimore) 95:e4498
Moeller C, Fleischmann C, Thomas-Rueddel D et al (2016) How safe is gelatin? A systematic review and meta-analysis of gelatin-containing plasma expanders vs crystalloids and albumin. J Crit Care 35:75–83
Thomas-Rueddel DO, Vlasakov V, Reinhart K et al (2012) Safety of gelatin for volume resuscitation – a systematic review and meta-analysis. Intensive Care Med 38:1134–1142
Perel P, Roberts I (2012) Colloids versus crystalloids for fluid resuscitation in critically ill patients. Cochrane Database Syst Rev. doi:10.1002/14651858
Annane D, Siami S, Jaber S et al (2013) Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: The CRISTAL randomized trial. JAMA 310:1809–1817
Holte K, Sharrock NE, Kehlet H (2002) Pathophysiology and clinical implications of perioperative fluid excess. Br J Anaesth 89:622–632
Mosteller RD (1987) Simplified calculation of body-surface area. N Engl J Med 317:1098
Pearson TC, Guthrie DL, Simpson J et al (1995) Interpretation of measured red cell mass and plasma volume in adults: Expert Panel on Radionuclides of the International Council for Standardization in Haematology. Br J Haematol 89:748–756
Jacob M, Saller T, Chappell D, Rehm M, Welsch U, Becker BF (2013) Physiological levels of A‑, B‑ and C‑type natriuretic peptide shed the endothelial glycocalyx and enhance vascular permeability. Basic Res Cardiol 108:347
Jacob M, Bruegger D, Conzen P, Becker BF, Finsterer U, Rehm M (2005) Development and validation of a mathematical algorithm for quantifying preoperative blood volume by means of the decrease in hematocrit resulting from acute normovolemic hemodilution. Transfusion 45:562–571
Orth VH, Rehm M, Thiel M et al (1998) First clinical implications of perioperative red cell volume measurement with a nonradioactive marker (sodium fluorescein). Anesth Analg 87:1234–1238
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Rehm is currently directing two clinical studies, one of which is supported by CSL Behring and the other of which is supported by Fresenius Kabi. He has received no travel expenses or honoraria from pharmaceutical companies during the past 2 years. N. Hulde, T. Kammerer, A.S. Meidert, and K. Hofmann-Kiefer declare that they have no competing interests.
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Extended and updated version of the article by Hulde N and Rehm M (2016) Grundlagen der Infusionstherapie. In: Refresher Course – Aktuelles Wissen für Anästhesisten, No. 42. Aktiv Druck & Verlag, Ebelsbach, pp. 73–81
Rights and permissions
About this article
Cite this article
Rehm, M., Hulde, N., Kammerer, T. et al. State of the art in fluid and volume therapy. Anaesthesist 68 (Suppl 1), 1–14 (2019). https://doi.org/10.1007/s00101-017-0290-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-017-0290-8