Abstract
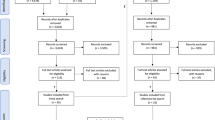
We used three approaches to determine whether first-year medical students would begin to confront their biases in response to a simulated encounter with an incarcerated, African-American patient. The patient presented with fatigue in a Biochemistry course workshop. Two hundred five students watched and helped a classmate conduct a simulated interview with the patient who had been imprisoned for attempted murder. We then studied whether the students confronted their biases against the patient using (a) a survey of individual students regarding these biases, (b) one of a number of questions on a formal assignment concerning the case completed in a team format, and (c) an unprompted extra-credit opportunity to reflect as a team on issues of their choice. On the survey, eighty five percent of students confronted their biases against the patient, and they began to reflect critically about these biases. Critical reflection on teams occurred more frequently outside the formally assigned exercise (Effect Size = 0.75, crucial practical importance). Thus, most first-year medical students can be led, even in basic sciences courses, to confront their biases. In this way, they may also begin to mitigate their biases against patients. Such self-regulation of biases by health care professionals on a regular basis should help to decrease health care disparities.
Similar content being viewed by others
References
Dovidio JF, Fiske ST. Under the radar: how unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. Am J Public Health. 2012;102:945–952.
Penner LA, Albrecht TL, Orom H, Coleman DK, Underwood III W. Health and health care disparities. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. The SAGE handbook of prejudice, stereotyping and discrimination. London, UK: Sage; 2010. p. 472–90.
Smedley BD, Stith AY, Nelson AR. Unequal treatment: confronting racial and ethnic disparities in healthcare. Washington, DC: National Academies Press; 2003.
Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67:478–486.
Rhoads KF, Cullen J, Ngo JV, Wren SM. Racial and ethnic differences in lymph node examination after colon cancer resection do not completely explain disparities in mortality. Cancer. 2012;118:469–477.
VanWinkle LJ, Chandar N, Green JM, Lynch SM, Viselli SM, Burdick P. Does critical reflection by biochemistry learning teams foster patient-centered beliefs among medical students? Med Sci Educator. 2011;21:158–168.
Van Winkle LJ, Robson C, Chandar N, Green JM, Viselli SM, Donovan K. Use of poems written by physicians to elicit critical reflection by students in a medical biochemistry course. Journal for Learning Through the Arts. 2011;7(1). Retrieved from: http://escholarship.org/uc/item/7513c5mv.
Van Winkle L, Dobie S, Ross V, Sharma U, Green J, Lynch S. Acute intervention to foster reflection on reciprocity in relationships increased participants’ patient-or student-centered orientation scores in association with a medical biochemistry course. Internet J Med Educ. 2011;1(2). DOI: 10.5580/11e6.
Van Winkle LJ, Fjortoft N, Hojat M. Impact of a workshop about aging on the empathy scores of pharmacy and medical students. Am J Pharm Educ. 2012;76:9.
Van Winkle L, Bjork BC, Chandar N, Cornell S, Fjortoft N, Green JM, et al. Improvement in pharmacy and medical student physician-pharmacist collaboration scores following a workshop to foster mutual understanding. Am J Pharm Educ. 2012;76:150.
Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–364.
Hojat M, Mangione S, Nasca TJ, Cohen MJM, Gonnella JS, Erdmann JB, et al. The Jefferson scale of physician empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61:349–365.
Hojat M. Empathy in patient care: antecedents, development, measurement, and outcomes. New York: Springer Verlag; 2007.
Neumann M, Edelhauser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86:996–1009.
Nunes P, Williams S, Sa B, Stevenson K. A study of empathy decline in students from five health disciplines during their first year of training. Int J Med Educ. 2011;2:12–17.
Williams B, Boyle M, Brightwell R, Devenish S, Hartley P, McCall M, et al. An assessment of undergraduate paramedic students’ empathy levels. Int J Med Educ. 2012;3:98–102.
Godlaski TM, Butler L, Heron M, Debord S, Cauvin L. A qualitative exploration of engagement among rural women entering substance user treatment. Subst Use Misuse. 2009;44:62–83.
Hojat M, Gonnella JS, Mangione S, Nasca TJ, Veloski JJ, Erdmann JB, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36:522–527.
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloksi JJ, Magee M. The Jefferson scale of physician empathy: further psychometric data and differences by gender and specialty at item level. Acad Med. 2002;77(10 Suppl):S58–S60.
Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–1569.
Hojat M, Mangione S, Nasca TJ, Gonnella JS, Magee M. Empathy scores in medical school and ratings of empathic behavior in residency training 3 years later. J Soc Pychol. 2005;145:663–672.
Skloot R. The immortal life of Henrietta Lacks. New York: Random House; 2010.
Hojat M, Xu G. A visitor’s guide to effect sizes: statistical significance versus practical (clinical) importance of research findings. Adv Health Sci Educ. 2004;9: 241–249.
Rosenthal R, Rubin DB. A simple, general purpose display of magnitude of experimental effect. J Educ Psych. 1982;74: 166–169.
Lonie JM, Alemam R, Dhing C, Mihm D. Assessing pharmacy student self-reported empathic tendencies. Am J Pharm Educ. 2005;69: 29.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Van Winkle, L.J., La Salle, S., Richardson, L. et al. Challenging Medical Students to Confront their Biases: A Case Study Simulation Approach. Med.Sci.Educ. 23, 217–224 (2013). https://doi.org/10.1007/BF03341624
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03341624