Abstract
Virtual Touch™ Quantification (VTq) is a software application used with Siemens Acuson ultrasound scanners to assess the stiffness of liver tissue. The National Institute for Health and Care Excellence (NICE) Medical Technologies Advisory Committee (MTAC) selected VTq for evaluation and invited the company to submit clinical and economic evidence. King’s Technology Evaluation Centre, an External Assessment Centre (EAC) commissioned by NICE, independently assessed the evidence submitted. The EAC conducted its own systematic review, meta-analysis and economic analysis to supplement the company’s submitted evidence. The meta-analyses comparing VTq and transient elastography (TE) with liver biopsy (LB) provided pooled estimates of liver stiffness and stage of fibrosis for the study populations (hepatitis B, hepatitis C or combined populations). When comparing significant fibrosis (Metavir score F ≥ 2) for both hepatitis B and C, VTq had slightly higher values for both sensitivity and specificity (77 and 81 %) than TE (76 and 71 %). The overall prevalence of cirrhosis (F4, combined populations) was similar with VTq and TE (23 vs. 23 %), and significant fibrosis (F ≥ 2) was lower for VTq than for TE (55 vs. 62 %). The EAC revised the company’s de novo cost model, which resulted in a cost saving of £53 (against TE) and £434 (against LB). Following public consultation, taking into account submitted comments, NICE Medical Technology Guidance MTG27 was published in September 2015. This recommended the adoption of the VTq software to diagnose and monitor liver fibrosis in patients with hepatitis B or hepatitis C.
Similar content being viewed by others
Virtual Touch™ Quantification (VTq) is a software application used with Siemens Acuson ultrasound scanners to assess the stiffness of liver tissue and the stage of liver fibrosis. |
The National Institute for Health and Care Excellence Medical Technology Evaluation Programme assessed the VTq software for use in people with hepatitis B or C and the External Assessment Centre estimated cost savings per patient for the VTq software in hepatitis patients was £53 when compared to transient elastography and £434 when compared to liver biopsy. |
In September 2015, the VTq software was recommended for adoption within the National Health Service (NHS) for patients with hepatitis B or C for diagnosis and monitoring of liver fibrosis. |
1 Introduction
The role of the National Institute for Health and Care Excellence (NICE) is to provide guidance and advice to improve health and social care in England. Evaluating new or innovative medical technologies for adoption in the National Health Service (NHS) in England is part of this role. These evaluations are undertaken by the NICE Medical Technologies Evaluation Programme (MTEP).
In order for technologies to be eligible for evaluation they must be new or innovative, have a current CE mark or equivalent regulatory approval (or be expecting one within 12 months) and be suitable for eventual NICE guidance within the definitions of a medical or diagnostic technology. The process and methods for topic selection and guidance development are described further in the MTEP process and method guides [1]. Guidance is produced by the Medical Technologies Advisory Committee (MTAC) after clinical and cost evidence submitted by the manufacturer is independently assessed by an External Assessment Centre (EAC), and following consideration of comments received during public consultation on the draft recommendations. Throughout the evaluation process, input from patient organisations and independent expert advisers is considered.
Virtual Touch™ Quantification (VTq) is a software application used with either the Acuson S2000™ or the Acuson S3000™ ultrasound scanner (Siemens Healthcare, Erlangen, Germany) to assess the stiffness of liver tissue. In September 2015, NICE issued final guidance (MTG27) on this technology specifically in relation to liver fibrosis in patients with chronic hepatitis B or hepatitis C [2]. This article presents a summary of the EAC report and its contribution to the NICE guidance on the use of VTq as part of a series of NICE Medical Technology Guidance summaries published in Applied Health Economics and Health Policy.
2 Decision Problem
2.1 Disease Overview
Viral hepatitis in humans is characterised by inflammation and damage to the liver such as liver fibrosis, cirrhosis and hepatocellular carcinoma. Worldwide, viral hepatitis is considered to be a major public health issue as it is the cause of significant morbidity and mortality. There are several types of viral hepatitis: hepatitis A, hepatitis B, hepatitis C, hepatitis D and hepatitis E. Symptoms of hepatitis vary; they may include (but are not limited to) abdominal pain, fever, joint pain, loss of appetite, yellowing of skin and eyes (jaundice), and nausea/vomiting.
Hepatitis B and C are of particular interest for this current MTEP technology evaluation. Hepatitis B (International Statistical Classification of Diseases and Related Health Problems, 10th edition [ICD-10] classification: B17.0, B16.0, B16.1, B16.9) causes acute and chronic hepatitis and is largely transmitted through exposure to infected body fluids such as blood through sexual activity, unsanitary conditions or breastfeeding. There is a vaccine available that provides lifetime protection. Worldwide, it is estimated that chronic infection with hepatitis B affects 400 million people [3], whilst the British Liver Trust estimates that 1 in 350 people in the UK have chronic hepatitis B [4].
Hepatitis C (ICD-10: B17.1, B18.2) is usually contracted through exposure to infected blood and through the placenta during pregnancy. It can remain asymptomatic for several years, and when symptoms do occur, they are similar to the symptoms of influenza. Infection with hepatitis C can lead to chronic hepatitis, resulting in fibrosis (stiffening of the liver) and cirrhosis of the liver. The World Health Organization estimate that 130–150 million people have hepatitis C globally [5] and there is currently no vaccine available. It is estimated that 215,000 people in the UK have hepatitis C [6] and that 50 % of those people are undiagnosed [7].
2.2 Risk Assessment and Current Treatment Options
The NICE guideline on chronic hepatitis B diagnosis and management recommends that people with hepatitis B are assessed in primary care and refers to special consideration for patients who are pregnant or have decompensated liver disease and for paediatric patients [8]. In secondary specialist care, it is recommended that all hepatitis B patients be assessed for liver disease using non-invasive tests such as transient elastography (TE) and/or genotype testing, and, where deemed necessary/appropriate, they are offered a liver biopsy (LB) to determine the level of fibrosis and/or antiviral treatment. Recommendations for regular surveillance and monitoring of liver disease are outlined in the guidance, along with specific reference to particular patient subgroup management.
NICE guidelines for hepatitis C are currently being developed and will be published in September 2016 (https://www.nice.org.uk/guidance/indevelopment/gid-cgwave0666). Draft guidance in the interim period recommends three different treatment options for patients with chronic hepatitis C depending on genotype, liver disease stage and fibrosis stage: daclatasvir, ledipasvir–sofosbuvir and ombitasvir–partaprevir–ritonavir with or without dasabuvir [7].
2.3 Virtual Touch™ Quantification (VTq)
VTq is a software application (implementation of acoustic radiation force impulse [ARFI] technology) used with either the Acuson S2000™ or the Acuson S3000™ ultrasound scanners (Siemens Healthcare) to assess the stiffness (elasticity) of liver tissue. More specifically, ARFI works by measuring shear wave speed in the liver using an ultrasound machine, and is usually performed by a sonographer, radiologist or hepatologist. VTq assessment requires multiple measurements, adding 5–10 min to a routine abdominal ultrasound examination, and the company describes it as a non-invasive and pain-free application. VTq software reports a statistical summary of both the median and mean shear wave velocities, and reliability can be confirmed by calculating a “ratio of the inter-quartile range to median, which should be less than 0.30” [9].
This assessment report focuses specifically on the use of VTq in patients with chronic hepatitis B or hepatitis C. The company provided three CE declarations of conformity; the Acuson S3000™ declaration of conformity was dated November 2012. Both ultrasound devices were classified as Class IIa medical devices.
2.4 NICE Scope
The final scope for the evaluation of VTq to diagnose and monitor liver fibrosis was developed by NICE in consultation with stakeholders and published in May 2014. The scope defined the patient population as “adults or children with chronic hepatitis B or C in whom assessment of liver fibrosis is indicated” [10]. The comparators were TE (also referred to as Fibroscan) (http://www.myliverexam.com/en/lexamen-fibroscan.html) and the index test of LB. The intervention was the VTq software application to be “used with the Siemens Virtual Touch Tissue Imaging systems (the Acuson S2000 or S3000 ultrasound platforms)” [10]. The outcome measures specified were correlation in assessment of stage of liver disease, sensitivity and specificity (using area under the receiver operating characteristic [AUROC], a summary statistic) in assessment of liver fibrosis, correlation in assessment of stage of fibrosis using Metavir score (a scoring system for assessing liver inflammation and fibrosis of the liver), use of antiviral drugs, quality-of-life measures, hospital bed usage and length of stay, the requirement for LB, and device-related adverse events. The Metavir scoring system provides a validated classification system for development of fibrosis: F0 = no fibrosis; F1 = portal fibrosis without septa; F2 = portal fibrosis with rare septa; F3 = numerous septa without cirrhosis; and F4 = cirrhosis.
The scope requested that both comparators (TE and LB) be included in the cost analysis, depending on “whether either or both of these represent standard care in the relevant patient population” [10] and that both primary and secondary care settings be considered. The model for the cost analysis was also to consider scenarios where a compatible Siemens ultrasound machine is and is not available. The scope did not specify any subgroups or special considerations to be considered which related to equality issues.
3 EAC Review
The company’s submission consisted of clinical and economic evidence. The clinical section provided an overview and systematic review of clinical evidence related to VTq and the comparators of TE and LB. The company found no economic evidence relating to VTq, and instead submitted a de novo cost model. King’s Technology Evaluation Centre (KiTEC), an EAC based in the King’s Health Partners Academic Health Science Centre (KHP), was commissioned by NICE to critique the manufacturer’s submission and provide further evidence if available.
3.1 Clinical Effectiveness Evidence
The company submitted clinical evidence and a search strategy relating to the use of VTq with either the Acuson S2000™ or Acuson S3000™ ultrasound scanners to assess the stiffness of liver tissue.
Clinical evidence was provided on the intended intervention and both comparators specified in the scope. The company provided clinical evidence based on 23 studies (a combination of conference abstracts and full publications) [11–31]. On further evaluation, the company refined this evidence to 11 studies for full review, as the other 12 studies “did not contain sufficient information to complete the inclusion assessment” [9]. Of the 11 publications that the company did include for further evaluation, ten were case-control observational studies [20, 23–27, 29, 32–34] and one was a meta-analysis [22].
The company stated that they had not been made aware of any ongoing studies. However, the EAC performed a search of the clinical trials database (ClinicalTrials.gov) using the terms ‘ARFI’, ‘VTq’, ‘Virtual Touch tissue quantification’ and ‘Acoustic Radiation Force Impulse’ and identified three clinical trials that it considered potentially relevant [35–37]. The EAC noted that one of these clinical trials is being conducted in a paediatric population, with an estimated trial completion date of November 2015 [37]. However, additional data for this age group are only likely to become available within the next 1–2 years.
3.1.1 Critique of Clinical Effectiveness Evidence
The EAC considered that the company included some of the relevant evidence on VTq and both comparators and that the company’s interpretation of the available clinical evidence was reasonable and provided a fair assessment of the studies submitted. Of the 11 studies provided by the company, all fitted the required scope in terms of comparators and outcome measures. The majority of these publications (mainly conference abstracts) provided limited study details, such as baseline characteristics of patients (e.g. ethnicity) and study design.
The EAC had several concerns relating to the effectiveness of the company’s study selection: for example, although the search terms and time limits used by the company were appropriate for the technology, a large proportion of the published studies included overlapping cohorts. Identifying which studies used independent groups of patients is challenging and this was noted in the company’s submission and during the clinical evidence submission discussion teleconference held on 30 June 2014.
Of these 11 company-included studies, eight were subsequently excluded by the EAC as their patient cohorts overlapped with those of the three studies subsequently accepted by the EAC [32–34] (Table 1).
The company reported no adverse events in the submission, and the EAC also did not identify any adverse events reported in the literature. Expert advisers were asked if they had any knowledge of adverse events that had occurred previously or could potentially occur in the future. No expert adviser responded with any known adverse events related to this technology.
3.1.2 Additional EAC Clinical Effectiveness Evidence
The EAC noted that there were minor discrepancies in the description of the company’s systematic review methodology, such as incomplete search strategy terms. Clarification was sought from the company, who responded with the correct search terminology. The EAC replicated the company’s search strategy but concluded that it lacked some important search terms. Therefore, the EAC conducted a revised systematic review with additional search terms related to outcomes as defined in the scope and to ensure all available evidence had been considered (see Appendices 1, 2).
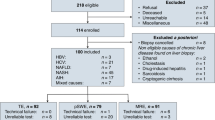
A total of 49 studies were selected for full paper review, of which 39 were rejected. Of the ten studies that the EAC’s systematic review identified as relevant in terms of the scope, three were also identified in the company’s own systematic review: Friedrich-Rust et al. [32, 33] and Sporea et al. [34]. The findings of the remaining seven EAC-accepted papers and an overview of each study are presented in Table 2. It is noted here that two of the studies [38, 39] were previously identified by the company but were not included in their final selection. Appendix 3 shows a PRISMA flow diagram including both the company’s and the EAC’s search strategies.
3.1.3 EAC Meta-Analyses
All EAC-accepted studies were reviewed and, where appropriate, population outcome data were extracted in order to conduct meta-analyses. Where actual frequencies were not reported in full in the papers they were calculated using available study summary data (sensitivity, specificity, totals). Random effects meta-analyses were used to calculate all pooled proportions for correlation, sensitivity, specificity and prevalence. Prior to analysis proportions were transformed using the logit function (log[p/(1 − p)]) as in most cases they were either close to 0 or close to 100 % and so skewed. For positive skewness (log[p/(1 − p)]) was used, for negative skewness (log[(1 − p)/p]) was used. For sets of proportions that had a wide range, no transformation was used prior to pooling. Numerator values of 0 (in specificity) were replaced with 0.5 to permit pooling. Results of meta-analyses were back-transformed to the natural scale as appropriate. All analyses were conducted using STATA® v11.0 (STATA Corp. LP, College Station, TX, USA). The ‘metan’ procedure was used for the random effects meta-analyses.
Pooled values were calculated for each study population (i.e. hepatitis B, hepatitis C and combined) and then for the liver fibrosis comparator (i.e. VTq and TE) to LB for all liver fibrosis stages (where available). In cases where only a single study was available, the appropriate proportion and 95 % confidence interval (CI) were calculated. In all, nine outcome estimates were calculated with 95 % CIs for prevalence, sensitivity and specificity (Table 3). Six further estimates are given using single study data.
Correlation values were pooled for nine studies (Table 3). Most papers reported Spearman’s rank correlation (rho), but Yamada et al. [39] used Pearson’s correlation coefficient (r). In order to provide a pooled correlation for the Spearman’s rho, the large sample approximation for the variance of rho was calculated as 1/(N − 1), where N is the total number of subjects from whom the correlation was calculated. Since it is not possible to pool values of rho and r, Yamada et al.’s value was considered to be a Spearman’s rho coefficient for meta-analysis. Sensitivity analysis without Yamada et al.’s study made virtually no difference to pooled estimates and so the pooled values including Yamada et al. [39] are reported. The 95 % CIs are only provided where the number of values to be combined is sufficient to give a stable estimate.
The meta-analyses provided estimates with 95 % CIs for prevalence, sensitivity and specificity (Table 4). In all, nine pooled outcome estimates were calculated for significant fibrosis (F ≥ 2) and both hepatitis B and C were lower with VTq (55 %) than TE (62 %); however, the techniques had similar scores for cirrhosis (F4): VTq, 23 % and TE, 23 %. The results for specificity in all subgroups ranged from 71 to 87 %, while for sensitivity the values ranged more widely, from 70 to 93 %. The range of values for both sensitivity and specificity were similar for both the hepatitis B and hepatitis C study populations. When comparing significant fibrosis (F ≥ 2) for both hepatitis B and C, VTq had slightly higher values for both sensitivity and specificity (77 and 81 %) than TE (76 and 71 %). Sensitivity values were higher than specificity for cirrhosis (F4) in the combined study population for VTq (85 and 80 %), whilst the opposite was found for TE (79 and 84 %). However, the values were similar for both VTq and TE.
The meta-analyses of correlation coefficients for VTq and TE gave pooled estimates ranging from 0.63 to 0.69 (Table 5). The combined study population correlation coefficients for VTq and TE were similar (0.68 and 0.69, respectively).
As expected, prevalence rates generally decreased with increasing liver fibrosis stage. Overall prevalence for both VTq and TE (combined study populations) had similar rates for cirrhosis (F4) (0.23 vs. 0.23) and a lower prevalence for significant fibrosis (F ≥ 2) for VTq when compared with TE (0.55 vs. 0.62). Pooled estimates (combined study populations) for correlation were similar for VTq and TE, whilst the pooled estimates for sensitivity for significant fibrosis (F ≥ 2) and cirrhosis (F4) were higher for VTq than for TE. Specificity values for significant fibrosis (F ≥ 2) were notably higher for VTq than TE (81 vs. 71 %), but were closer for cirrhosis (F4) (80 vs. 84 %).
The EAC notes that caution must be observed when interpreting the results from the meta-analyses as no adjustment was possible for confounding variables such as patient characteristics, other than hepatitis type, research design and research settings (such as country).
3.2 Economic Evidence
The company submitted details of the search strategy designed to retrieve relevant health economics studies from published and unpublished literature from 2009 to 2014. They concluded that no economic evidence was available for VTq and hence submitted a de novo cost model. The company provided a decision-tree model using 2013 prices from the UK NHS and personal social services perspective to estimate the cost for VTq and the comparators. The time horizon for the model was 1 year. The company’s modelling approach was based on a 2009 economic report from the Centre for Evidence-based Purchasing [45]. However, this report does not include the distribution of different stages of liver fibrosis (i.e. F1–F4 using the Metavir score). Therefore, this model would not fully capture the decision problem stated in the scope issued by NICE. In order to mitigate this issue, the company submitted a revised model using a sequential distribution of liver fibrosis stage (according to Metavir score). This is achieved by sequentially separating the overall prevalence of liver fibrosis in three stage groups: (1) F ≥ 2; (2) F ≥ 3; and (3) F4. The modelling was developed using two parameters: (1) estimated prevalence of liver fibrosis for different stages; and (2) the sensitivity/specificity of each strategy (i.e. VTq and the comparators [TE and LB]) at different liver fibrosis stages. Based on these parameters, all patients were categorised as (1) true positive; (2) true negative; (3) false positive; or (4) false negative.
Prevalence estimates were based on expert opinion provided by four clinicians who had familiarity with VTq and Fibroscan. The diagnostic accuracy for TE was based on a published meta-analysis [46]. LB was assumed to have perfect (i.e. 100 %) sensitivity and specificity, as it is the reference test for diagnosing liver fibrosis. The sensitivity and specificity of VTq for different stages of liver fibrosis were estimated as an average from different published studies, i.e. not from a meta-analysis [22, 24, 25, 27, 29, 30, 39, 44, 47–51].
The company had undertaken and presented a bottom-up approach for costing the technology (VTq; £15.02 per scan) and one of the comparators (TE; £25.33 per scan), as there were no specific tariffs that accurately reflect differences in resource use. The biopsy unit cost (£615 per LB) was estimated from the 2013 to 2014 payment by results (PbR) tariff. The company performed several deterministic one-way and multi-way sensitivity analyses, varying the prevalence of liver fibrosis, VTq’s diagnostic accuracy, specific costs (e.g. unit cost per VTq examination) and biopsy utilisation after initial diagnostic ultrasound.
The company reported a cost saving of £10.31 per patient by using VTq compared with TE. In comparison with LB, the company reported that VTq leads to a cost savings of around £599.08 per patient. The sensitivity analysis also confirmed the cost-savings conclusions.
3.2.1 Critique of Economic Evidence
The EAC reviewed the company’s search strategy and the databases included and concluded that it could be improved in terms of the date limits (2000–2014) and the search. The EAC therefore undertook a new search for economic evidence, but they did not find any new evidence on the technology.
The EAC considered that the model addressed the decision problem in the scope, but that the structure did not accurately reflect current clinical pathways for people with liver fibrosis. Furthermore, it did not include all the relevant costs and outcomes for diagnosing and treating the condition. No monitoring or treatment costs were included for people in the F ≥ 2, F3 or F4 fibrosis groups. The EAC concluded that this was erroneous, as people with less severe fibrosis may benefit from treatment.
The EAC also questioned the assumption that people falsely classified as negative for fibrosis would not incur any treatment costs and would re-enter the model as new patients. It was determined that this was a misleading approach as misdiagnosis may incur additional costs (from further diagnostic tests, inpatient or emergency episodes and treatment). The EAC considered that a mortality arm would have been useful to account for the small increased risk associated with LB, but acknowledged that this was likely to have been incorporated in the chosen tariff cost. The EAC noted that the company used a cohort approach rather than a per-patient approach as specified in NICE’s methodology. In order to address these issues, the EAC revised some of the parameters and re-ran the company’s model (described further in Sect. 3.2.2).
3.2.2 Additional EAC Economic Evidence
The EAC revised some parameters and re-ran the company’s model to address the issues mentioned in Sect. 3.2.1, including treatment and monitoring costs for people diagnosed with less severe fibrosis (F < 2), those initially classed as false negative and a mortality arm. The revised model was a sequential decision tree incorporating outcomes for F ≥ 2, F ≥ 3 and F4 fibrosis using VTq, TE and LB over a 1-year time horizon for adults or children with chronic hepatitis B or C. Each stage included true positives, false positives, true negatives and false negatives. Revised prevalence and diagnostic accuracy parameters for the model were taken mainly from the EAC’s meta-analyses and applied at each sequential stage for VTq, TE and LB.
As in the company’s model, LB was treated as the reference standard with 100 % sensitivity and specificity [9]. The EAC made several assumptions for the model (see Appendix 4). The unit costs for VTq and TE were estimated using an annuity method and discounted at 3 %, to give a per-test figure of £15.24 for VTq and £25.90 for TE. The cost for LB was estimated from NHS reference costs to be £622 (weighted average of NHS reference codes GB04D and GB04E) [52]. The costs for antiviral therapy were taken as £2808 for those at stage F3 and £5680 for those at stage F4, based on duration of treatment with peginterferon-alfa and ribavirin [53].
Results from the revised base case are shown in Table 6. In a scenario where a compatible Siemens ultrasound machine would need to be purchased along with the VTq software, using VTq would generate cost savings of £53 per person compared with TE and £434 compared with LB. If a compatible ultrasound machine was already available, the cost savings for VTq increased slightly to £57 compared with TE and £438 compared with LB.
The EAC carried out deterministic sensitivity analyses, varying prevalence rates, sensitivity and specificity for VTq and TE, distribution of false positives between stages F2 and F3, unit costs of VTq and TE, usage levels of TE and antiviral therapy costs. Findings from the sensitivity analyses showed that VTq remained cost saving across all scenarios. The key drivers affecting the cost savings per person were prevalence of liver fibrosis, the distribution of false positives to other fibrosis stages, the specificity of VTq and TE for stages F ≥ 2 and F ≥ 3, unit costs of VTq and TE, and antiviral treatment costs.
3.3 Conclusion of the EAC
The EAC considered that the systematic review provided by the company was comprehensive and that the interpretation of the evidence was reasonable; however, they considered that many of the studies included by the company had overlapping cohorts and should have been excluded from the review. From the initial 11 studies that the company included, the EAC agreed with the inclusion of three studies: two with a population of people with hepatitis C [33, 34] and one with a population of people with hepatitis B [32]. Many studies were excluded by the EAC as the population included was mixed or included groups not specified in the scope, thus substantially reducing the available evidence submitted by the company.
To ensure that all available evidence had been identified, the EAC repeated the systematic review and performed a meta-analysis. The EAC’s systematic review identified ten studies, which included the three identified by the company, two that had been previously excluded by the company and five additional studies. The meta-analyses of the comparators (VTq and TE) to LB filled gaps in the evidence base by providing additional pooled outcome estimates with 95 % CIs.
As expected, prevalence rates generally decreased with increasing liver fibrosis stage. Overall prevalence for both VTq and TE (combined study populations) had similar rates for cirrhosis (F4) (0.23 vs. 0.23) and a lower prevalence for significant fibrosis (F ≥ 2) for VTq than for TE (0.55 vs. 0.62). Pooled estimates (combined study populations) for correlation were similar for VTq and TE, whilst the pooled estimates for sensitivity for significant fibrosis (F ≥ 2) and cirrhosis (F4) were higher for VTq than for TE. Specificity values for significant fibrosis (F ≥ 2) were notably higher for VTq than for TE (81 vs. 71 %), but were closer for cirrhosis (F4) (80 vs. 84 %).
The EAC sequentially remodelled the costs for the technology and comparators using prevalence, sensitivity, specificity, test costs and antiviral treatment cost; they found that the technology (VTq) offers cost savings when compared to TE and LB. The cost saving against LB was much larger than when compared to TE. Sensitivity analysis of the key variables also did not alter the conclusion that the VTq technology is cost saving. The EAC acknowledged some limitations of its revised parameters. Due to the lack of clear data available on prevalence and diagnostic accuracy at each stage of fibrosis, figures were extrapolated for the stages in a sequential model rather than each stage being presented separately. Figures for hepatitis C at stage F ≥ 3 fibrosis were applied to the whole population because combined data were not available.
4 NICE Guidance
In accordance with NICE’s MTEP process, draft recommendations for the adoption of the VTq device were produced based on discussion by MTAC, the EAC report and input from expert advisors. The draft recommendations were subject to public consultation and MTAC considered all submitted comments before developing final guidance.
4.1 Preliminary Guidance
In November 2014, MTAC met and reviewed both the company’s submission and the EAC report, along with input from expert advisers. Based on this meeting, MTAC concluded “that the case for adopting Virtual Touch Quantification (VTq) software to diagnose and monitor liver fibrosis is supported by the evidence” [2]. MTAC provisionally recommended the use of VTq in “adults and children with chronic hepatitis B or C who need assessment of liver fibrosis”.
4.2 Consultation Response
Public comment was invited on the draft recommendations between 17 December 2014 and 19 January 2015. During this period, detailed comments (n = 31) were received from nine consultees: two companies, one EAC (KiTEC), the Department of Health, two patient organisations, two Guideline Development Groups and one professional society [2]. The EAC, in collaboration with the MTEP team, prepared draft responses to all comments and presented them to MTAC for consideration in its final guidance meeting. During this meeting the consultation comments were discussed at length with expert advisers and EAC representatives.
The detailed consultation comments covered several areas of concern related to the use of VTq for the assessment of liver fibrosis. Several comments related to the use of VTq in patients with a high body mass index (BMI). The EAC responded by clarifying that the currently available evidence is unclear, with some studies suggesting that BMI has no interrelation with measurements of VTq or indeed TE, whilst other studies suggest that it does. Furthermore, the EAC was unable to adjust for BMI in the meta-analyses due to the lack of detailed and comparable data.
Disease progression and monitoring was another topic raised within the consultation process, with the suggestion that as disease progression for hepatitis B and hepatitis C is different this may influence the results for VTq. None of the accepted clinical or economic evidence assessed monitoring or disease progression. However, Yamada et al. [39] did investigate the ability of VTq to predict response to antiviral therapy based on hepatitis genotype. They found that VTq could not predict response with genotype 2 hepatitis C but could with genotype 1 hepatitis C.
The potential use of VTq in paediatric patient populations attracted comment. It was suggested that there were likely benefits of VTq for children since more invasive techniques such as LB could be avoided. The EAC identified two published studies that included a paediatric population, but these were subsequently excluded due to mixed patient cohorts. Both were pilot studies and concluded that VTq showed promise in non-invasive staging of liver fibrosis in children [54, 55]. As described in Sect. 3.1, the EAC also identified an ongoing clinical trial with a paediatric population in Canada [37]. Although the results of the trial are not yet available, the study consists of children with hepatitis B, hepatitis C or non-alcoholic fatty liver disease, and it is evaluating the safety/efficacy of TE, VTq and magnetic resonance imaging.
Concern was raised regarding the impact of hepatic inflammation on liver elasticity and associated VTq readings. Of the evidence included by the EAC, only two papers assessed inflammation (note that inflammation was outside the NICE scope for VTq). Nishikawa et al. [42] compared VTq and LB in diagnosed chronic hepatitis C patients in Japan, and concluded that there was no correlation between ARFI and inflammation when patients with different fibrosis stages were analysed separately using multivariate regression analysis. In contrast, in their study of hepatitis C patients in Taiwan, Chen et al. [40] found evidence that inflammation significantly affects the measurement of liver fibrosis using VTq. New evidence provided to the EAC assessed ARFI/VTq/histological variance amongst patients referred for a LB [56]. The unadjusted univariate analysis found no significant difference in ARFI/histological variance between non-viral and viral patients; however, the EAC notes that interpretation of this abstract is limited given the lack of subgroup analysis and detailed study information. MTAC considered this additional evidence in determining its final guidance.
The issues of inter-operator and intra-observer variability were raised throughout the consultation process. Although this was outside the NICE scope for VTq, the EAC reviewed the available evidence. Rizzo et al. [43] performed a range of analyses which included inter-observer agreement. The Bland-Altman method was used to assess agreement of ARFI performed by two different sonographers for 21 patients. There was no significant difference between VTq values, indicating good agreement. Chen et al. [40] assessed intra-observer correlations of ARFI liver stiffness measurements (LSM) using an intra-class correlation coefficient (ICC). Independent LSMs were performed on two separate occasions in 20 patients. The same hepatologist was involved on both occasions, and the study found statistically significant agreement/consensus. The EAC concluded that these two studies provide reasonable evidence for acceptable agreement/consensus between the observers when assessing VTq/ARFI measurements.
Expert advisers were approached for an opinion on the generalisability of the research, conducted in other European and Asian countries, to the UK population, and regarding whether there were likely to be differences in the overall VTq measurements between ethnic groups. Three experts responded: the first expert adviser commented that obesity, which may be less prevalent in some Asian countries, can cause the VTq technique to fail more often and may cause the results to be more variable. Another expert adviser remarked that the German and Romanian studies may not be applicable to a UK population as the UK population with hepatitis B and hepatitis C is a worldwide, rather than a European, population. The final expert advisor commented that they consider that the study populations would be applicable to the UK as long as they are corrected for age, BMI and other factors. These factors, which would be applicable to TE as well as VTq, could not be accounted for in the EAC’s meta-analysis using the current available clinical evidence. In light of this, the EAC considers that a study using a UK population to compare VTq, TE and LB would be beneficial, and should appropriately allow for such confounding factors, potentially through suitable subgroup analysis.
4.3 Final Guidance
An MTAC meeting was held on 19 February 2015 to produce the final medical technology guidance for the use of VTq to diagnose and monitor liver fibrosis in chronic hepatitis B and C (MTG27), which was published by NICE in September 2015 [2], and included the following recommendations.
-
1.
The case for adopting VTq software to diagnose and monitor liver fibrosis is supported by the evidence. VTq is as accurate as TE in diagnosing and staging liver fibrosis, and may offer other benefits in terms of imaging the liver and sampling selected areas to assess fibrosis and identify associated pathologies. By avoiding liver biopsies, it may also benefit people whose liver fibrosis needs monitoring. Cost savings through adopting VTq will be greater in hospitals in which LB is the primary method for diagnosing and monitoring liver fibrosis.
-
2.
VTq should be considered as an option for people with chronic hepatitis B or C who need assessment of liver fibrosis.
-
3.
Cost modelling suggests that using VTq is cost saving compared with TE and LB, whether or not a compatible Siemens ultrasound machine needs to be purchased. Compared with TE, the estimated overall cost saving for VTq is around £53 per person. This saving assumes that 10 % of the ultrasound machine capacity would be used for VTq measurements, leaving 90 % to be applied to other uses. Compared with LB, the corresponding saving is around £434 per person.
5 Challenges
During the course of reviewing the clinical evidence for VTq, the EAC encountered several challenges. The limited availability of clinical evidence for the use of VTq in hepatitis B and C patients was one of the main challenges. Many of the studies identified had overlapping patient populations, which is why the EAC subsequently rejected many of the studies included by the company. The company’s systematic review did not adequately reflect the scope specified by NICE; therefore, the EAC repeated this step. The EAC’s systematic review identified ten studies, which included the three identified by the company, two that had been previously excluded by the company and five additional studies.
Meta-analyses of the comparators (VTq and TE) for LB was carried out by the EAC to fill the gaps in the evidence base by providing additional pooled outcome estimates with 95 % CIs. The pooled estimates of prevalence, sensitivity and specificity were the parameters required for the economic modelling and pooled estimates for correlation were also provided. The meta-analysis provided pooled estimates for the various study populations (hepatitis B, hepatitis C and combined study populations) and for liver fibrosis stage. Not all liver fibrosis stages could be included in the meta-analyses; however, pooled estimates were available for all F ≥ 2 and F4 subgroups.
Since no economic evidence was available for the VTq technology, the company submitted a de novo cost model. The EAC considered that the proposed model generally addressed the scope issued by NICE, but nonetheless had important issues that needed to be considered. In particular, the model structure proposed by the company neither reflected the clinical pathway for patients with fibrosis (both the current pathways with TE and LB and the proposed pathway with VTq) nor took into account all relevant costs and outcomes for diagnosing and treating liver fibrosis. On this basis, the EAC considered it necessary to revise the company’s model, which resulted in a cost saving of £53 (against TE) and £434 (against LB).
In summary, there are several challenges in assessing medical technology arising from limitations in the available evidence. Specifically, for VTq, it was fortunate that sufficient evidence was available during the MTAC process to enable meta-analysis and more precise economic modelling. This evaluation has added to the evidence for the use of VTq in the assessment and monitoring of liver fibrosis in hepatitis B and hepatitis C patients in the UK.
References
National Institute for Health and Care Excellence. NICE medical technologies evaluation programme. 2015. https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-medical-technologies-evaluation-programme. Accessed 1 Jun 2016.
National Institute for Health and Care Excellence. Virutal Touch Quantification to diagnose and monitor liver fibrosis in chronic hepatitis B and C: Medical Technology Guidance (MTG27). 2015. https://www.nice.org.uk/guidance/mtg27/. Accessed 1 Jun 2016.
Dhillon R, Parakevopoulu M. Hepatitis B and C. J Intensive Care Soc. 2014;15(2):135–41.
Foster G, Campbell L. Hepatitis B. 2012. http://www.britishlivertrust.org.uk/liver-information/liver-conditions/hepatitis-b/. Accessed 1 Jun 2016.
World Health Organization. Hepatitis C. Fact sheet. 2015. http://www.who.int/mediacentre/factsheets/fs164/en/. Accessed 1 Jun 2016.
NHS Choices. Hepatitis C. 2015. http://www.nhs.uk/conditions/Hepatitis-C/Pages/Introduction.aspx. Accessed 1 Jun 2016.
National Institute for Health and Care Excellence. NICE recommends three new treatment options for hepatitis C in draft guidance. 2015. https://www.nice.org.uk/news/press-and-media/nice-recommends-new-treatment-options-for-hepatitis-c. Accessed 1 Jun 2016.
National Institute for Health and Care Excellence. Hepatits B (chronic): diagnosis and management: NICE Guidelines [CG165]. 2013. https://www.nice.org.uk/guidance/cg165. Accessed 1 Jun 2016.
Siemens. Virtual Touch Quantification to diagnose and monitor liver fibrosis: Company submission of evidence for NICE Medical Technologies Evaluation Programme. 2014.
National Institute for Health and Care Excellence. Medical technology guidance SCOPE Virtual Touch Quantification to diagnose and monitor liver fibrosis. 2014. Available at:https://www.nice.org.uk/guidance/gid-mt210/documents/virtual-touch-quantification-to-diagnose-and-monitor-liver-fibrosis-final-scope2. Accessed Aug 2016.
Calvaruso V, et al. Acoustic radiation force impulse is better than transient elasography in assessing liver fibrosis in chronic hepatitis C using collagen proportionate area as reference. Hepatology. 2013;58(Suppl. 1):919A.
Aoki T, et al. Analysis of risk factors for aiming at early detection of hepatocellular carcinoma. Hepatology. 2013;58(Suppl. 1):958A.
Atzori S, et al. Non-invasive assessment of liver fibrosis: acoustic radiation force impulse of the left lobe correlates best with Ishak histology score. Hepatology. 2013;58(Suppl. 1):964A.
Sporea I, et al. The feasibility of shear-wave elastographic methods for non-invasive assessment of liver fibrosis in chronic viral hepatitis patients. Ultraschall Med. 2013;34.
Schneider MD, et al. Non-invasive assessment of liver fibrosis with acoustic radiation force imaging and transient elastography in chronic viral hepatitis. Ultraschall Med. 2013;34.
Cassinotto C, et al. Assessment of liver fibrosis with ARFI: comparison with M and XL probles of Fibroscan and FibroTest in chronic liver diseases [abstract]. Hepatol Int. 2013;7(Suppl. 1):S487.
Badea R, et al. ARFI performance in the noninvasive assessment of HCV cirrhosis, compared to transient elastography and FIB score [abstract]. Hepatol Int. 2013;7(Suppl. 1):S680.
Bota S, et al. ARFI elastography vs. transient elastography: which one is more influenced by high aminotransferases values. Hepatology. 2012;56(Suppl. 1):839A.
Le LT, et al. Comparison of liver stiffness values by virtual touch ARFI and fibroscan TE in large sample study of 554 cases. J Med Imaging Radiat Oncol. 2012;56(Suppl. 1):120.
Sporea I, Sirli R, Bota S, et al. Comparative study concerning the value of acoustic radiation force impulse elastography (ARFI) in comparison with transient elastography (TE) for the assessment of liver fibrosis in patients with chronic hepatitis B and C. Ultrasound Med Biol. 2012;38(8):1310–6.
Sporea I, et al. Which elastographic method (transient elastography or ARFI) is more useful for liver fibrosis evaluation in patients with chronic hepatitis C? An international multicenter study. Gastroenterology. 2012;142(Suppl. 1):S1013.
Friedrich-Rust M, Nierhoff J, Lupsor M, et al. Performance of Acoustic Radiation Force Impulse imaging for the staging of liver fibrosis: a pooled meta-analysis. J Viral Hepat. 2012;19(2):e212–9.
Karlas T, Pfrepper C, Wiegand J, et al. Acoustic radiation force impulse imaging (ARFI) for non-invasive detection of liver fibrosis: examination standards and evaluation of interlobe differences in healthy subjects and chronic liver disease. Scand J Gastroenterol. 2011;46(12):1458–67.
Sporea I, Şirli R, Popescu A, et al. Is it better to use two elastographic methods for liver fibrosis assessment? World J Gastroenterol. 2011;17(33):3824–9.
Calvaruso V, et al. Comparison of transient elastography (TE) and acoustic radiation force impulse (ARFI) for noninvasive staging of liver fibrosis in patients with chronic hepatitis C. Hepatology. 2010;52(Suppl. 1):1237A.
Sporea I, et al. Which is the best noninvasive ultrasound method for the evaluation of liver fibrosis? Gastroenterology. 2010;138(Suppl. 1):S511.
Lupsor M, Badea R, Stefanescu H, et al. Performance of a new elastography method (ARFI technology) compared to unidimensional transient elastography in the noninvasive assessment of chronic hepatitis C. Preliminary results. J Gastrointestin Liver Dis. 2009;18(3):303–10.
Lupsor M, et al. Performance of acoustic radiation force impulse imaging in the noninvasive assessment of liver firbosis in comparison to unidimensional transient elastography. J Hepatol. 2010;52(Suppl. 1):S165–6.
Sporea I, Badea R, Sirli R, et al. How efficient is acoustic radiation force impulse elastography for the evaluation of liver stiffness? Hepat Mon. 2011;11(7):532–8.
Bota S, Herkner H, Sporea I, et al. Meta-analysis: ARFI elastography versus transient elastography for the evaluation of liver fibrosis. Liver Int. 2013;33(8):1138–47.
Nierhoff J, Chávez Ortiz AA, Herrmann E, et al. The efficiency of acoustic radiation force impulse imaging for the staging of liver fibrosis: a meta-analysis. Eur Radiol. 2013;23(11):3040–53.
Friedrich-Rust M, Buggisch P, de Knegt RJ, et al. Acoustic radiation force impulse imaging for non-invasive assessment of liver fibrosis in chronic hepatitis B. J Viral Hepat. 2013;20(4):240–7.
Friedrich-Rust M, Lupsor-Platon M, de Knegt R, et al. Acoustic radiation force impulse-imaging in comparison to transient elastography for non-invasive assessment of liver fibrosis in chronic hepatitis C: a prospective international multicenter study [abstract no. P1011]. J Hepatol. 2014;60(Suppl. 1):S411–2.
Sporea I, Bota S, Peck-Radosavljevic M, et al. Acoustic radiation force impulse elastography for fibrosis evaluation in patients with chronic hepatitis C: an international multicenter study. Eur J Radiol. 2012;81(12):4112–8.
Centre Hospitalier de l’Université de Montréal and Canadian Institutes of Health Research Montreal Canada. Nonivasive staging of liver fibrosis: MR vs ultrasound (ELF) [ClinicalTrials.gov identifier NCT02044523]. 2015. US National Institutes of Health, ClinicalTrials.gov. http://clinicaltrials.gov. Accessed 30 Aug 2016.
Severance Hospital and Yonsei University Seoul Republic of Korea. Evaluation of liver fibrosis staging with acoustic radiation force impulse elastography [ClinicalTrials.gov identifier NCT01283230]. 2015. US National Institutes of Health, ClinicalTrials.gov. http://clinicaltrials.gov. Accessed 30 Aug 2016.
University of Michigan Michigan United States. Ultrasound based acoustic radiation force impulse, shear wave velocity imaging in pediatric patients undergoing liver biopsy [ClinicalTrials.gov identifier NCT01781208]. 2015. US National Institutes of Health, ClinicalTrials.gov. http://clinicaltrials.gov. Accessed 30 Aug 2016.
Liu Y, Dong CF, Yang G, et al. Optimal linear combination of ARFI, transient elastography and APRI for the assessment of fibrosis in chronic hepatitis B. Liver Int. 2015;35(3):816–25.
Yamada R, Hiramatsu N, Oze T, et al. Significance of liver stiffness measurement by acoustic radiation force impulse (ARFI) among hepatitis C patients. J Med Virol. 2014;86(2):241–7.
Chen SH, Li YF, Lai HC, et al. Effects of patient factors on noninvasive liver stiffness measurement using acoustic radiation force impulse elastography in patients with chronic hepatitis C. BMC Gastroenterol. 2012;12:105.
Kuroda H, Kakisaka K, Tatemichi Y, et al. Non-invasive evaluation of liver fibrosis using acoustic radiation force impulse imaging in chronic hepatitis patients with hepatitis C virus infection. Hepatogastroenterology. 2010;57(102–103):1203–7.
Nishikawa T, Hashimoto S, Kawabe N, et al. Factors correlating with acoustic radiation force impulse elastography in chronic hepatitis C. World J Gastroenterol. 2014;20(5):1289–97.
Rizzo L, Calvaruso V, Cacopardo B, et al. Comparison of transient elastography and acoustic radiation force impulse for non-invasive staging of liver fibrosis in patients with chronic hepatitis C. Am J Gastroenterol. 2011;106(12):2112–20.
Ye XP, Ran HT, Cheng J, et al. Liver and spleen stiffness measured by acoustic radiation force impulse elastography for noninvasive assessment of liver fibrosis and esophageal varices in patients with chronic hepatitis B. J Ultrasound Med. 2012;31(8):1245–53.
Stamuli E, Kruger J, Hutton J. Cost-effectiveness of ultrasound elastography in the assessment of liver fibrosis: economic report CEP08053. 2009. http://nhscep.useconnect.co.uk/CEPProducts/Catalogue.aspx. Accessed 1 Jun 2016.
Steadman R, Myers RP, Leggett L, et al. A health technology assessment of transient elastography in adult liver disease. Can J Gastroenterol. 2013;27(3):149–58.
Shah A, et al. Acoustic Radiation Force Imaging (ARFI) is able to identify early fibrosis in chronic liver disease results in 169 patients. United Kingdom Radiological Congress; 10–12 Jun 2013; Liverpool.
Crespo G, Fernández-Varo G, Mariño Z, et al. ARFI, FibroScan, ELF, and their combinations in the assessment of liver fibrosis: a prospective study. J Hepatol. 2012;57(2):281–7.
Takahashi H, Ono N, Eguchi Y, et al. Evaluation of acoustic radiation force impulse elastography for fibrosis staging of chronic liver disease: a pilot study. Liver Int. 2010;30(4):538–45.
Friedrich-Rust M, Wunder K, Kriener S, et al. Liver fibrosis in viral hepatitis: noninvasive assessment with acoustic radiation force impulse imaging versus transient elastography. Radiology. 2009;252(2):595–604.
Toshima T, Shirabe K, Takeishi K, et al. New method for assessing liver fibrosis based on acoustic radiation force impulse: a special reference to the difference between right and left liver. Gastroenterology. 2011;46(5):705–11.
Department of Health. NHS reference costs 2012 to 2013. 2013. https://www.gov.uk/government/publications/nhs-reference-costs-2012-to-2013. Accessed 1 Jun 2016.
National Institute for Health and Care Excellence. Peginterferon alfa and ribavirin for the treatment of chronic hepatitis C NICE technology appraisal [TA200]. London: NICE; 2010.
Noruegas M, Matos H, Gonçalves I, et al. Acoustic radiation force impulse-imaging in the assessment of liver fibrosis in children. Pediatr Radiol. 2012;42(2):201–4.
Hanquinet S, Rougemont AL, Courvoisier D, et al. Acoustic radiation force impulse (ARFI) elastography for the noninvasive diagnosis of liver fibrosis in children. Pediatr Radiol. 2013;43(5):545–51.
Sherman D, et al. Factors contributing to variance between ARFI elastography and liver histology: results of a large unselected consecutive series with simultaneous biopsy of ARFI measurement site [abstract]. European Association for the Study of Liver Disease meeting, British Society of Gastroenterology meeting and Radiological Society of North America meeting, 2014, London, Manchester and Chicago.
Acknowledgments
JP and JS were supported by the National Institute for Health Research (NIHR) Biomedical Research Centre based at Guy’s and St Thomas’ NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health. The authors thank Ms. Sophie Auld (Society and College of radiographers), Dr. Simon Elliot (Royal College of Radiologists), Mr. Colin Griffin (British Medical Ultrasound Society), Dr. Michael Heneghan (British Association for the Study of the Liver), Dr. Edmund Godfrey (Royal College of Radiologists), Professor Paul Sidhu (Royal College of Radiologists), Dr. Philip Shovron (Royal College of Physicians), Dr. Priya Narayanan (Royal College of Radiologists), Professor Roger Williams (Royal College of Physicians) and Dr. David Sherman (Royal College of Physicians) for their advice on the clinical evidence and for their contribution to the original EAC report for NICE. The authors also thank Paul Dimmock from NICE for advice on the original EAC report and the current manuscript.
Author contributions
The clinical effectiveness section of this paper was written by JS, EM, AC, VM, AD, YW, SA and JP. AC conducted the systematic review of the clinical evidence. JS and JP conducted the meta-analyses. The economic section and other sections were written by MR, TR and AP. VM, AD, YW, SA, JH, CL and SK contributed to the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
King’s Technology Evaluation Centre is funded by NICE to act as an External Assessment Centre for the Medical Technologies Evaluation Programme. The NHS has a financial interest in the guidance issued by NICE as a result of this work and two authors are NHS employees (Prof. Keevil and Dr. Lewis).
Conflict of interest
This summary of the Medical Technology Guidance was produced following the publication of the final guidance report. The summary has been reviewed by NICE but has not been externally peer reviewed by Applied Health Economics and Health Policy. The following authors are employed in the King’s Technology Evaluation Centre and declare a conflict of interest as they are contracted by NICE to evaluate medical technologies: Dr. Summers, Dr. Radhakrishnan, Ms. Morris, Dr. Chalkidou, Mr. Rua, Prof. Patel, Ms. McMillan, Dr. Douiri, Dr. Wang, Dr. Ayis, Prof. Keevil, Dr. Lewis and Prof. Peacock. Two of the authors (Prof. Keevil and Dr. Lewis) are NHS employees and thus have an additional conflict of interest. Ms. Higgins is a NICE employee and had no role in the preparation of the EAC report; however, this employment is a source of conflict of interest.
Appendices
Appendix 1: Selection criteria used to identify relevant published studies
Inclusion criteria | |
Population | Adults or children with chronic hepatitis B or C in whom assessment of liver fibrosis is indicated |
Intervention | The Virtual Touch™ Quantification (VTq) software application used with the Siemens Virtual Touch™ Tissue Imaging systems (the Acuson S2000™ or S3000™ ultrasound platforms) |
Outcomes | Correlation in assessment of stage of liver disease Sensitivity and specificity (using AUROC) in assessment of liver fibrosis Correlation in assessment of stage of fibrosis using Metavir score Use of antiviral drugs Quality-of-life measures Hospital bed usage and length of stay Requirement for liver biopsy Device-related adverse events |
Study design | Diagnostic accuracy studies |
Language restrictions | English language only Foreign language papers with English abstracts could be included |
Search dates | 2009–current |
Exclusion criteria | |
Population | Mixed patient cohort, use of a fibrosis score other than Metavir, overlapping cohorts with other identified populations |
Study design | Case studies, editorials, letters, reviews |
Interventions | No restriction |
Appendix 2: Clinical evidence search strategy
Ovid MEDLINE® in-process and other non-indexed citations and Ovid MEDLINE® 1946 to present, and EMBASE 1980 to 10 July 2014; searched on 10 July 2014
1 | virtual touch tissue quantification.mp. |
2 | acoustic radiation force impulse.mp. |
3 | acoustic radiation force impulse imaging.mp. |
4 | acoustic radiation force impulse elastography.mp. |
5 | ARFI elastography.mp. |
6 | elasticity imaging techniques.mp. or Elasticity Imaging Techniques/ |
7 | liver diseases.mp. or Liver Diseases/ |
8 | liver fibrosis.mp. or Liver Cirrhosis/ |
9 | Hepatitis/ or Hepatitis B, Chronic/ or Hepatitis, Viral, Human/ or Hepatitis B/ or Hepatitis C/ or Hepatitis C, Chronic/ or hepatitis.mp. |
10 | prognosis.mp. or Prognosis/ |
11 | predictive.mp. or “Predictive Value of Tests”/ |
12 | receiver operating characteristic.mp. or ROC Curve/ |
13 | adverse event.mp. |
14 | “Sensitivity and Specificity”/ or diagnostic accuracy.mp. |
15 | antiviral.mp. or Antiviral Agents/ |
16 | quality of life.mp. or “Quality of Life”/ |
17 | 1 or 2 or 3 or 4 or 5 or 6 |
18 | 7 or 8 or 9 |
19 | 10 or 11 or 12 or 13 or 14 or 15 or 16 |
20 | 17 and 18 and 19 |
21 | Limit 20 to English language |
22 | Limit 21 to yr = “2009–current” |
23 | Limit 22 to humans |
24 | Remove duplicates from 23 |
The Cochrane Library, to present; searched on 11 July 2014.
Search all text | Acoustic radiation force impulse | |
OR | Search all text | ARFI elastography |
OR | Search all text | ARFI |
OR | Search all text | Virtual touch tissue quantification |
OR | Search all text | Elasticity imaging |
Database of Abstracts of reviews of Effects (DARE), to present; searched on 11 July 2014.
Any field | Acoustic radiation force impulse | OR |
Any field | Virtual touch tissue quantification | OR |
Any field | Elasticity imaging |
Appendix 3: PRISMA flow diagram showing the company’s search (dotted box) and the External Assessment Centre (EAC) search results

Appendix 4: Model assumptions for clinical parameters
Assumption and justification |
People categorised as false negative for fibrosis would return and be re-diagnosed as true positive within 1 year |
Prevalence rates for stages of fibrosis were different for VTq and TE based on the EAC’s meta-analyses. The combined hepatitis B and C prevalence rates for VTq were used for TE and liver biopsy in the model to ensure compatibility |
Combined hepatitis B and C prevalence and diagnostic accuracy figures for F ≥ 3 fibrosis were not available from the meta-analysis. The EAC therefore used figures for hepatitis C across the model for this stage |
Treatment delay resulting from misdiagnosis was unlikely to have a clinical impact and so long-term modelling of disease progression was not needed. According to published clinical evidence and expert advice gathered by the EAC, progression in both hepatitis B and C is relatively slow |
People diagnosed as being at stage F ≥ 2 had fibrosis and those at stage F ≤ 1 did not |
The majority of misclassified (false positive) cases for VTq and TE would be diagnosed as having F2 fibrosis. A proportion of those with F2 fibrosis would be misclassified as having F3 or F4 fibrosis. These proportions were chosen arbitrarily and subjected to sensitivity analyses |
People diagnosed with F3 or F4 fibrosis would have antiviral therapy |
A mortality risk of 0.003 would apply to liver biopsy |
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Summers, J.A., Radhakrishnan, M., Morris, E. et al. Virtual Touch™ Quantification to Diagnose and Monitor Liver Fibrosis in Hepatitis B and Hepatitis C: A NICE Medical Technology Guidance. Appl Health Econ Health Policy 15, 139–154 (2017). https://doi.org/10.1007/s40258-016-0277-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-016-0277-7