Abstract
Pleural infection remains a major healthcare problem in the 21st century. It is responsible for significant morbidity and mortality in both adults and children across developed as well as developing countries. Its incidence continues to rise globally despite the introduction of the pneumococcal conjugate vaccine in 2000 and modern advances in medical care. The pathobiology of empyema remains relatively poorly understood and its changing bacteriology over time is important to recognize as it is likely to have future implications in terms of patient management, outcome, and healthcare costs. Many questions still remain regarding the diagnosis and management of pleural infection. This paper reviews current data on biomarkers, bacterial tests, and imaging modalities, in addition to discussing potential future directions on research in the field.
Similar content being viewed by others
Introduction
Pleural infection is a centuries-old serious respiratory illness, first described by Hippocrates of Kos (460–377 BC) who recognized that “pneumonia coming on pleurisy is bad.” Empyema was fatal in as many as 70% of patients between 400 BC and 1800 AD, though the mortality rate gradually improved to ~30% by the 1950s [1]. Pneumonia-related pleurisy has claimed many famous lives, including Benjamin Franklin (1706–1790), Guillaume Dupuytren (1777–1835), and Anna Pavlova (1881–1931). Still, in the 21st century, ~15% of adult patients with empyema do not survive the illness [2].
Establishing the diagnosis of pleural infection has always been challenging. Hippocrates had to rely solely on the clinical signs of “pain in the side, fever, shivering, and breathing rapidly” [1]. Advances in imaging and laboratory tests have vastly improved the diagnostic accuracy, but major limitations exist [3] and delay in diagnosis (and treatment) contributes to the disease morbidity.
Empyema results from bacterial infection of the pleural cavity, but capturing the offending organism is not always straightforward [4]. Sir William Osler (1848–1919), the father of modern medicine, died from an empyema. Although he analyzed his own disease course in the greatest details, the causative organism(s) was never definitively identified [5]. No pathogens are cultured in ~40% of empyema patients even in the modern era.
This paper discusses contemporary challenges in the diagnosis of pleural infection, especially in view of its rising incidence and changing bacteriology, and future perspectives.
The rising incidence from epidemiologic data
Each year in the UK and USA over 65,000 patients suffer from a complicated parapneumonic effusion or empyema [6]. The incidence of empyema is rising worldwide in both developed and developing countries, and across ages. Increased rates have been seen in pediatric and adult populations alike, contributing to a significant degree of morbidity and mortality. Alarmingly, the rate of empyema deaths has increased significantly since 2000, with a sixfold higher death rate in 2000–2004 compared to 1950–1975 in a study from Utah [7].
In children ≤18 years of age, the annual empyema-associated hospitalization rates increased almost 70% between 1997 and 2006 in the USA despite decreases in the bacterial pneumonia and invasive pneumococcal disease rates [8]. Similar findings have been reported in studies from Europe and Asia; the annual incidence of empyema in Israeli children increased strikingly from 5 to 42 per million between 1990 and 2002 [9]. The annual population-based incidence of empyema among children under 5 years in Taiwan increased year by year from 1997 to 2004, from 4.94 to 15.55 episodes per 100,000 children-year [10]. Likewise, increased pleural infection rates in adults over the last decade have been seen in Canada [11] and in USA where pleural infection rates have increased by 3% per year over the last 2 decades [12].
The prevalence of causative organisms of pleural infection differs around the world and can vary over time, depending on the source of infection (community vs hospital acquired empyema) and host factors (patient age, immune status). Data from the UK Multicentre Intrapleural Sepsis Trial (MIST-1) confirmed streptococcal species as the most prevalent organisms isolated in community-acquired cases of pleural infection, with the Streptococcus milleri group as the leading cause, accounting for one-third of cases [2]. Streptococcus pneumoniae is the second most common pathogen in adult empyema and the most common causative organism in pediatric empyema [4]. Other commonly occurring microbes include anaerobes and staphylococci, the latter accounting for 46% of hospital-acquired cases in the MIST-1 cohort, 60% of which were methicillin resistant [13]. Conversely, Klebsiella pneumoniae was the most frequent cause of community-acquired empyema or complicated parapneumonic effusion in Taiwanese adults treated during the period 2001–2008. Diabetes mellitus, liver cirrhosis, and bronchogenic carcinoma were shown to be independent risk factors for K. pneumoniae infection in the study [14].
The annual incidence of invasive disease caused by S. pneumoniae has decreased significantly in all age groups with the introduction of the heptavalent pneumococcal conjugate vaccine PCV-7 in 2000 [15]. Despite reductions in invasive disease due to PCV-7 serotypes (4, 6B, 9V, 18C, 19F, and 23F), pediatric pneumococcal empyema rates have continued to rise significantly [16] suggesting a change in bacteriology and replacement of other serotypes causing empyema. In Utah prior to license of PCV-7, 62% of cases of pediatric pneumococcal empyema were due to non-vaccine serotypes, primarily serotype 1, compared to 98% in 2007 (P < 0.001) when cases were predominantly due to serotypes 1, 3, 19A, and 7F [17]. In adults with pneumonia and S. pneumoniae septicemia, those infected with serotypes of high invasive disease potential (1, 5, and 7F) were found to be at significantly higher risk of developing pleural infection (17.2% versus 5.1%) than patients infected with low potential serotypes [18]. A Spanish study recently analyzed the differences in the incidence and serotype distribution between the pre and post-PCV7 era in young adults with pneumococcal empyema. The incidence increased during the post vaccine period (from 0.5 to 1.6 cases per 100,000 person-years), mainly as a result of the emergence of serotype 1 which caused 43.3% of cases of pneumococcal empyema [19•]. This again supports the idea that the widespread adoption of the vaccine has favored the spread of these empyema-prone serotypes by reducing their natural competition.
The observed rise in incidence of pleural infection and associated mortality rate over time has occurred in spite of advances in medical care. This is of grave concern globally and raises some interesting questions. Does the cultured organism from empyema fluid correctly represent the causative organism? Are we using inappropriate antibiotics and/or delaying their initiation? Is antibiotic resistance increasing in community acquired cases of pleural infection? Available epidemiological data would support the call for more sensitive diagnostic techniques for microbes causing pleural infection, along with improved antibacterial agents, vaccines, and more standardized treatment strategies to reduce disease mortality and morbidity.
Biomarkers and diagnostic biochemical tests
All patients with a presumptive diagnosis of pleural space infection should undergo thoracentesis. Clinical data (ie, febrile acute illness, peripheral leukocytosis, lung infiltrates) in conjunction with a good working knowledge of pleural fluid analysis enables the physician to make a confident diagnosis of parapneumonic effusion in most cases. Where biochemistries of the aspirated fluid are not immediately available, reagent strips, designed for urine but applied to pleural fluid specimens, may provide useful diagnostic information in just a few minutes. A recent study tested commercially available reagent strips for leukocyte esterase on 128 patients with different causes of pleural effusion, including 42 non-mycobacterial infections, 15 tuberculosis, and 71 non-infectious etiologies [20]. A positive test (ie, any visual color change in the leukocyte label of the dipstick) displayed a sensitivity of 42%, specificity of 100%, and positive likelihood ratio (LR) of 75 for the detection of non-tuberculous infectious effusions [20]. Therefore, reagent strips may speed up the bedside diagnosis of infectious effusions in the setting of resource-limited healthcare systems.
From the biochemical standpoint, parapneumonic effusions are typically neutrophil-rich exudates. However, a pleural fluid dominated by polymorphonuclear leukocytes can also occur in 10% and 20% of tuberculous and malignant effusions, respectively, as well as in a number of acute effusions [21]. Recently, Porcel et al. examined the diagnostic usefulness of pleural fluid routine biochemistries (white blood cell count and differential, pH, glucose, lactate dehydrogenase [LDH], adenosine deaminase [ADA]) and C-reactive protein (CRP) for labeling parapneumonic effusions among nearly 2,000 non-purulent exudates [22]. The latter is an acute phase reactant commonly used as an infection marker. It was found that pleural fluid CRP greater than 100 mg/L (sensitivity 36%, specificity 98%, LR 19.4) and a percentage of neutrophils above 85% (sensitivity 44%, specificity 94%, LR 7.8) were the most important parameters in the identification of parapneumonic effusions, both exhibiting areas under the curve (AUC) higher than 0.80 [22].
More so than correctly diagnosing an infectious effusion, the greater clinical challenge is to identify complicated parapneumonic effusions, specifically those non-purulent-appearing effusions that require chest tube drainage. Clinical guidelines advocate measurement of pleural fluid pH or glucose as the first laboratory criterion for instituting tube thoracostomy [23]. The rationale behind this is that the more advanced the pleural space infection is, the lower the pleural fluid pH and glucose levels become. If the pleural fluid pH is less than 7.20 or the pleural fluid glucose is below 60 mg/dL the pleural space should probably be drained (LR about 5.5) [22, 23]. Nevertheless, about 40% of patients who will eventually be treated by tube thoracostomy have values above these thresholds [22]. Recently, it has been shown that CRP levels higher than 100 mg/L in the pleural fluid were an equally effective marker of complicated parapneumonic effusions (sensitivity 58%, specificity 88%, LR 5) [22]. The combination of CRP with either pH or glucose at the established cutoff points using an “or” rule, wherein the pleural space would be drained if any test is positive, increased sensitivity for detecting complicated parapaneumonics to nearly 80% [22]. On the other hand, the presence of both high CRP and low pH or glucose values argues strongly for pleural fluid drainage (specificity 97%, LR 15) [22]. The theoretic advantage of combining several biomarkers into a single classification rule is that it should help to improve their classification accuracy and, therefore, their clinical usefulness. Whether pleural fluid CRP may be included among the routine biochemical data used to make decisions on drainage of non-purulent collections warrants further studies.
In addition to the tests described above, there have been a number of promising biomarkers of infection under research [24•]. They reflect different stages of the inflammatory cascade triggered by microorganisms and can be measured by commercially available immunoassays. Although the results are limited by the small populations tested, some pleural fluid biomarkers exhibiting acceptable performances for discriminating between complicated and non-complicated parapneumonic effusions are, in decreasing order of positive LRs: tumor necrosis factor-α ≥ 80 pg/mL (LR 6.8) [25], myeloperoxidase >3,000 μg/L (LR 5.9) [26], matrix metalloproteinase-2 ≤ 343 ng/mL (LR 5.5) [27], neutrophil elastase >3,500 μg/L (LR 4.6) [28], interleukin-8 ≥ 1,000 pg/mL (LR 4.6) [29], lipopolysaccharide binding protein ≥ 17 μg/mL (LR 4) [30], and soluble triggering receptor expressed on myeloid cell ≥180 pg/mL (LR 3.9) [30]. Other biomarkers may be clinically meaningful because of their high sensitivity and, thus, their extremely low LR negative for complicated effusions. Examples are a pleural interleukin 1β > 3.9 pg/mL (LR negative 0.02) [31], terminal complement complex SC5b-9 > 2,000 μg/L (LR negative 0.03) [32], and 8-isoprostane >35.1 pg/mL (LR negative 0.04) [33], where values lower than the reported thresholds make a complicated parapneumonic effusion highly unlikely. Of note, procalcitonin, a prohormone used to confirm or exclude the diagnosis of severe bacterial infection, lacks the ability to separate complicated from uncomplicated effusions when evaluated in the pleural fluid [30].
A confident comparative analysis between new and traditional markers of complicated effusions is hampered by incorporation bias. That is, most physicians use the pleural fluid pH and glucose to select patients who should undergo tube thoracostomy, thereby artificially increasing their discriminating properties [24•]. Since the new biomarkers provide the same information as the widely established pH and glucose, or the easily performed CRP, it is not anticipated that they will replace or be added to those currently being used for clinical decision-making in parapneumonic effusions.
Imaging of pleural infection
Chest X-ray
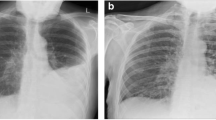
The initial investigation for suspected pleural infection remains chest radiography and a posteroanterior X-ray can detect effusions ≥200–300 mL [34, 35]. There are no radiographic features with high specificity for pleural infection, although a new loculated effusion is suspicious for infection in the context of sepsis.
Pleural ultrasound
Ultrasonography is increasingly used by physicians to improve the diagnosis and management of pleural infection [36•]. It allows real-time radiation-free pleural space imaging, and is particularly useful when bedside imaging is required for critically unwell patients. Adequate imaging can be achieved with most portable ultrasound machines.
Ultrasound has a higher sensitivity than chest X-ray in detecting pleural fluid [37, 38]. It is able to accurately locate loculated fluid [39], estimate pleural fluid depth and volume [40–43], and allows guided pleural intervention, which is safer than clinical examination combined with chest X-ray review (that risk organ perforation in 10% of cases [44]). Combining ultrasound with policies restricting pleural interventions to a core group of physicians led to an eight-fold reduction in the risk associated with pleural aspiration [45•]. Other observational studies have also suggested a lower complication rate associated with ultrasound guidance [46, 47]. Ultrasound can accurately distinguish pleural fluid from underlying consolidation and atelectasis, thereby avoiding injudicious pleural intervention [48].
Sonographic features allow effusions to be characterized into anechoic (Fig. 1), complex nonseptated (Fig. 2), complex septated (Fig. 3), and homogenously echogenic effusions (Fig. 4) [49]. Anechoic effusions may be transudative or exudative (and require sampling to clarify), whereas complex and echogenic effusions are virtually always exudative. Septations suggest an inflammatory effusion, but are often also associated with other conditions such as pleural malignancy.
Some sonographic characteristics may have a use in risk-stratifying patients and aid in determining when to sample an effusion to rule out pleural infection. 1–2 cm fluid depth is a conventional cutoff for sampling, although heavily echogenic fluid (suggestive of pus or blood [50]) might lower this threshold or suggest an aggressive patient follow-up strategy. Tu et al. [51] examined whether ultrasound could predict those with pleural infection amongst 94 febrile ICU patients. Fluid sampling found 15 cases of empyema: none was anechoic on imaging, suggesting that routine fluid sampling is not required for anechoic effusions. However, pleural pH and other biochemical criteria were not included in that study to exclude complicated parapneumonic effusions.
Pleural fluid septation density has been proposed to predict outcome, in particular chest tube drainage success. Studies have shown a success rate of drainage for 92%–100% of anechoic effusions, 79%–82% of complex non-septated effusions, 80% of homogenously echogenic effusions, and 51%–63% of complex septated effusions [52–54]. Chen et al. [55] found a higher treatment failure rate for complex septated effusions compared with non-septated effusions. However, others have failed to demonstrate an association with outcome or surgical requirements [56]. Overall, septated effusions should not deter physicians from using chest tubes given that the majority of such effusions still drain well.
In spite of many advantages of bedside ultrasound, several factors may make imaging difficult, including obesity, air in the pleural cavity (eg, from bronchopleural fistula), and subcutaneous emphysema. The increased adoption of pleural ultrasound by physicians mandates adequate training to avoid patient harm [57, 58].
Computed tomography (CT)
CT is not routinely used for imaging pleural infection, but has a role when other imaging modalities are ambiguous, when malignancy or unusual causes of pleural infection (such as oesophageal rupture) are suspected, or when pleural intervention is impossible with ultrasound.
Standard contrast-enhanced thoracic CT with image-acquisition in the arterial phase is suboptimal for pleural imaging. Specific “pleural protocols” acquire images in the tissue phase (~ 50–60 s post contrast injection) for optimal pleural enhancement while still achieving reasonable major vessel enhancement [59•].
Pleural infection (and other causes of exudative effusions) result in parietal pleural enhancement and smooth parietal thickening. Extrapleural changes in the subcostal tissue between the ribs and parietal pleura are commonly associated with pleural infection and manifest as increased extrapleural fat attenuation and soft tissue thickening (Fig. 5) [60–62].
The distinction between a peripheral pulmonary abscess and loculated pleural infection is often difficult, but CT features can aid in this distinction. The “split pleura” sign describes the separation of visceral and parietal pleura around a loculated pleural infection, not present in a pulmonary abscess. Other features favoring pleural infection rather than lung abscess are fluid collections that 1) make obtuse rather than acute angles with the chest wall, 2) are lenticular (rather than round) in shape, and 3) cause compression of the adjacent lung [63].
Magnetic resonance imaging (MRI)
MRI is used infrequently for pleural infection, but may have a specific role for younger patients requiring repeated imaging, in whom radiation exposure is of particular concern. Respiratory and cardiac motion often degrades image quality, but gating techniques decrease artifacts. Pleural infection fluid gives a low signal on T1-weighted and high signal on T2-weighted images (Fig. 6) [64]. MRI readily detects extrapleural fat changes and is superior to CT in visualizing septations.
While a variety of imaging features may suggest pleural infection, the absence of such features is not sufficient to rule out infection. All effusions large enough to be aspirated safely should be sampled to enable pleural fluid analysis and determine which effusions require chest tube drainage. Physician-performed pleural ultrasound has led to significant improvements in pleural infection diagnosis and has improved the safety of pleural interventions.
Bacterial tests and bacteriology of pleural fluid
Given the remarkably consistent pattern found for the major pathogens for community-acquired pneumonia (CAP) worldwide [65], it should not be surprising that most series of community-acquired empyema report very similar results. In children, Streptococcus pneumoniae is overwhelming the most common pathogen accounting for >80% of culture-positive cases, with Staphylococcus aureus a distant second [66–69]. However, in adults Streptococcus milleri is much more commonly isolated than S. pneumoniae and easily the most common pathogen at 25%–40% of culture-positive cases in most series [13, 70–73]. Many laboratories do not usually further speciate S. milleri, which is a heterogeneous group of facultatively Gram-positive anaerobic cocci (S. intermedius, S. anginosus, and S. constellatus) of the viridans streptococci group.
After S. milleri, S. pneumoniae, and S. aureus, there is a long list of other aerobic organisms including Gram-negative bacteria such as Escherichia coli, Haemophilus influenza, and Klebsiella pneumoniae [66, 67]. Gram-negative pathogens appear to be more common in the elderly [74], as they are in pneumonia [65]. It is also not uncommon for cultures to grow a mix of aerobic and anaerobic bacteria, with the commonest anaerobes being Bacteroides fragilis [75]. Given the difficulties in culturing anaerobic bacteria if samples are not handled and processed correctly the frequency of mixed infections is probably underestimated.
Much as it is for pneumonia, it is very important to distinguish between nosocomial and community acquired infections as there is a very different mix of pathogens identified as the usual causative agents [72]. With nosocomial empyema S. milleri and S. pneumoniae are much less commonly isolated, although S. aureus remains extremely common. What is much more common in nosocomial disease are pathogens such as the enterobacteria, enterococci, and Pseudomonas aeruginosa [76].
Despite a general consistency across most etiological studies there can be important regional differences and clinicians need to be aware of any important differences in their local etiology. For example, two reports from Taiwan found K. pneumoniae was the commonest cause of empyema in community-acquired and hospital-acquired cases [14, 77]. The rise of multi-resistant S. aureus (MRSA) is also a major cause of concern in community-acquired cases in some areas and is a direct flow on from the rise of community-acquired MRSA pneumonia [78–80]. MRSA pneumonia appears especially prone to be complicated by empyema, from 35% to 75% of patients depending on the series reported [81–83], and is also associated with high mortality rates [72, 81, 83]. Clinicians should therefore be particularly vigilant for the development of empyema when S. aureus is identified in a patient with pneumonia.
One of the frustrations for clinicians is that the pathogen is usually not identified in patients with empyema, with routine cultures of pleural fluid and blood generally negative [16, 84]. When antibiotics have already been given the yield is even lower, typically well below 10%. One of the reasons for the low culture rate is the loss of viable bacteria in transport to the laboratory. If pleural fluid is injected immediately after aspiration into blood culture bottles, including anaerobic bottles, the culture yield can be increased by up to 50% [85].
Given the low yield from conventional cultures, attempts have been made to improve the diagnostic rate by the use of newer techniques including polymerase chain reaction (PCR)-based assays and antigen detection. While these approaches have generally resulted in small improvements in detection for most pathogens so far [13], for S. pneumoniae they have proved exceptionally successful. For reasons not entirely clear it appears that pneumococcus is particularly amenable to detection by PCR compared to other pathogens such as S. aureus or S. pyogenes [69]. Because of the success of detecting S. pneumoniae with PCR, the latter is a much more useful tool in pediatric empyema.
In a study of 89 children with empyema, Strachan et al. found that pleural fluid culture was positive for S. pneumoniae in 5/84 samples (5.9%) whereas using a PCR-based approach to detect the pneumococcal gene lytA, 43/79 pleural fluid samples were positive, a nearly 10-fold increase in sensitivity [86•]. Other groups have also reported significantly increased yield (2–4x culture rate) with a variety of PCR methods [69, 87].
A separate manuscript from Strachan et al. used the Binax urinary antigen test for pneumococcus on pleural fluid and found the sensitivity to be 83.8% and specificity to be 93.5% compared to a composite gold standard of any other test (PCR, pleural fluid culture, blood culture) being positive [88]. A Spanish research group had even better results for the Binax urinary antigen test on pleural fluid (96% sensitivity, 100% specificity) when compared against the combination of culture and PCR [89]. However, the PCR-positive rate was not quite as good (13/40) as the study by Stachan et al., possibly due to an inferior PCR assay [90]. A further smaller study also reported excellent sensitivity with the Binax antigen test when used on pleural fluid [87].
The concept of measuring bacterial load as a marker of disease severity is increasingly entering the sepsis and pneumonia literature [91], something that can be readily done with PCR using a real-time platform. A recent study by Munoz-Almagro et al. demonstrated that not only was their pneumococcal PCR-assay very sensitive at four times the rate of culture, but that quantitating the bacterial load in pleural fluid was highly predictive of the clinical outcome. As expected bacterial load was lower in patients with prior antibiotics, but higher loads were associated with longer length of hospital stay and longer duration of pleural drainage [92]. This represents a major area of current and future research.
The future perspectives
It is unknown why pulmonary infection with some pathogens is more likely to cause parapneumonic effusions than infection with other pathogens. Although the Streptococcus intermedius-anginosus-constellatus (milleri) group of bacteria are the most common organisms responsible for pleural infection in adults [13], these commensals are rarely implicated in pneumonia. This casts doubt over the traditional belief that empyema always results as a consequence of lung infection. A related problem is to identify the pathogen causing the parapneumonic effusion. In the above study, cultures were positive in 232 of 434 patients [13] and nucleic acid amplification identified the responsible bacteria in an additional 70 cases. Nevertheless, no organism was identified in the remaining 132 patients (30.4%) [13].
Identifying which parapneumonic effusion needs drainage remains challenging. Low pleural fluid pH was shown as the most sensitive indicator in the 1970s [93]. Subsequently, glucose (<60 mg/dL) and LDH (> 3x the upper limit of normal) were added as indicators that a parapneumonic effusion was complicated [94]. In these early studies the clinician knew the result of the pleural fluid analysis which probably influenced their decision whether to insert a chest tube. A huge number of pleural fluid biomarkers [30, 31] have been evaluated since; none is superior to the pleural fluid pH, glucose, or LDH in identifying complicated parapneumonic effusions. The need for a better biomarker remains.
Which patients with parapneumonic effusions should undergo a thoracentesis? The current guidelines [6, 23] state that if the pleural effusion is more than 10 mm in thickness of a lateral decubitus, CT scan or ultrasound, a thoracentesis is indicated. However, many patients have more pleural fluid than this and do fine without a thoracentesis. A recent paper [95] suggested that if the thickness of the pleural fluid was less than 20 mm, the effusions were rarely complicated and a thoracentesis was not indicated.
If the decision is made to sample a parapneumonic effusion, how should it be performed? There are no controlled studies comparing the potential options—a diagnostic thoracentesis, a therapeutic thoracentesis, or the insertion of a small chest tube—that allows the shortest hospitalization and the lowest need for thoracoscopy.
Conclusions
Improvements in healthcare and availability of antibiotics, since the days of Hippocrates, have failed to eliminate pleural infection. Instead it remains a common illness worldwide with a rising incidence, morbidity, and mortality. The causative bacteria continue to evade current pleural fluid culture methods in an unacceptably high rate. No new diagnostic biomarkers have made a realistic impact in pleural infection. Imaging techniques have helped precision of drainage but its benefits on the overall outcome of this illness remain limited.
A better understanding of the bacterial interaction with the lung and pleura, better characterization of the host immune response to the bacteria, and the application of new molecular technology to pleural investigations are needed in the next stage of our attempts to win the centuries-long battle against this disease that has claimed so many human lives.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Tassi GF, Marchetti GP. Pleural disease: historic perspective. In: Light RW, Lee YCG, editors. Textbook of Pleural Diseases. 2nd ed. London: Hodder; p. 1–9.
Maskell NA, Davies CW, Nunn AJ, et al. First Multicenter Intrapleural Sepsis Trial (MIST1) Group. U.K. Controlled trial of intrapleural streptokinase for pleural infection. N Engl J Med. 2005;352:865–74.
Brims FJ, Lansley SM, Waterer GW, et al. Empyema thoracis: new insights into an old disease. Eur Respir Rev. 2010;19:220–8.
Lisboa T, Waterer G, Lee YCG. Pleural Infection: changing bacteriology and its implications. Respirology. 2011;16:598–603.
Barondess JA. A case of empyema: notes on the last illness of Sir William Osler. Trans Am Clin Climatol Assoc. 1975;86:59–72.
Colice G, Curtis A, Deslauriers J, et al. Medical and surgical treatment of parapneumonic effusions: an evidence based guideline. Chest. 2000;118(4):1158–71.
Bender J, Ampofo K, Sheng X, et al. Parapneumonic empyema deaths during past century, Utah. Emerg Infect Dis. 2009;15:44–8.
Li S, Tancredi D. Empyema hospitalizations increased in US children despite pneumococcal conjugate vaccine. Pediatrics. 2010;125:26–33.
Goldbart A, Leibovitz E, Porat N, et al. Complicated community acquired pneumonia in children prior to the introduction of the pneumococcal conjugate vaccine. Scand J Infect Dis. 2009;41:182–7.
Wu P, Huang L, Chang I, et al. The epidemiology of hospitalized children with pneumococcal/lobar pneumonia and empyema from 1997 to 2004 in Taiwan. Eur J Paediatr. 2010;169:861–6.
Finley C, Clifton J, Fitzgerald J, et al. Empyema: an increasing concern in Canada. Can Respir J. 2008;15:85–9.
Farjah F, Symons R, Krishnadasan B, et al. Management of pleural space infections: a population-based analysis. J Thorac Cardiovasc Surg. 2007;133:346–51.
Maskell N, Batt S, Hedley E, et al. The bacteriology of pleural infection by genetic and standard methods and its mortality significance. Am J Respir Crit Care Med. 2006;174:817–23.
Lin Y, Chen T, Siu L, et al. Clinical and microbiological characteristics of community acquired thoracic empyema or complicated parapneumonic effusion caused by Klebsiella pneumoniae in Taiwan. Eur J Clin Microbiol Infect Dis. 2010;29:1003–10.
Kyaw M, Lynfield R, Schaffner W, et al. Effect of introduction of the pneumococcal conjugate vaccine on drug resistant Streptococcus pneumoniae. N Engl J Med. 2006;345:1455–63.
Hendrickson D, Blumberg D, Joad J, et al. Five-fold increase in pediatric parapneumonic empyema since introduction of pneumococcal conjugate vaccine. Pediatr Infect Dis J. 2008;41:182–7.
Byington C, Hulten K, Ampofo K, et al. Molecular epidemiology of pediatric pneumococcal empyema from 2001-2007 in Utah. J Clin Microbiol. 2010;48:520–5.
Lujan M, Gallego M, Belmonte Y, et al. Influence of pneumococcal serotype group on outcome in adults with bacteraemic pneumonia. Eur Respir J. 2010;36:1073–9.
• Burgos J, Lugan M, Falco V, et al. The spectrum of pneumococcal empyema in adults in the early 21st century. Clin Infect Dis. 2011;53:254–61. This study addresses the differences in the incidence, disease characteristics, and serotype distribution in pneumococcal empyema in adults between the pre and post-PCV7 eras.
Porcel JM, Esquerda A, Bielsa S. A specific point-of-care screen for infectious pleural effusions using reagent strips. Eur Respir J. 2011;37:1528–30.
Porcel JM. Pearls and myths in pleural fluid analysis. Respirology. 2011;16:44–52.
Porcel JM, Bielsa S, Esquerda A, et al. Pleural fluid C-reactive protein contributes to the diagnosis and assessment of severity of parapneumonic effusions. Lung. In press.
Davies HE, Davies RJO, Davies CWH. Management of pleural infection in adults: British Thoracic Society pleural disease guideline 2010. Thorax. 2010;65:ii41–53.
• Porcel JM. Pleural fluid tests to identify complicated parapneumonic effusions. Curr Opin Pulm Med. 2010;16:357–61. This review describes the role of traditional and newer pleural fluid biochemistries in guiding the therapeutic approach to parapneumonic effusions.
Porcel JM, Vives M, Esquerda A. Tumor necrosis factor-α in pleural fluid: a marker of complicated parapneumonic effusions. Chest. 2004;125:160–4.
Alegre J, Jufresa J, Segura R, et al. Pleural-fluid myeloperoxidase in complicated and noncomplicated parapneumonic effusions. Eur Respir J. 2002;19:320–5.
Oikonomidi S, Kostikas K, Kalomenidis I, et al. Matrix metalloproteinases levels in the differentiation of parapneumonic pleural effusions. Respiration. 2010;80:285–91.
Alemán C, Alegre J, Segura RM, et al. Polymorphonuclear elastase in the early diagnosis of complicated pyogenic pleural effusions. Respiration. 2003;70:462–7.
Porcel JM, Galindo C, Esquerda A, et al. Pleural fluid interleukin-8 and C-reactive protein for discriminating complicated non-purulent from uncomplicated parapneumonic effusions. Respirology. 2008;13:58–62.
Porcel JM, Vives M, Cao G, et al. Biomarkers of infection in pleural fluid for the differential diagnosis of pleural effusions. Eur Respir J. 2009;34:1383–9.
Marchi E, Vargas FS, Acencio MM, et al. Pro- and anti-inflammatory cytokines levels in complicated and non-complicated parapneumonic effusions. Chest. 2011, In press.
Vives M, Porcel JM, Gázquez I, et al. Pleural SC5b-9: a test for identifying complicated parapneumonic effusions. Respiration. 2000;67:433–8.
Tsilioni I, Kostikas K, Kalomenidis I, et al. Diagnostic accuracy of biomarkers of oxidative stress in parapneumonic pleural effusions. Eur J Clin Invest. 2011;41:349–56.
Emamian SA, Kaasbol MA, Olsen JF, Pedersen JF. Accuracy of the diagnosis of pleural effusion on supine chest X-ray. Eur Radiol. 1997;7:57–60.
Blackmore CC, Black WC, Dallas RV, Crow HC. Pleural fluid volume estimation: a chest radiograph prediction rule. Acad Radiol. 1996;3:103–9.
• Rahman NM, Singanayagam A, Davies HE, et al. Diagnostic accuracy, safety and utilisation of respiratory physician-delivered thoracic ultrasound. Thorax. 2010;65:449–53. Study demonstrating that physicians can safely use thoracic ultrasound, following adequate training.
Lipscomb DJ, Flower CD, Hadfield JW. Ultrasound of the pleura: an assessment of its clinical value. Clin Radiol. 1981;32:289–90.
Eibenberger KL, Dock WI, Ammann ME, et al. Quantification of pleural effusions: sonography versus radiography. Radiology. 1994;191:681–4.
Wu RG, Yuan A, Liaw YS, et al. Image comparison of real-time gray-scale ultrasound and color Doppler ultrasound for use in diagnosis of minimal pleural effusion. Am J of Respir Crit Care Med. 1994;150:510–4.
Balik M, Plasil P, Waldauf P, et al. Ultrasound estimation of volume of pleural fluid in mechanically ventilated patients. Intensive Care Med. 2006;32:318–21.
Remérand F, Dellamonica J, Mao Z, et al. Multiplane ultrasound approach to quantify pleural effusion at the bedside. Intensive Care Med. 2010;36:656–64.
Vignon P, Chastagner C, Berkane V, et al. Quantitative assessment of pleural effusion in critically ill patients by means of ultrasonography. Crit Care Med. 2005;33:1757–63.
Roch A. Usefulness of ultrasonography in predicting pleural effusions >500 mL in patients receiving mechanical ventilation. Chest. 2005;127:224–32.
Diacon AH. Accuracy of pleural puncture sites: a prospective comparison of clinical examination with ultrasound. Chest. 2003;123:436–41.
• Duncan DR, Morgenthaler TI, Ryu JH, Daniels CE. Reducing iatrogenic risk in thoracentesis: establishing best practice via experiential training in a zero-risk environment. Chest. 2009;135:1315–20. This prospective study demonstrated that pleural intervention risk can be reduced using a training program for physicians, which included thoracic ultrasound.
Raptopoulos V, Davis LM, Lee G, et al. Factors affecting the development of pneumothorax associated with thoracentesis. AJR Am J Roentgenol. 1991;156:917–20.
Barnes TW, Morgenthaler TI, Olson EJ, et al. Sonographically guided thoracentesis and rate of pneumothorax. J Clin Ultrasound. 2005;33:442–6.
Yu CJ, Yang PC, Wu HD, et al. Ultrasound study in unilateral hemithorax opacification. Image comparison with computed tomography. Am Rev Respir Dis. 1993;147:430–4.
Hirsch JH, Rogers JV, Mack LA. Real-time sonography of pleural opacities. AJR Am J Roentgenol. 1981;136:297–301.
Yang PC, Luh KT, Chang DB, et al. Value of sonography in determining the nature of pleural effusion: analysis of 320 cases. AJR Am J Roentgenol. 1992;159:29–33.
Tu CY. Pleural effusions in febrile medical ICU patients: chest ultrasound study. Chest. 2004;126:1274–80.
Akhan O, Ozkan O, Akinci D, et al. Image-guided catheter drainage of infected pleural effusions. Diagn Interv Radiol. 2007;13:204–9.
Shankar S, Gulati M, Kang M, et al. Image-guided percutaneous drainage of thoracic empyema: can sonography predict the outcome? Eur Radiol. 2000;10:495–9.
Chen C-H, Chen W, Chen H-J, et al. Transthoracic ultrasonography in predicting the outcome of small-bore catheter drainage in empyemas or complicated parapneumonic effusions. Ultrasound Med Biol. 2009;35:1468–74.
Chen KY, Liaw YS, Wang HC, et al. Sonographic septation: a useful prognostic indicator of acute thoracic empyema. J Ultrasound Med. 2000;19:837–43.
Kearney SE, Davies CW, Davies RJ, Gleeson FV. Computed tomography and ultrasound in parapneumonic effusions and empyema. Clin Radiol. 2000;55:542–7.
Wrightson JM, Maskell NA. Thoracic ultrasound for beginners: utility and training issues for clinicians. Br J Hosp Med (Lond). 2011;72:325–30.
Wrightson JM, Fysh E, Maskell NA, Lee YC. Risk reduction in pleural procedures: sonography, simulation and supervision. Curr Opin Pulm Med. 2010;16:340–50.
• Raj V, Kirke R, Bankart MJ, Entwisle JJ. Multidetector CT imaging of pleura: comparison of two contrast infusion protocols. Br J Radiol. 2011;84:796–9. This paper discusses techniques for CT-based pleural imaging, particularly with reference to optimizing pleural enhancement and reduction of radiation dose..
Takasugi JE, Godwin JD, Teefey SA. The extrapleural fat in empyema: CT appearance. Br J Radiol. 1991;64:580–3.
Waite RJ, Carbonneau RJ, Balikian JP, et al. Parietal pleural changes in empyema: appearances at CT. Radiology. 1990;175:145–50.
Aquino SL, Webb WR, Gushiken BJ. Pleural exudates and transudates: diagnosis with contrast-enhanced CT. Radiology. 1994;192:803–8.
Stark DD, Federle MP, Goodman PC, et al. Differentiating lung abscess and empyema: radiography and computed tomography. AJR Am J Roentgenol. 1983;141:163–7.
Helm EJ, Matin TN, Gleeson FV. Imaging of the pleura. J Magn Reson Imaging. 2010;32:1275–86.
Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44 Suppl 2:S27–72.
Brook I, Frazier EH. Aerobic and anaerobic microbiology of empyema. A retrospective review in two military hospitals. Chest. 1993;103:1502–7.
Strachan RE, Jaffe A. Recommendations for managing paediatric empyema thoracis. Med J Aust. 2011;195:95.
Eastham KM, Freeman R, Kearns AM, et al. Clinical features, aetiology and outcome of empyema in children in the north east of England. Thorax. 2004;59:522–5.
Blaschke AJ, Heyrend C, Byington CL, et al. Molecular analysis improves pathogen identification and epidemiologic study of pediatric parapneumonic empyema. Pediatr Infect Dis J. 2011;30:289–94.
Wong CA, Donald F, Macfarlane JT. Streptococcus milleri pulmonary disease: a review and clinical description of 25 patients. Thorax. 1995;50:1093–6.
Ahmed RA, Marrie TJ, Huang JQ. Thoracic empyema in patients with community-acquired pneumonia. Am J Med. 2006;119:877–83.
Meyer CN, Rosenlund S, Nielsen J, Friis-Moller A. Bacteriological aetiology and antimicrobial treatment of pleural empyema. Scand J Infect Dis. 2011;43:165–9.
Lindstrom ST, Kolbe J. Community acquired parapneumonic thoracic empyema: predictors of outcome. Respirology. 1999;4:173–9.
Lin YC, Tu CY, Chen W, et al. An urgent problem of aerobic gram-negative pathogen infection in complicated parapneumonic effusions or empyemas. Intern Med. 2007;46:1173–8.
Civen R, Jousimies-Somer H, Marina M, et al. A retrospective review of cases of anaerobic empyema and update of bacteriology. Clin Infect Dis. 1995;20 Suppl 2:S224–9.
Chapman SJ, Davies RJ. The management of pleural space infections. Respirology. 2004;9:4–11.
Tu CY, Hsu WH, Hsia TC, et al. The changing pathogens of complicated parapneumonic effusions or empyemas in a medical intensive care unit. Intensive Care Med. 2006;32:570–6.
Mongkolrattanothai K, Aldag JC, Mankin P, Gray BM. Epidemiology of community-onset Staphylococcus aureus infections in pediatric patients: an experience at a Children’s Hospital in central Illinois. BMC Infect Dis. 2009;9:112.
Gonzalez BE, Rueda AM, Shelburne SA, et al. Community-associated strains of methicillin-resistant Staphylococccus aureus as the cause of healthcare-associated infection. Infect Control Hosp Epidemiol. 2006;27:1051–6.
Micek ST, Dunne M, Kollef MH. Pleuropulmonary complications of Panton-Valentine leukocidin-positive community-acquired methicillin-resistant Staphylococcus aureus: importance of treatment with antimicrobials inhibiting exotoxin production. Chest. 2005;128:2732–8.
Gonzalez BE, Hulten KG, Dishop MK, et al. Pulmonary manifestations in children with invasive community-acquired Staphylococcus aureus infection. Clin Infect Dis. 2005;41:583–90.
Thomas R, Ferguson J, Coombs G, Gibson PG. Community-acquired methicillin-resistant Staphylococcus aureus pneumonia: a clinical audit. Respirology. 2011;6:926–31.
Carrillo-Marquez MA, Hulten KG, Hammerman W, et al. Staphylococcus aureus pneumonia in children in the era of community-acquired methicillin-resistance at Texas Children’s Hospital. Pediatr Infect Dis J. 2011;30:545–50.
Schultz KD, Fan LL, Pinsky J, et al. The changing face of pleural empyemas in children: epidemiology and management. Pediatrics. 2004;113:1735–40.
Ferrer A, Osset J, Alegre J, et al. Prospective clinical and microbiological study of pleural effusions. Eur J Clin Microbiol Infect Dis. 1999;18:237–41.
• Strachan RE, Cornelius A, Neo PI, et al. Pleural fluid nucleic acid testing enhances Pneumococcal surveillance in children. Respirology 2011. In press. Examines the use of molecular techniques in childhood empyema to identify and serotype Streptococcus pneumoniae in culture-negative pleural fluid specimens.
Maataoui N, Bidet P, Doit C, et al. A multiplex polymerase chain reaction method for rapid pneumococcal serotype determination in childhood empyema. Diagn Microbiol Infect Dis. 2011;69:245–9.
Strachan RE, Cornelius A, Gilbert GL, et al. A bedside assay to detect streptococcus pneumoniae in children with empyema. Pediatr Pulmonol. 2011;46:179–83.
Martinon-Torres F, Dosil-Gallardo S, Perez Del Molino-Bernal ML, et al. Pleural antigen assay in the diagnosis of pediatric pneumococcal empyema. J Crit Care. 2011. In press.
Kee C, Palladino S, Kay I, et al. Feasibility of real-time polymerase chain reaction in whole blood to identify Streptococcus pneumoniae in patients with community-acquired pneumonia. Diagn Microbiol Infect Dis. 2008;61:72–5.
Lisboa T, Waterer G, Rello J. We should be measuring genomic bacterial load and virulence factors. Crit Care Med. 2010;38(10 Suppl):S656–62.
Munoz-Almagro C, Gala S, Selva L, et al. DNA bacterial load in children and adolescents with pneumococcal pneumonia and empyema. Eur J Clin Microbiol Infect Dis. 2011;30:327–35.
Light RW, MacGregor MI, Ball Jr WC, et al. Diagnostic significance of pleural fluid pH and Pco2. Chest. 1973;64:591–6.
Light RW, Girard WM, Jenkinson SG, et al. Parapneumonic effusions. Am J Med. 1980;69:507–11.
Skouras V, Awdankiewicz A, Light RW. What size parapneumonic effusions should be sampled? Thorax. 2010;65:91.
Disclosure
No potential conflicts of interest relevant to this article were reported.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tobin, C.L., Porcel, J.M., Wrightson, J.M. et al. Diagnosis of pleural infection: state-of-the-art. Curr Respir Care Rep 1, 101–110 (2012). https://doi.org/10.1007/s13665-012-0011-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-012-0011-3