Abstract
Objective
Nitric oxide (NO) and inducible nitric oxide synthase enzyme (iNOS) have been implicated in various tumors. Hepatocellular carcinoma is a highly aggressive form of solid tumor. The lack of effective therapy necessitates the introduction of novel therapeutic strategies to counter this disease. Nigella sativa (NS) has been shown to have specific health benefits. The aim of this study was to investigate the in vivo modulation of the iNOS pathway by NS ethanolic extract (NSEE) and the implications of this effect as an antitumor therapeutic approach against diethylnitrosamine (DENA)-induced hepatocarcinogenesis.
Methods
Rats were divided into four groups, normal control, NSEE control, cancer control, and NSEE-DENA groups. The diagnosis of cancer was based on alpha-fetoprotein (AFP) levels and histological variations. Serum NO, tumor necrosis factor-α (TNF-α), and interleukin-6 (IL-6) levels and serum iNOS activity were measured. Liver iNOS expression was investigated by reverse transcriptase (RT)-PCR and western blot assays.
Results
Serum AFP, NO, TNF-α, and IL-6 levels and iNOS enzyme activity were significantly increased in rats treated with DENA. Significant up-regulation of liver iNOS mRNA and protein expression was also observed. Subsequent treatment with NSEE significantly reversed these effects and improved the histopathological changes in malignant liver tissue which appeared after treatment with DENA, without any toxic effect when given alone.
Conclusion
These results provide evidence that attenuation of the iNOS pathway and suppression of the inflammatory response mediated by TNF-α, and IL-6 could be implicated in the antitumor effect of NSEE. As such, our findings hold great promise for the utilization of NS as an effective natural therapeutic agent in the treatment of hepatocarcinogenesis.
Similar content being viewed by others
Introduction
Nitric oxide (NO), a membrane permeable gaseous radical and an important cellular second messenger that is produced by three NO synthase (NOS) isoforms [inducible (iNOS), endothelial (eNOS) and neuronal (nNOS)], has been postulated to mediate numerous physiological and pathophysiological processes [1–3]. It plays an important role as a redox-based signaling mediator, modulating enzyme activities, signal transductions, and cytokine networks and also produces reactive nitrogen species (RNS). RNS cause the aberrant S-nitrosylation of proteins, DNA damage, as well as lipid peroxidation, apoptosis, and necrosis [4, 5].
NO, which is produced by iNOS during inflammation and overexpressed in neoplastic lesions, is also an endogenous candidate molecule involved in the predisposition to cancer [6–9]. Induction of gene alterations by NO through DNA damage, mutations, inhibition of DNA repair, and effects on p53, together with activation of DNA methyltransferase might thereby be important in studies on cancer. NO can also inhibit caspases and lymphocyte proliferation, activate telomerase and matrix metalloproteinases, and induce vascular permeability and pro-angiogenic factors, thus impacting on apoptosis, angiogenesis, cell migration, and invasion [6, 8, 10, 11].
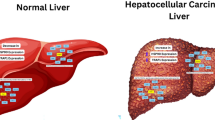
Hepatocellular carcinoma (HCC) is one of the most frequently occurring forms of a solid tumor, with a high prevalence of 620,000 cases per year reported worldwide [12]. It is highly aggressive, as shown by the mortality of 595,000 cases per year, a mortality rate that nearly matches the incidence of this tumor type [13]. At the present time, there is a limited number of therapeutic options for HCC patients. Hence, a thorough understanding of the biological bases of this malignancy might be the first step in developing new strategies for effective treatment [14]. iNOS is known to be overexpressed in HCC [15, 16], and in the livers of patients with hepatitis, fibrosis, and cirrhosis [17–21]. Epidemiological studies have shown that inflammation predisposes to certain cancers and that most cancerous tissues show signs of inflammation, in association with specific inflammatory signaling molecules (i.e., cytokines), remodeling, and angiogenesis. It has also been shown that cancer-associated inflammation actually promotes tumor growth and progression [22, 23]. Several pro-inflammatory gene products [i.e., tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6)] play a critical role in apoptosis, proliferation, angiogenesis, invasion, and metastasis. Their expression is mainly regulated by nuclear factor kappa-B, which is constitutively active in most tumors and induced by chemotherapeutic agents and carcinogens [24]. Although improper up-regulation of iNOS and pro-inflammatory cytokines has been linked to the pathophysiology of certain cancers [25–32], the involvement of iNOS in hepatocarcinogenesis remains largely unclear.
On account of the high morbidity and mortality of cancer diseases, the problems encountered in their treatment, and the toxic effects of cancer chemotherapy, various attempts have been made to investigate the anticancer effects of relatively safe edible herbs [33]. One of these herbs is Nigella sativa (NS). NS seed has long been an important natural remedy for many ailments in ancient systems of medicine (e.g. Unani, Ayurveda, Chinese, and Arabic medicines), and many active components have been isolated from this herb. The pharmacological effects of NS seed, its oil, various extracts, and active components have been identified to include stimulation of the immune system and anti-inflammation, hypoglycemic, antihypertensive, antiasthmatic, antimicrobial, antiparasitic, antioxidant, and anticancer effects [34, 35]. However, only a few authors have reviewed the medicinal properties of NS and reported on its anticancer effects. Toxicity studies have recently confirmed the safety of NS oil and its most abundant active component, thymoquinone [34, 36–38].
The molecular effect of thymoquinone and NS oil on the iNOS pathway in lung and testicular injuries has recently been shown [39–43], but to date the molecular effect of NS seed extracts on that pathway has not been investigated. Here we report our study on the in vivo molecular mechanism underlying the antitumor properties of NS ethanolic extract (NSEE) through the modulation of the iNOS pathway against diethylnitrosamine (DENA)-induced hepatocarcinogenesis. To this end we examined the effects of NSEE on DENA-stimulated increased alpha-fetoprotein (AFP), NO, TNF-α, and IL-6 levels, as well as the effects of NSEE on iNOS activity and expression.
Materials and methods
Animals
Animal care and experimental protocols were performed in accordance with the guidelines established by the Research Ethics Committee of the Experimental Animal Center, University of Toyama. In total, we used 32 male Wistar rats (weight 160 ± 5 g) which were maintained on a standard rodent diet and water ad libitum. The rats were housed in polyethylene cages in a humid room under a controlled light regime of 12 h light and 12 h dark for 2 weeks before the experiment.
Chemicals
All chemicals were of analytical grade and came from local suppliers.
NS ethanolic extract
Nigella sativa seeds (Kahira Pharmaceuticals and Chemical Industries Co., Cairo, Egypt) were washed, dried, and then ground to powder using an electric micronizer (Jiangyin Hongke Shredder Machinery Co., Jiangsu, China). The powder was extracted three times with 80 % ethanol and the solvent evaporated at 40 °C under reduced pressure. This procedure resulted in a two-phased extract. The oily and solid phases were recombined in proportion to their yield (typically 70 and 30 %, respectively). The NSEE was stored at 4 °C and protected from light and humidity.
Experimental design
The rats were divided into four equally sized groups (8 rats/group). Rats in the normal control group were given normal saline 0.5 ml by gavage daily for 5 consecutive days and received a single intraperitoneal (i.p.) injection of normal saline (2.5 ml/kg) on day 3. Rats in the NSEE control group were given NSEE 250 mg/kg orally by gavage daily for 5 consecutive days [44]. Rats in the cancer control group were given the same doses of normal saline as the normal control group (0.5 ml) for 3 consecutive days before and 2 days after a single i.p. dose of DENA (Sigma Chemical Co., St. Louis, MO) 200 mg/kg in saline [45]. Rats in the NSEE-DENA group received the same doses of NSEE as the NSEE control group (250 mg/kg) for 3 consecutive days before and 2 days after a single i.p. dose of DENA (200 mg/kg). Fourteen weeks after the administration of DENA, the animals were fasted overnight, then weighed and killed by exposure to an increasing concentration of CO2. Blood samples were obtained by cardiac puncture, left to clot for 1 h at 37 °C, then centrifuged at 10,000 rpm at 4 °C to separate out the serum samples which were kept at −80 °C for further use.
Liver samples were quickly removed, washed in ice-cold phosphate buffered saline (PBS) and desiccated. Individual liver weights were recorded. The liver was cut into portions for subsequent studies. The portion intended for histological examination was kept in 10 % buffered formalin. A second portion was either frozen in liquid nitrogen and stored at −80 °C for further use or homogenized in 0.25 mM sucrose, 10 mM Tris, 1 mM ethylene diamine tetraacetic acid (EDTA) (pH 7.4), and 1 % protease inhibitor cocktail (Boehringer Mannheim, Indianopolis, IN). The liver homogenates were centrifuged at 4,000 rpm for 15 min at 4 °C and the supernatant collected; total protein in the supernatant was determined. For biochemical investigations, samples were distributed into aliquots in Eppendorf tubes and kept at −80 °C.
Serum AFP, TNF-α, and IL-6 measurements
Samples were analyzed in triplicate. AFP serum levels were determined using the UBI MAGIWEL™ AFP CM-101 assay, a highly sensitive enzyme-linked immunosorbent assay (ELISA) kit (United Bioresearch, Sunnyvale, CA) following the recommendations of the manufacturer. TNF-α and IL-6 serum levels were determined using highly sensitive ELISA kits from R&S Systems (Minneapolis, MN) according to the manufacturer’s recommendations.
Serum NO measurement
The NO stable end products nitrite + nitrate (NO x ) were measured in serum using the Total Nitric Oxide Assay kit (Thermo Scientific, Rock Ford, IL). In brief, after nitrate had been reduced by 0.25 % vanadium(III) chloride in 0.5 M HCl, a 100-μl sample was mixed with 100 μl of Griess reagent [mixture of equal amounts of A (1 % sulphanilamide) and B (0.1 % naphthylethylene diamine dihydrochloride in 5 % H3PO4)] followed by incubation for 10 min at room temperature. Absorbance at 540 nm was measured, and the NO levels were calculated by using a standard calibration curve prepared from different concentrations of sodium nitrite. Standards were analyzed in triplicate.
Serum iNOS enzymatic activity assay
Serum iNOS enzymatic activities were measured using the Mouse iNOS ELISA kit from ElAab (Wuhan ElAab Science Co., Wuhan, China) according to the manufacturer’s instructions. In this kit, a monoclonal antibody specific for iNOS has been pre-coated onto a microplate. Standards and samples are pipetted into the wells, and any iNOS present is bound by the immobilized antibody. An enzyme-linked polyclonal antibody specific for iNOS is then added to the wells. Following a wash to remove any unbound antibody–enzyme reagent, a substrate solution is added to the wells and color develops in proportion to the amount of iNOS bound in the initial step. The color development is then stopped and absorbance at 450 nm measured. In our study we used an HTS Multi-Mode Microplate Reader (BioTek Instruments, Winooski, VT) to measure absorbance, and enzymatic activities of the different groups were expressed relative to those of the normal control group.
RNA isolation, cDNA synthesis, and reverse transcription-PCR for iNOS mRNA
Total RNA was extracted from frozen mouse livers using Isogen (Nippon Gene, Tokyo, Japan) according to the manufacturer’s instructions. Aliquots of 1 μg of total RNA were treated with 0.1 U/μl deoxyribonuclease I (DNase I; Sigma-Aldrich) at room temperature for 15 min. cDNAs were synthesized using 0.5 μg DNase I-treated RNA by using a Rever Tra Ace qPCR RT kit (TOYOBO Co., Osaka, Japan) according to the manufacturer’s instructions. The resulting cDNA was subjected to PCR using a Taq DNA polymerase kit (QIAGEN, Hilden, Germany). PCR cycling was performed in a 25-μl reaction mixture and consisted of one cycle of 70 s at 95 °C, 25 cycles of 55 s at 93 °C, 45 s at 61 °C, and 40 s at 72 °C, and one cycle of 100 s at 72 °C, according to the manufacturer’s instructions for the thermal cycler (Gene Amp PCR System 2700; Applied Biosystems, Foster City, CA). The primers (Invitrogen, Carlsbad, CA) used were: mouse iNOS (835 bp; forward 5′-CAACCAGTATTATGGCTCCT-3′, reverse 5′-GTGACAGCCCGGTCTTTCCA-3′) and mouse β-actin (840 bp; forward 5′-GGAGAAGATCTGGCACCACACC-3′, reverse 5′-CCTGCTTGCTGATCCACATCTGCTGG-3′). The β-actin primer was used as an internal control. PCR products were separated by electrophoresis in 2 % agarose gels containing 0.1 μg/ml ethidium bromide. Digital images were captured by LAS-3000 (Fujifilm, Tokyo, Japan) and Multi-Gauge v3.0 software (Fujifilm). Bands corresponding to iNOS of the different groups were analyzed densitometrically relative to the normal control group using Image J software. Data were normalized to the corresponding internal control β-actin mRNA bands.
Western blot assay of iNOS protein expression
Samples containing 50 μg of protein were separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (12–14 % acrylamide) and transferred onto polyvinylidene fluoride membranes (Millipore, Bedford, MA). Nonspecific binding was blocked by preincubation of the membranes in PBS containing 3–5 % nonfat dried milk for 30 min at 37 °C. The membranes were then incubated overnight at 4 °C with rabbit polyclonal anti-iNOS antibody (1:1000; Santa Cruz Biotechnology, Santa Cruz, CA). Bound primary antibody was detected using a horseradish peroxidase-conjugated antirabbit secondary antibody (Dako, Glostrup, Denmark) by chemiluminescence using an enhanced chemiluminescence kit (GE Healthcare, Little Chalfont, UK) according to the manufacturer’s instructions. Immunoreactive proteins were visualized using a luminescent image analyzer (LAS-4000; Fujifilm Co.). Glyceraldehyde 3-phosphate dehydrogenase (GAPDH; Santa Cruz Biotechnology) was used (1:1000) as a loading control to ensure equal loading and even transfer from the gel to the membrane across the whole gel. Bands corresponding to iNOS protein of the different groups were analyzed densitometrically, using Image J Software, relative to the normal control group. Data were normalized to GAPDH levels. Electrophoresis and electroblotting were carried out in a Bio-Rad Trans-Blot SD Cell apparatus (Bio-Rad, Hercules, CA) using a discontinuous buffer system.
Histological examination
For histological examination, a piece of the liver was fixed by immersion in 10 % buffered formalin for 24 h. The blocks were dehydrated in a graded series of ethanol and embedded in Paraffin wax. Serial 4-μm-thick sections were stained with hematoxylin and eosin (H&E) stain.
Statistical analysis
All results were expressed as mean ± standard deviation of n = 8 rats. Statistical comparison was conducted using Student’s t test after one-way analysis of variance (ANOVA) using GraphPad Prism 5 statistical software (GraphPad, La Jolla, CA) and Excel software (Microsoft, Redwood, WA). The results were considered to be significant when the probability values (P) were <0.05.
Results
Serum AFP level
Serum AFP levels were measured as an indicator of cancer incidence. As shown in Table 1, animals treated with NSEE showed non-significant changes in serum AFP levels, while animals treated with DENA (cancer group) showed significantly (P < 0.001) higher serum levels of AFP when compared to their counterparts in the normal control group. The treatment of rats which had developed cancer with NSEE (NSEE-DENA group) significantly (P < 0.001) reduced serum AFP levels compared to rats treated only with DENA.
Serum levels of the pro-inflammatory cytokines (TNF-α and IL-6)
The level of the pro-inflammatory cytokines TNF-α and IL-6 in the serum was determined by appropriate ELISA assay according to the manufacturer’s instructions. As shown in Table 1, the administration of DENA significantly (P < 0.001) increased the serum levels of both pro-inflammatory cytokines in rats of the cancer control group relative to those of the normal control group; this increase was significantly (P < 0.001) reversed in the rats of the NSEE-DENA group. Rats treated with NSEE alone did not show any significant changes in their serum levels compared to the normal control group rats.
Serum levels of the pro-inflammatory mediator NO
The serum levels of the NO stable end products were estimated, and the results are shown in Fig. 1. NO serum levels were significantly (P < 0.001) increased in rats treated with DENA, but did not significantly change in those treated with NSEE when compared to those in the normal control group animals. The serum level of this pro-inflammatory mediator was significantly reduced in rats in the NSEE-DENA group (P < 0.001) compared the cancer control group rats.
Serum levels of the pro-inflammatory mediator nitric oxide. Serum levels are expressed relative to those of the normal control group. Bars Mean ± standard deviation (SD), n = 8. Significant differences between groups are analyzed by one-way analysis of variance (ANOVA). *P < 0.001 compared to normal control group, § P < 0.001 compared to cancer control group, ns non-significant (P > 0.05) compared to normal control group. NSEE Nigella sativa ethanolic extract, DENA diethylnitrosamine. See Materials and methods subsection Experimental design for a detailed description of the animal groups
iNOS enzymatic activity
The inhibitory effect of NSEE on the activity of serum iNOS enzyme was also examined. Figure 2 shows that DENA significantly (P < 0.001) elevated the enzymatic activity of iNOS in the cancer control rats while NSEE did not elevate iNOS enzymatic activity, when compared to iNOS activity in normal control rats. More interestingly, iNOS enzyme activity in rats in the NSEE-DENA group was significantly (P < 0.001) reduced when compared that in the cancer control group rats.
Serum inducible nitric oxide synthase (iNOS) enzymatic activity. Enzymatic activities of the different groups are expressed relative to that of the normal control group. Bars Mean ± SD, n = 8. Significant differences between groups are analyzed by one-way ANOVA test. *P < 0.001 compared to normal control group, § P < 0.001 compared to cancer control group, ns non-significant (P > 0.05) compared to normal control group
Liver iNOS mRNA expression
Liver tissues from rats of different groups were investigated for their iNOS mRNA expression by reverse transcription (RT)-PCR (Fig. 3a). When the iNOS bands of the different groups were densitometrically analyzed relative to the normal control group and normalized to β-actin levels, iNOS mRNA expression in the cancer control group was found to be significantly (P < 0.001) elevated compared to that of normal control group. Surprisingly, iNOS mRNA expression in NSEE control rats and NSEE-DENA rats were significantly (P < 0.001) reduced compared to that of normal control and cancer control rats, respectively, as shown in Fig. 3b.
Liver iNOS mRNA expression. a Representative reverse transcription (RT)-PCR photographs for the different groups. b Relative expression of iNOS mRNA of the different groups is expressed densitometrically as a percentage of that of the normal control group using the bands in a. Expression was normalized to that of the corresponding internal control β-actin mRNA. Bars Mean ± SD, n = 8. Significant differences between groups are analyzed by one-way ANOVA, where *P < 0.001 compared to the normal control group, § P < 0.001 compared to the cancer control group
Liver iNOS protein expression
Nigella sativa ethanolic extract is known to down-regulate NO production induced by DENA. Because NO overproduction is always associated with the up-regulation of iNOS protein expression, we examined iNOS protein expression by the liver by western blot (Fig. 4a). The densities of bands corresponding to the iNOS protein were normalized on the basis of GAPDH and analyzed relative to that of the normal control group, as shown in Fig. 4b. The administration of DENA significantly (P < 0.01) up-regulated liver iNOS protein expression in the cancer group rats, while NSEE significantly (P < 0.001) down-regulated its expression, when compared to the normal control group rats. Also, iNOS protein expression in the liver of NSEE-DENA rats was significantly (P < 0.001) reduced when compared to that of cancer control rats.
Liver iNOS protein expression. a Representative immunoprecipitation blots of iNOS protein expressed in the liver of rats in the different groups. b Relative expression of iNOS protein by the different groups expressed densitometrically as a percentage of that of the normal control group using the bands in a. Expression was normalized to the expression of the corresponding internal control glyceraldehyde 3-phosphate dehydrogenase (GAPDH). Bars Mean ± SD, n = 8. Significant differences between groups are analyzed by one-way ANOVA, where: *P < 0.01 compared to normal control group, **P < 0.001 compared to normal control group, § P < 0.001 compared to cancer control group
Liver histological examination
The liver tissue was examined histologically using H&E staining, and serum AFP levels were used as an indicator of cancer incidence. Histological examination of the liver normal control animals (Fig. 5a) revealed normal cells with granulated cytoplasm and small, uniform nuclei, as well as normal sinusoids and normal architecture, while no obvious changes were observed in livers of NSEE animals (Fig. 5b). Liver sections of cancer control rats (Fig. 5c) showed a loss of normal architecture, enlargement of sinusoids, focal areas of necrosis, and irregularly shaped neoplastic hepatocytes with polymorphic and hyperchromatic nuclei. These changes were observed to be reduced in liver sections of NSEE-DENA rats, indicating a certain degree of improvement (Fig. 5d).
Histological examination of the livers of animals in all groups. a–d Representative photomicrographs of livers of normal control rats (a), NSEE control rats (b), cancer control rats (c), and NSEE-DENA rats (d). Hematoxylin and eosin staining revealed normal architecture and normal cells with granulated cytoplasm and uniform nuclei in liver sections of normal control and NSEE control rats. Loss of normal architecture, enlargement of sinusoids, and irregularly shaped neoplastic hepatocytes with polymorphic and hyperchromatic nuclei were observed in liver sections of cancer control rats (arrows), while these changes were reduced in NSEE-DENA rats with few neoplastic hepatocytes. Magnification ×200
Discussion
The precise role of NO in tumor pathophysiology has been the focus of numerous studies, with particular emphasis on its involvement in a multitude of inter- and intra-cellular signaling pathways that are crucial to the malignant character of cancer. It is not surprising that in heterogeneous tumors, a variety of responses have been observed following modification of NO levels [46]. iNOS has been implicated in different stages of cellular changes that lead to malignancy, growth of transformed cells, angiogenesis, and metastasis of malignant cells. Up-regulation of iNOS expression can be observed in a variety of human malignant tumors, such as breast, lung, prostate, bladder, colon, gastric, and malignant melanoma [10, 25–28, 30–32, 47–49]. Further studies are required to determine the role of the iNOS pathway in tumorigenesis and to establish the utility of iNOS inhibitors as chemoprevention agents. In fact, specific iNOS inhibitors and iNOS gene ablation have been demonstrated to prevent colon and lung carcinogenesis in rats [50–52]. Nevertheless, an enhancement of colon lesion development with iNOS gene ablation was reported in one case [53], and thus the involvement of iNOS in this and other organs remains controversial [6, 7].
Hepatocarcinogenesis induced by DENA is an ideal animal model to investigate liver tumor formation because it proceeds in stages similar to that of human liver cancer—i.e., formation of preneoplastic foci, neoplastic nodules, and HCC nodules [54, 55]. In our study, liver carcinogenesis was induced chemically by DENA, a well-known hepatic cancer model in which serum AFP level is highly elevated and hepatocarcinogenesis can be histopathologically identified [45, 56, 57]. Serum AFP levels and liver histological examination were used as indicators of cancer incidence. Our data show that animals treated with DENA alone had elevated serum AFP levels and definite histological changes reflecting severe hepatocellular damage. AFP is always used to assess and follow up both HCC diagnostically and prognostically [24]. In our study we investigated the in vivo modulation of the iNOS pathway by NSEE and the implication of this effect as an antitumor pathway against hepatocarcinogenesis induced by DENA.
Our data reveal that the administration of NSEE alone did not significantly affect the biochemical parameters studied (AFP, TNF-α, IL-6, and NO) or change the liver histological examination. Furthermore, NSEE significantly down-regulated the expression of iNOS. More interestingly, we found no significant changes in the body weights or hepatosomatic indices of rats treated with NSEE alone (data not shown), suggesting the great safety of this extract. These results are in accordance with those reported earlier [58, 59]. NSEE also significantly down-regulated the elevation of serum AFP levels and reduced the histopathological changes caused by DENA in the livers of the rats. These anti-neoplastic effects have been confirmed by others in different models [60–64].
The inhibitory effect of NS oil and thymoquinone on pro-inflammatory cytokines release and iNOS activation has been proved in lung and testicular injuries, but there is nothing about the effect of NSEE [39–43].
Overproduction of the inflammatory mediators (NO, TNF-α, and IL-6) and stimulation of iNOS enzyme activity and expression have been reported in DENA-induced hepatocarcinogenesis [55, 64, 65]. In our study, NSEE blocked DENA-induced various responses in rats, including NO overproduction, the release of pro-inflammatory cytokines (TNF-α and IL-6), and the stimulation of both iNOS enzymatic activity and expression. Overall, our results suggest that NSEE (which contains natural constituents, such as thymoquinone, alpha-hederin, quercetin, and kaempferol) prevented DENA-induced hepatocarcinogenesis in rats through the inhibition of the iNOS pathway. Various other studies have reported that iNOS pathway inhibition may result in an antineoplastic effect [28, 31, 47, 55, 64].
In conclusion, the results of our investigation provide evidence that attenuation of iNOS pathway and suppression of the inflammatory response mediated by TNF-α and IL-6 could be implicated, in part, in the antitumor effect of NS. Consequently, our findings hold great promise for the utilization of NS as an effective natural therapeutic agent in the treatment of liver cancer.
References
Alderton WK, Cooper CE, Knowles RG. Nitric oxide synthases: structure, function and inhibition. Biochem J. 2001;357:593–615.
Schwentker A, Vodovotz Y, Weller R, Billiar TR. Nitric oxide and wound repair: role of cytokines? Nitric Oxide. 2002;7:1–10.
Stamler JS, Lamas S, Fang FC. Nitrosylation. The prototypic redox-based signaling mechanism. Cell. 2001;106:675–83.
Dedon PC, Tannenbaum SR. Reactive nitrogen species in the chemical biology of inflammation. Arch Biochem Biophys. 2004;423:12–22.
Ohshima H, Tatemichi M, Sawa T. Chemical basis of inflammation-induced carcinogenesis. Arch Biochem Biophys. 2003;417:3–11.
Crowell JA, Steele VE, Sigman CC, Fay JR. Is inducible nitric oxide synthase a target for chemoprevention? Mol Cancer Ther. 2003;2:815–23.
Hofseth LJ, Hussain SP, Wogan GN, Harris CC. Nitric oxide in cancer and chemoprevention. Free Radic Biol Med. 2003;34:955–68.
Jaiswal M, LaRusso NF, Gores GJ. Nitric oxide in gastrointestinal epithelial cell carcinogenesis: linking inflammation to oncogenesis. Am J Physiol Gastrointest Liver Physiol. 2001;281:G626–34.
Wu J, Akaike T, Hayashida K, Okamoto T, Okuyama A, Maeda H. Enhanced vascular permeability in solid tumor involving peroxynitrite and matrix metalloproteinases. Jpn J Cancer Res. 2001;92:439–51.
Aurello P, Rossi Del Monte S, D’Angelo F, Cicchini C, Ciardi A, Bellagamba R, et al. Vascular endothelial growth factor C and microvessel density in gastric carcinoma: correlation with clinicopathological factors. Our experience and review of the literature. Oncol Res. 2009;17:405–11.
Ishii Y, Ogura T, Tatemichi M, Fujisawa H, Otsuka F, Esumi H. Induction of matrix metalloproteinase gene transcription by nitric oxide and mechanisms of MMP-1 gene induction in human melanoma cell lines. Int J Cancer. 2003;103:161–8.
Ribes J, Cleries R, Esteban L, Moreno V, Bosch FX. The influence of alcohol consumption and hepatitis B and C infections on the risk of liver cancer in Europe. J Hepatol. 2008;49:233–42.
Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94:153–6.
D’Alessandro N, Poma P, Montalto G. Multifactorial nature of hepatocellular carcinoma drug resistance: could plant polyphenols be helpful? World J Gastroenterol. 2007;13:2037–43.
Ikeguchi M, Ueta T, Yamane Y, Hirooka Y, Kaibara N. Inducible nitric oxide synthase and survivin messenger RNA expression in hepatocellular carcinoma. Clin Cancer Res. 2002;8:3131–6.
Rahman MA, Dhar DK, Yamaguchi E, Maruyama S, Sato T, Hayashi H, et al. Coexpression of inducible nitric oxide synthase and COX-2 in hepatocellular carcinoma and surrounding liver: possible involvement of COX-2 in the angiogenesis of hepatitis C virus-positive cases. Clin Cancer Res. 2001;7:1325–32.
Mohammed NA, Abd El-Aleem S, Appleton I, Maklouf MM, Said M, McMahon RF. Expression of nitric oxide synthase isoforms in human liver cirrhosis. J Pathol. 2003;200:647–55.
Gardner CR, Laskin JD, Dambach DM, Sacco M, Durham SK, Bruno MK, et al. Reduced hepatotoxicity of acetaminophen in mice lacking inducible nitric oxide synthase: potential role of tumor necrosis factor-alpha and interleukin-10. Toxicol Appl Pharmacol. 2002;184:27–36.
McKim SE, Gabele E, Isayama F, Lambert JC, Tucker LM, Wheeler MD, et al. Inducible nitric oxide synthase is required in alcohol-induced liver injury: studies with knockout mice. Gastroenterology. 2003;125:1834–44.
Sanz-Cameno P, Medina J, Garcia-Buey L, Garcia-Sanchez A, Borque MJ, Martin-Vilchez S, et al. Enhanced intrahepatic inducible nitric oxide synthase expression and nitrotyrosine accumulation in primary biliary cirrhosis and autoimmune hepatitis. J Hepatol. 2002;37:723–9.
Wei CL, Khoo HE, Lee KH, Hon WM. Differential expression and localization of nitric oxide synthases in cirrhotic livers of bile duct-ligated rats. Nitric Oxide. 2002;7:91–102.
Balkwill F. Tumor necrosis factor or tumor promoting factor? Cytokine Growth Factor Rev. 2002;13:135–41.
Balkwill F, Charles KA, Mantovani A. Smoldering and polarized inflammation in the initiation and promotion of malignant disease. Cancer Cell. 2005;7:211–7.
Aggarwal BB, Shishodia S, Sandur SK, Pandey MK, Sethi G. Inflammation and cancer: how hot is the link? Biochem Pharmacol. 2006;72:1605–21.
Aviello G, Romano B, Borrelli F, Capasso R, Gallo L, Piscitelli F, et al. Chemopreventive effect of the non-psychotropic phytocannabinoid cannabidiol on experimental colon cancer. J Mol Med (Berl). 2012. doi:10.1007/s00109-011-0856-x.
Huang FY, Chan AO, Rashid A, Wong DK, Cho CH, Yuen MF. Helicobacter pylori induces promoter methylation of E-cadherin via interleukin-1beta activation of nitric oxide production in gastric cancer cells. Cancer. 2012;118:4969–80.
Li CF, Fang FM, Wang JM, Tzeng CC, Tai HC, Wei YC, et al. EGFR nuclear import in gallbladder carcinoma: nuclear phosphorylated EGFR upregulates iNOS expression and confers independent prognostic impact. Ann Surg Oncol. 2012;19:443–54.
Li TW, Yang H, Peng H, Xia M, Mato JM, Lu SC. Effects of S-adenosylmethionine and methylthioadenosine on inflammation-induced colon cancer in mice. Carcinogenesis. 2012;33:427–35.
Ma N, Thanan R, Kobayashi H, Hammam O, Wishahi M, El Leithy T, et al. Nitrative DNA damage and Oct3/4 expression in urinary bladder cancer with Schistosoma haematobium infection. Biochem Biophys Res Commun. 2011;414:344–9.
Murata M, Thanan R, Ma N, Kawanishi S. Role of nitrative and oxidative DNA damage in inflammation-related carcinogenesis. J Biomed Biotechnol. 2012;2012:623019.
Piplani H, Vaish V, Sanyal SN. Dolastatin 15, a mollusk linear peptide, and Celecoxib, a selective cyclooxygenase-2 inhibitor, prevent preneoplastic colonic lesions and induce apoptosis through inhibition of the regulatory transcription factor NF-kappaB and an inflammatory protein, iNOS. Eur J Cancer Prev. 2012;21:511–22.
Vaish V, Sanyal SN. Role of Sulindac and Celecoxib in the regulation of angiogenesis during the early neoplasm of colon: exploring PI3-K/PTEN/Akt pathway to the canonical Wnt/beta-catenin signaling. Biomed Pharmacother. 2012;66:354–67.
Abdel-Hamid NM, El-Moselhy MA, El-Baz A. Hepatocyte lysosomal membrane stabilization by olive leaves against chemically induced hepatocellular neoplasia in rats. Int J Hepatol. 2011;2011:736581.
Randhawa MA, Alghamdi MS. Anticancer activity of Nigella sativa (black seed)—a review. Am J Chin Med. 2011;39:1075–91.
Ashraf SS, Rao MV, Kaneez FS, Qadri S, Al-Marzouqi AH, Chandranath IS, et al. Nigella sativa extract as a potent antioxidant for petrochemical-induced oxidative stress. J Chromatogr Sci. 2011;49:321–6.
Ali BH, Blunden G. Pharmacological and toxicological properties of Nigella sativa. Phytother Res. 2003;17:299–305.
Salem ML. Immunomodulatory and therapeutic properties of the Nigella sativa L. seed. Int Immunopharmacol. 2005;5:1749–70.
Padhye S, Banerjee S, Ahmad A, Mohammad R, Sarkar FH. From here to eternity—the secret of Pharaohs: therapeutic potential of black cumin seeds and beyond. Cancer Ther. 2008;6:495–510.
el Ammar SM, Gameil NM, Shawky NM, Nader MA. Comparative evaluation of anti-inflammatory properties of thymoquinone and curcumin using an asthmatic murine model. Int Immunopharmacol. 2011;11:2232–6.
Ibrahim ZS, Ishizuka M, Soliman M, ElBohi K, Sobhy W, Muzandu K, et al. Protection by Nigella sativa against carbon tetrachloride-induced downregulation of hepatic cytochrome P450 isozymes in rats. Jpn J Vet Res. 2008;56:119–28.
Kanter M. Effects of Nigella sativa seed extract on ameliorating lung tissue damage in rats after experimental pulmonary aspirations. Acta Histochem. 2009;111:393–403.
Kanter M. Thymoquinone attenuates lung injury induced by chronic toluene exposure in rats. Toxicol Ind Health. 2011;27:387–95.
Kanter M. Thymoquinone reestablishes spermatogenesis after testicular injury caused by chronic toluene exposure in rats. Toxicol Ind Health. 2011;27:155–66.
Michel CG, El-Sayed NS, Moustafa SF, Ezzat SM, Nesseem DI, El-Alfy TS. Phytochemical and biological investigation of the extracts of Nigella sativa L. seed waste. Drug Test Anal. 2011;3:245–54.
Sayed-Ahmed MM, Aleisa AM, Al-Rejaie SS, Al-Yahya AA, Al-Shabanah OA, Hafez MM, et al. Thymoquinone attenuates diethylnitrosamine induction of hepatic carcinogenesis through antioxidant signaling. Oxid Med Cell Longev. 2010;3:254–61.
Singh S, Gupta AK. Nitric oxide: role in tumour biology and iNOS/NO-based anticancer therapies. Cancer Chemother Pharmacol. 2011;67:1211–24.
Giantonio BJ, Catalano PJ, Meropol NJ, O’Dwyer PJ, Mitchell EP, Alberts SR, et al. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007;25:1539–44.
Ichinoe M, Mikami T, Shiraishi H, Okayasu I. High microvascular density is correlated with high VEGF, iNOS and COX-2 expression in penetrating growth-type early gastric carcinomas. Histopathology. 2004;45:612–8.
Nakamura Y, Yasuoka H, Tsujimoto M, Yang Q, Tsukiyama A, Imabun S, et al. Clinicopathological significance of vascular endothelial growth factor-C in breast carcinoma with long-term follow-up. Mod Pathol. 2003;16:309–14.
Ahn B, Ohshima H. Suppression of intestinal polyposis in Apc(Min/+) mice by inhibiting nitric oxide production. Cancer Res. 2001;61:8357–60.
Kisley LR, Barrett BS, Bauer AK, Dwyer-Nield LD, Barthel B, Meyer AM, et al. Genetic ablation of inducible nitric oxide synthase decreases mouse lung tumorigenesis. Cancer Res. 2002;62:6850–6.
Rao CV, Indranie C, Simi B, Manning PT, Connor JR, Reddy BS. Chemopreventive properties of a selective inducible nitric oxide synthase inhibitor in colon carcinogenesis, administered alone or in combination with celecoxib, a selective cyclooxygenase-2 inhibitor. Cancer Res. 2002;62:165–70.
Scott DJ, Hull MA, Cartwright EJ, Lam WK, Tisbury A, Poulsom R, et al. Lack of inducible nitric oxide synthase promotes intestinal tumorigenesis in the Apc(Min/+) mouse. Gastroenterology. 2001;121:889–99.
Boyault S, Rickman DS, de Reynies A, Balabaud C, Rebouissou S, Jeannot E, et al. Transcriptome classification of HCC is related to gene alterations and to new therapeutic targets. Hepatology. 2007;45:42–52.
Khan MS, Halagowder D, Devaraj SN. Methylated chrysin induces co-ordinated attenuation of the canonical Wnt and NF-κB signaling pathway and upregulates apoptotic gene expression in the early hepatocarcinogenesis rat model. Chem Biol Interact. 2011;193:12–21.
Iddamaldeniya SS, Thabrew MI, Wickramasinghe SM, Ratnatunge N, Thammitiyagodage MG. A long-term investigation of the anti-hepatocarcinogenic potential of an indigenous medicine comprised of Nigella sativa, Hemidesmus indicus and Smilax glabra. J Carcinog. 2006;5:11.
Iddamaldeniya SS, Wickramasinghe N, Thabrew I, Ratnatunge N, Thammitiyagodage MG. Protection against diethylnitrosoamine-induced hepatocarcinogenesis by an indigenous medicine comprised of Nigella sativa, Hemidesmus indicus and Smilax glabra: a preliminary study. J Carcinog. 2003;2:6.
Al-Ali A, Alkhawajah AA, Randhawa MA, Shaikh NA. Oral and intraperitoneal LD50 of thymoquinone, an active principle of Nigella sativa, in mice and rats. J Ayub Med Coll Abbottabad. 2008;20:25–7.
Mansour MA, Ginawi OT, El-Hadiyah T, El-Khatib AS, Al-Shabanah OA, Al-Sawaf HA. Effects of volatile oil constituents of Nigella sativa on carbon tetrachloride-induced hepatotoxicity in mice: evidence for antioxidant effects of thymoquinone. Res Commun Mol Pathol Pharmacol. 2001;110:239–51.
Mansour MA, Al-Ismaeel H, Al-Rikabi AC, Al-Shabanah OA. Comparison of angiotensin converting enzyme inhibitors and angiotensin II type 1 receptor blockade for the prevention of premalignant changes in the liver. Life Sci. 2011;89:188–94.
Nakagawa T, Takeishi S, Kameyama A, Yagi H, Yoshioka T, Moriwaki K, et al. Glycomic analyses of glycoproteins in bile and serum during rat hepatocarcinogenesis. J Proteome Res. 2010;9:4888–96.
Taha MM, Abdul AB, Abdullah R, Ibrahim TA, Abdelwahab SI, Mohan S. Potential chemoprevention of diethylnitrosamine-initiated and 2-acetylaminofluorene-promoted hepatocarcinogenesis by zerumbone from the rhizomes of the subtropical ginger (Zingiber zerumbet). Chem Biol Interact. 2010;186:295–305.
Singh BN, Singh BR, Sarma BK, Singh HB. Potential chemoprevention of N-nitrosodiethylamine-induced hepatocarcinogenesis by polyphenolics from Acacia nilotica bark. Chem Biol Interact. 2009;181:20–8.
Lee J, Lim KT. Preventive effect of phytoglycoprotein (38 kDa) on expression of alpha-fetoprotein and matrix metalloproteinase-9 in diethylnitrosamine-treated ICR mice. Drug Chem Toxicol. 2011;35(3):277–84.
Machida K, Tsukamoto H, Liu JC, Han YP, Govindarajan S, Lai MM, et al. c-Jun mediates hepatitis C virus hepatocarcinogenesis through signal transducer and activator of transcription 3 and nitric oxide-dependent impairment of oxidative DNA repair. Hepatology. 2010;52:480–92.
Acknowledgments
The authors are grateful to Dr. Alaa Tawfik, Institute of Natural Medicine, University of Toyama for his kind cooperation in preparing the ethanolic extract. The expert technical assistance of Mrs. Etsuko Furuichi is aknowledged and greatly appreciated by the authors.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fathy, M., Nikaido, T. In vivo modulation of iNOS pathway in hepatocellular carcinoma by Nigella sativa . Environ Health Prev Med 18, 377–385 (2013). https://doi.org/10.1007/s12199-013-0336-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12199-013-0336-8