Abstract
Background
Physician empathy is an essential attribute of the patient–physician relationship and is associated with better outcomes, greater patient safety and fewer malpractice claims.
Objective
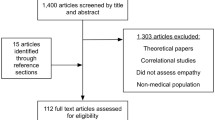
We tested whether an innovative empathy training protocol grounded in neuroscience could improve physician empathy as rated by patients.
Design
Randomized controlled trial.
Intervention
We randomly assigned residents and fellows from surgery, medicine, anesthesiology, psychiatry, ophthalmology, and orthopedics (N = 99, 52% female, mean age 30.6 ± 3.6) to receive standard post-graduate medical education or education augmented with three 60-minute empathy training modules.
Main Measure
Patient ratings of physician empathy were assessed within one-month pre-training and between 1–2 months post-training with the use of the Consultation and Relational Empathy (CARE) measure. Each physician was rated by multiple patients (pre-mean = 4.6 ± 3.1; post-mean 4.9 ± 2.5), who were blinded to physician randomization. The primary outcome was change score on the patient-rated CARE.
Key Results
The empathy training group showed greater changes in patient-rated CARE scores than the control (difference 2.2; P = 0.04). Trained physicians also showed greater changes in knowledge of the neurobiology of empathy (difference 1.8; P < 0.001) and in ability to decode facial expressions of emotion (difference 1.9; P < 0.001).
Conclusions
A brief intervention grounded in the neurobiology of empathy significantly improved physician empathy as rated by patients, suggesting that the quality of care in medicine could be improved by integrating the neuroscience of empathy into medical education.

Similar content being viewed by others
References
Nunes P, Williams S, Stevenson K. A study of empathy decline in students from five health disciplines during their first year of training. Int J Med Educ. 2011;2:12–7.
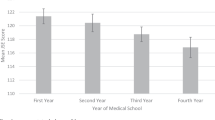
Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: A longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–91.
Bellini LM, Shea JA. Mood changes and empathy decline persist during internal medicine residency training. Acad Med. 2005;80:164–7.
Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: A systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009.
Colliver JA, Conlee MJ, Verhulst SJ, Dorsery JK. Reports of the decline of empathy during medical education are greatly exaggerated: A reexamination of the research. Acad Med. 2010;85(4):588–93.
Medical School Objectives Project. Learning Objectives for Medical Education: Guidelines for Medical Schools. Association of American Medical Colleges, 1998.
Chaudhry HJ, Rhyne J, Cain FE, Young A, Crane M, Bush F. Maintenance of licensure: protecting the public, promoting quality health care. J Med Regul. 2010;96(1):1–8.
Hickson GB, Federspiel CF, Pichert JW, Miller CS, Gauld-Jaeger J, Bost P. Patient complaints and malpractice risk. J Am Med Assoc. 2002;287(22):2951–7.
Halpern J. from detached concern to empathy: Humanizing medical practice. Paperbackth ed. New York: Oxford University Press; 2010.
Brennan TA, Leape LL, Laird NM. Incidence of adverse events and negligence in hospitalized patients: Results of the Harvard medical practice study I. N Engl J Med. 1991;324:370–6.
Marci CD, Riess H. The clinical relevance of psychophysiology: Support for the psychobiology of empathy and psychodynamic process. Am J Psychother. 2005;59(3):213–26.
Kelley JM, Lembo AJ, Ablon JS, et al. Patient and practitioner influences on the placebo effect in irritable bowel syndrome. Psychosom Med. 2009;71(7):789–97.
Kaptchuk TJ, Kelley JM, Conboy LA, et al. Components of placebo effect: Randomised controlled trial in patients with Irritable Bowel Syndrome. Br Med J. 2008;336:998–1003.
Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz CG. J S. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359–64.
Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. J Am Med Assoc. 2009;302(12):1284–93.
Decety J, Yang C, Chen Y. Physicians down-regulate their pain empathy response: An event-related brain potential study. Neuroimage. 2010;50:1676–82.
Harris J. The evolutionary neurobiology, emergence and facilitation of empathy. In: Farrow TFD, Woodruff PWR, eds. Empathy in mental illness. Cambridge: Cambridge University Press; 2007:506.
Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the "nature" and "specific effectiveness" of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns. 2009;74(3):339–46.
Decety J, Jackson PL. The functional architecture of human empathy. Behav Cogn Neurosci Rev. 2004;3:71–100.
Decety J. Dissecting the neural mechanisms mediating empathy. Emotion Review. 2011;3(1):92–108.
Riess H. Biomarkers in the psychotherapeutic relationship: the role of physiology, neurobiology, and biological correlates of E.M.P.A.T.H.Y. Harv Rev Psychiatry. 2011;19(3):162–74.
Smith RC, Lyles JS, Mettler JA, et al. A strategy for improving patient satisfaction by the intensive training of residents in psychosocial medicine: a controlled, randomized study. Acad Med. 1995;70(8):729–32.
Alder J, Christen R, Zemp E, Bitzer J. Communication skills training in obstetrics and gynaecology: whom should we train? A randomized controlled trial. Arch Gynecol Obstet. 2007;276:605–612.
Stein T, Frankel RM, Krupat E. Enhancing clinician communication skills in a large healthcare organization: a longitudinal case study. Patient Educ Couns. 2005;58(1):4–12.
Riess H. Empathy in medicine—A neurobiological perspective. J Am Med Assoc. 2010;304(14):1604–5.
Riess H, Kelley JM, Bailey RW, Konowitz PM, Gray ST. Improving empathy and relational skills in otolaryngology residents: a pilot study. Otolaryngol Head Neck Surg. 2011;144(1):120–2.
Carr L, Iacoboni M, Dubeau M, Mazziotta JC, Lenzi GL. Neural mechanisms of empathy in humans: a relay from neural systems for imitation to limbic areas. Proc Natl Acad Sci. 2003;100(9):5497–502.
Saarela MV, Hlushchuk Y, Williams AC, Schürmann M, Kalso E, Hari R. The compassionate brain: humans detect intensity of pain from another's face. Cereb Cortex. 2007;17(1):230–7.
Hammond DC. Hypnotic induction and suggestion: An introductory manual. 1st ed. Des Plaines, IL: The American Society of Clinical Hypnosis; 1988.
Epstein R. Mindful practice. J Am Med Assoc. 1999;282:833–9.
Mercer SW, Maxwell M, Heaney D, Watt GCM. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Fam Pract. 2004;21(6):699–705.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Ekman P. Emotions revealed: Recognizing faces and feelings to improve communication and emotional life. New York: Holt; 2004.
Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: Development and preliminary psychometric data. Educ Psychol Meas. 2001;61:349–65.
Mehrabian A, Epstein N. A measure of emotional empathy. J Pers. 1972;40:525–43.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988.
Hemmerdinger JM, Samuel DR Stoddart SDR, Lilford RJ. A systematic review of tests of empathy in medicine. BMC Med Educ. 2007;7(24).
Bieber C, Muller KG, Blumenstiel K, et al. A shared decision-making communication training program for physicians treating fibromyalgia patients: effects of a randomized controlled trial. J Psychosom Res. 2008;64:13–20.
Brown LD, De Negri B, Hernandez O, Domingueq L, Sanchack JH, Roter DL. An evaluation of the impact of training Honduran health care providers in interpersonal communication. Int J Qual Health Care. 2000;12(6):595–01.
Roter DL, Rosenbaum J, de Negri B, Renaud D, DiPrete-Brown L, Hernandez O. The effects of a continuing medical education programme in interpersonal communication skills on doctor practice and patient satisfaction in Trinidad and Tobago. Med Educ. 1998;32:181–9.
Sulmasy DP. Should medical schools be schools for virtue? J Gen Intern Med. 2000;15(7):514–6.
Acknowledgments
Contributors: We thank Dr. Lidia Schapira for her helpful comments on the manuscript and Dr. Brian C. George for his assistance with study design and recruitment. We are grateful to Paul Ekman, PhD for permission to use the Ekman Test. We are also grateful to the residents and fellows who participated in this study, to the patients who provided ratings of physician empathy, and to the staff, program directors, and department chiefs of the participating specialties.
Funders:
We are grateful to the following foundations for their generous support: The Arnold P. Gold Foundation, The David Judah Fund, The Josiah Macy, Jr. Foundation, and The Risk Management Foundation. The funding agencies played no role in the design and conduct of this study, including analysis and interpretation of data, and preparation, review, and approval of the manuscript.
Prior Presentations
This work has not been presented previously.
Conflict of Interest:
Helen Riess reports her role as Chief Technology Officer for Empathetics, LLC. This study was completed prior to formation of Empathetics, LLC. The other authors declare that they do not have a conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Riess, H., Kelley, J.M., Bailey, R.W. et al. Empathy Training for Resident Physicians: A Randomized Controlled Trial of a Neuroscience-Informed Curriculum. J GEN INTERN MED 27, 1280–1286 (2012). https://doi.org/10.1007/s11606-012-2063-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-012-2063-z