Abstract
Background
Despite proven safety and efficacy, rates of minimally invasive approaches for colon cancer remain low in the USA. Given the known benefits, investigating the root causes of underutilization and methods to increase laparoscopy is warranted. Our goal was to develop a predictive model of factors impacting use of laparoscopic surgery for colon cancer.
Methods
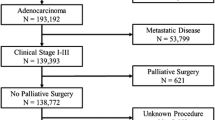
The Premier Hospital Database was reviewed for elective colorectal resections for colon cancer (2009–2014). Patients were identified by ICD-9-CM diagnosis code and then stratified into open or laparoscopic approaches by ICD-9-CM procedure codes. An adjusted multivariate logistic regression model identified variables predictive of use of laparoscopy for colon cancer.
Results
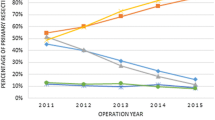
A total of 24,245 patients were included–12,523 (52 %) laparoscopic and 11,722 (48 %) open. General surgeons performed the majority of all procedures (77.99 % open, 71.60 % laparoscopic). Overall use of laparoscopy increased from 48.94 to 52.03 % over the study period (p < 0.0001). Patients with private insurance were more likely to have laparoscopy compared with Medicare patients (adjusted odds ratio (OR) 1.089, 95 % CI [1.004, 1.181], p = 0.0388). Higher volume of surgeons (OR 3.518, 95 % CI [2.796, 4.428], p < 0.0001) and larger hospitals by bed size were more likely to approach colon cancer laparoscopically. Colorectal surgeons were 32 % more likely to approach a case laparoscopically than general surgeons (OR 1.315, 95 % CI [1.222, 1.415], p < 0.0001). Teaching hospitals, hospitals in the Midwest, and hospitals with less than 500 beds were less likely to use laparoscopy.
Conclusions
There are patient, provider, and hospital characteristics that can be identified preoperatively to predict who will undergo surgery for colon cancer using laparoscopy. However, additional patients may be eligible for laparoscopy based on patient-level characteristics. These results have implications for regionalization and increasing teaching of MIS. Recognizing and addressing these variables with training and recruiting could increase use of minimally invasive approaches, with the associated clinical and financial benefits.
Similar content being viewed by others
References
Jacobs M, Verdeja JC, Goldstein HS (1991) Minimally invasive colon resection (laparoscopic colectomy). Surg Laparosc Endosc 1:144–150
Delaney CP, Kiran RP, Senagore AJ, Brady K, Fazio VW (2003) Case-matched comparison of clinical and financial outcome after laparoscopic or open colorectal surgery. Ann Surg 238:67–72
Delaney CP, Chang E, Senagore AJ, Broder M (2008) Clinical outcomes and resource utilization associated with laparoscopic and open colectomy using a large national database. Ann Surg 247:819–824
Senagore AJ, Stulberg JJ, Byrnes J, Delaney CP (2009) A national comparison of laparoscopic vs. open colectomy using the National Surgical Quality Improvement Project data. Dis Colon Rectum 52:183–186
Braga M, Frasson M, Zuliani W, Vignali A, Pecorelli N, Di Carlo V (2010) Randomized clinical trial of laparoscopic versus open left colonic resection. Br J Surg 97:1180–1186
Senagore AJ (2015) Adoption of Laparoscopic Colorectal Surgery: it Was Quite a Journey. Clin Colon Rectal Surg 28:131–134
Akle CA (1996) Early parietal recurrence of adenocarcinoma of the colon after laparoscopic colectomy. Port site metastasis after laparascopic colorectal surgery for cure of malignancy. Br J Surg 83:427
Berends FJ, Kazemier G, Bonjer HJ, Lange JF (1994) Subcutaneous metastases after laparoscopic colectomy. Lancet 344(8914):58
Jacquet P, Averbach AM, Jacquet N (1995) Abdominal wall metastasis and peritoneal carcinomatosis after laparoscopic-assisted colectomy for colon cancer. Eur J Surg Oncol 21:568–570
Bonjer HJ, Hop WC, Nelson H et al (2007) Laparoscopically assisted vs open colectomy for colon cancer: a meta-analysis. Arch Surg 142:298–303
Kuhry E, Schwenk W, Gaupset R, Romild U, Bonjer J (2008) Long-term outcome of laparoscopic surgery for colorectal cancer: a cochrane systematic review of randomised controlled trials. Cancer Treat Rev 34:498–504
Veldkamp R, Kuhry E, Hop WC et al (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol 6:477–484
Weeks JC, Nelson H, Gelber S, Sargent D, Schroeder G (2002) Short-term quality-of-life outcomes following laparoscopic-assisted colectomy vs open colectomy for colon cancer: a randomized trial. Jama 287:321–328
Jayne DG, Guillou PJ, Thorpe H et al (2007) Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol 25:3061–3068
Jayne DG, Thorpe HC, Copeland J, Quirke P, Brown JM, Guillou PJ (2010) Five-year follow-up of the Medical Research Council CLASICC trial of laparoscopically assisted versus open surgery for colorectal cancer. Br J Surg 97:1638–1645
Tjandra JJ, Chan MK (2006) Systematic review on the short-term outcome of laparoscopic resection for colon and rectosigmoid cancer. Colorectal Dis 8:375–388
Lacy AM, Garcia-Valdecasas JC, Delgado S et al (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Lacy AM, Delgado S, Castells A et al (2008) The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg 248:1–7
Nelson H, Sargent DJ (2004) COST Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 350:2050–2059
Braga M, Vignali A, Gianotti L et al (2002) Laparoscopic versus open colorectal surgery: a randomized trial on short-term outcome. Ann Surg 236:759–766 (discussion 767)
Fleshman J, Sargent DJ, Green E et al (2007) Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg 246:655–662 (discussion 662-624)
Poylin V, Curran T, Lee E, Nagle D (2014) Laparoscopic colectomy decreases the time to administration of chemotherapy compared with open colectomy. Ann Surg Oncol 21:3587–3591
Rea JD, Cone MM, Diggs BS, Deveney KE, Lu KC, Herzig DO (2011) Utilization of laparoscopic colectomy in the United States before and after the clinical outcomes of surgical therapy study group trial. Ann Surg 254:281–288
Carmichael JC, Masoomi H, Mills S, Stamos MJ, Nguyen NT (2011) Utilization of laparoscopy in colorectal surgery for cancer at academic medical centers: does site of surgery affect rate of laparoscopy? Am Surg 77:1300–1304
Robinson CN, Chen GJ, Balentine CJ et al (2011) Minimally invasive surgery is underutilized for colon cancer. Ann Surg Oncol 18:1412–1418
Fox J, Gross CP, Longo W, Reddy V (2012) Laparoscopic colectomy for the treatment of cancer has been widely adopted in the United States. Dis Colon Rectum 55:501–508
Premier Research Services. https://www.premierinc.com/transforming-healthcare/healthcare-performance-improvement/premier-research-services/ Last accessed February 2015
All Patient Refined Diagnostic Related Groups Methodology Overview. v20.0. 3 M Health Information Systems. http://www.hcup-us.ahrq.gov/db/nation/nis/APR-DRGsV20MethodologyOverviewandBibliography.pdf Last accessed June 2015
Moghadamyeghaneh Z, Carmichael JC, Mills S, Pigazzi A, Nguyen NT, Stamos MJ (2015) Variations in Laparoscopic Colectomy Utilization in the United States. Dis Colon Rectum 58:950–956
Keller DS, Delaney CP, Hashemi L, Haas EM (2015) A national evaluation of clinical and economic outcomes in open versus laparoscopic colorectal surgery. Surg Endosc. doi:10.1007/s00464-015-4732-6
Crawshaw BP, Chien HL, Augestad KM, Delaney CP (2015) Effect of laparoscopic surgery on health care utilization and costs in patients who undergo colectomy. JAMA Surg 150:410–415
Wennberg JE, Fisher ES, Skinner JS (2002) Geography and the debate over Medicare reform. Health Aff (Millwood), Suppl Web Exclusives:W96–114
Reames BN, Sheetz KH, Waits SA, Dimick JB, Regenbogen SE (2014) Geographic variation in use of laparoscopic colectomy for colon cancer. J Clin Oncol 32:3667–3672
Moloo H, Haggar F, Martel G et al (2009) The adoption of laparoscopic colorectal surgery: a national survey of general surgeons. Can J Surg 52:455–462
Accreditation Council of Graduate Medical Education (ACGME) Colon and Rectal Surgery Fellowship Programs. https://www.acgme.org/acgmeweb/tabid/129/ProgramandInstitutionalAccreditation/SurgicalSpecialties/ColonandRectalSurgery.aspx Last accessed March 2016
Non-ACGME Advanced Colorectal Fellowship Programs. The Fellowship Council. Available online at: https://fellowshipcouncil.org/directory-of-fellowships/?match=2 Last accessed March 2016
Coleman MG, Hanna GB, Kennedy R (2011) The National Training Programme for Laparoscopic Colorectal Surgery in England: a new training paradigm. Colorectal Dis 13:614–616
Mackenzie H, Miskovic D, Ni M et al (2015) Risk prediction score in laparoscopic colorectal surgery training: experience from the English National Training Program. Ann Surg 261:338–344
Mackenzie H, Miskovic D, Ni M et al (2013) Clinical and educational proficiency gain of supervised laparoscopic colorectal surgical trainees. Surg Endosc 27:2704–2711
Kapiteijn E, Putter H, van de Velde CJ (2002) Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg 89:1142–1149
Chowdhury MM, Dagash H, Pierro A (2007) A systematic review of the impact of volume of surgery and specialization on patient outcome. Br J Surg 94:145–161
Aquina CT, Probst CP, Becerra AZ et al (2016) High volume improves outcomes: the argument for centralization of rectal cancer surgery. Surgery 159:736–748
Munasinghe A, Markar SR, Mamidanna R et al (2015) Is It Time to Centralize High-risk Cancer Care in the United States? Comparison of Outcomes of Esophagectomy Between England and the United States. Ann Surg 262:79–85
Pawa N, Cathcart PL, Arulampalam TH, Tutton MG, Motson RW (2012) Enhanced recovery program following colorectal resection in the elderly patient. World J Surg 36:415–423
Roscio F, Bertoglio C, De Luca A, Frigerio A, Galli F, Scandroglio I (2011) Outcomes of laparoscopic surgery for colorectal cancer in elderly patients. JSLS 15:315–321
She WH, Poon JT, Fan JK, Lo OS, Law WL (2013) Outcome of laparoscopic colectomy for cancer in elderly patients. Surg Endosc 27:308–312
Iorio T, Blumberg D (2014) Laparoscopic colectomy is feasible in the mega-obese patient using a standardized technique. Surg Obes Relat Dis 10:1005–1008
Makino T, Trencheva K, Shukla PJ et al (2014) The influence of obesity on short- and long-term outcomes after laparoscopic surgery for colon cancer: a case-matched study of 152 patients. Surgery 156:661–668
Vignali A, De Nardi P, Ghirardelli L, Di Palo S, Staudacher C (2013) Short and long-term outcomes of laparoscopic colectomy in obese patients. World J Gastroenterol 19:7405–7411
Keller DS, Ibarra S, Flores-Gonzalez JR et al (2016) Outcomes for single-incision laparoscopic colectomy surgery in obese patients: a case-matched study. Surg Endosc 30:739–744
Keller DS, Madhoun N, Flores-Gonzalez JR, Ibarra S, Tahilramani R, Haas EM (2016) Effect of BMI on short-term outcomes with robotic-assisted laparoscopic surgery: a case-matched study. J Gastrointest Surg 20:488–493
Kang CY, Halabi WJ, Chaudhry OO et al (2013) A nationwide analysis of laparoscopy in high-risk colorectal surgery patients. J Gastrointest Surg 17:382–391
Acknowledgments
The authors acknowledge Medtronic Minimally Invasive Surgical Therapies group for supporting the data source and analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Dr. Keller has no conflict of interest, Mr. Parikh is an employee of Medtronic, Inc., in the Medtronic Minimally Invasive Surgical Therapies group at the time of the analysis, and Dr. Senagore was in the Advisory board consulting fees from Ethicon Endosurgery.
Rights and permissions
About this article
Cite this article
Keller, D.S., Parikh, N. & Senagore, A.J. Predicting opportunities to increase utilization of laparoscopy for colon cancer. Surg Endosc 31, 1855–1862 (2017). https://doi.org/10.1007/s00464-016-5185-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5185-2