Abstract
Background
The aim of this study was to assess the time from the first subfertility diagnosis to pregnancy (TTP) and to elucidate factors influencing TTP for patients in German gynecological practices comprising a representative sample and provide a realistic picture of the current situation in Germany.
Methods
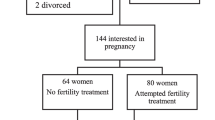
The study collective included all women with first-time diagnoses of female infertility (ICD: N97) or unfulfilled desire for children (ICD: Z31) from the representative database (IMS Disease Analyzer). Demographic data on patients such as their age (ranges 18–25, 26–30, 31–35, 36–40 or 51–50) and information on previous pregnancies and births and concomitant diseases were collected. Data pertaining to 61,815 women from 433 gynecological practices in Germany with a first diagnosis of female infertility or an unfulfilled desire for children were analyzed. The period of data collection was between January 1, 2001 to December 31, 2012 (=144 months). The mean observation period for the patients after the first gynecological consultation was 1,420 days (=47.3 months), with a standard deviation of 879 days.
Results
A total of 22,744 patients became pregnant during the first year of observation (36.8 %). The highest cumulative pregnancy rate was seen in women between 18 and 30 years of age (74.8 %). The older the women were, the lower the cumulative pregnancy rate became (18.1 % in the group of 41- to 50-year-old women). Cox regression calculations showed that the following factors considerably impaired the chances of pregnancy: age, endometriosis, diabetes mellitus, ovarian dysfunction, PCOS, previous infection of the genitourinary tract. In contrast, a couple of factors were proven to increase pregnancy rates, namely previous use of hormonal contraceptives, private insurance, previous birth, previous pregnancy and progesterone therapy (at any time).
Conclusion
Along with information about reproductive physiology, such as decreasing fertility with maternal age, counseling in daily practice should also include individual factors influencing fertility. It is of the utmost importance to further increase public awareness of the impact of advanced female and male age on the reproductive outcome so that people can make well-informed decisions on when to start a family.

Similar content being viewed by others
References
Practice Committee of American Society for Reproductive Medicine (2013) Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil Steril 99(1):63. doi:10.1016/j.fertnstert.2012.09.023
WHO. (2002). Current practices and controversies in assisted reproduction. Report of a conference on “Medical, Ethical and Social Aspects of Assisted Reproduction”. Retrieved from http://whqlibdoc.who.int/hq/2002/9241590300.pdf
Ziller M, Rashed AN, Ziller V, Kostev K (2013) The prescribing of contraceptives for adolescents in German gynecologic practices in 2007 and 2011: a retrospective database analysis. J Pediatr Adolesc Gynecol 26(5):261–264. doi:10.1016/j.jpag.2013.04.003
Becher H, Kostev K, Schröder-Bernhardi D (2009) Validity and representativeness of the “disease analyzer” patient database for use in pharmacoepidemiological and pharmacoeconomic studies. Int J Clin Pharmacol Ther 47(10):617–626
Ziller M, Ziller V, Haas G, Rex J, Kostev K (2013) Risk of venous thrombosis in users of hormonal contraceptives in German gynaecological practices: a patient database analysis. Arch Gynecol Obstet. doi:10.1007/s00404-013-2983-9
Ziller V, Hadji P, Thielscher C, Ziller M, Kostev K (2013) Prevalence of female subfertility in German gynecological practices. Gynecological endocrinology: the official journal of the international society of gynecological endocrinology 29(8):767–770. doi:10.3109/09513590.2013.798274
Van der Ven H, Kühr M, Roth S, van der Ven K (2013) [Nimmt die gynäkologische Fertilität ab?] Does gynecological fertility decrease? Der Gynäkologe 46(1):12–17
Strowitzki T (2013) Infertility in women : latest developments. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 56(12):1628–1632. doi:10.1007/s00103-013-1851-x
Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, Nygren K, Sullivan EA, World Health Organization (2009) International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril 92(5):1520–1524. doi:10.1016/j.fertnstert.2009.09.009
Macer ML, Taylor HS (2012) Endometriosis and infertility: a review of the pathogenesis and treatment of endometriosis-associated infertility. Obstet Gynecol Clin North Am 39(4):535–549. doi:10.1016/j.ogc.2012.10.002
Dunson DB, Colombo B, Baird DD (2002) Changes with age in the level and duration of fertility in the menstrual cycle. Hum Reprod (Oxford, England) 17(5):1399–1403
Mutsaerts MAQ, Groen H, Huiting HG, Kuchenbecker WKH, Sauer PJJ, Land JA, Stolk RP, Hoek A (2012) The influence of maternal and paternal factors on time to pregnancy—a Dutch population-based birth-cohort study: the GECKO Drenthe study. Hum Reprod (Oxford, England) 27(2):583–593. doi:10.1093/humrep/der429
Schmidt L, Sobotka T, Bentzen JG, Nyboe Andersen A, ESHRE Reproduction and Society Task Force (2012) Demographic and medical consequences of the postponement of parenthood. Hum Reprod Update 18(1):29–43. doi:10.1093/humupd/dmr040
Homan GF, Davies M, Norman R (2007) The impact of lifestyle factors on reproductive performance in the general population and those undergoing infertility treatment: a review. Hum Reprod Update 13(3):209–223. doi:10.1093/humupd/dml056
Gupta S, Goldberg JM, Aziz N, Goldberg E, Krajcir N, Agarwal A (2008) Pathogenic mechanisms in endometriosis-associated infertility. Fertil Steril 90(2):247–257. doi:10.1016/j.fertnstert.2008.02.093
Usadi RS, Legro RS (2012) Reproductive impact of polycystic ovary syndrome. Curr Opin Endocrinol Diabetes Obes 19(6):505–511. doi:10.1097/MED.0b013e328359ff92
Panidis D, Tziomalos K, Papadakis E, Katsikis I (2013) Infertility treatment in polycystic ovary syndrome: lifestyle interventions, medications and surgery. Front Horm Res 40:128–141. doi:10.1159/000341824
Thessaloniki ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group (2008) Consensus on infertility treatment related to polycystic ovary syndrome. Fertil Steril 89(3):505–522. doi:10.1016/j.fertnstert.2007.09.041
Akande V, Turner C, Horner P, Horne A, Pacey A, British Fertility Society (2010) Impact of Chlamydia trachomatis in the reproductive setting: British Fertility Society Guidelines for practice. Human Fertility (Cambridge, England), 13(3):115–125. doi:10.3109/14647273.2010.513893
Haggerty CL, Gottlieb SL, Taylor BD, Low N, Xu F, Ness RB (2010) Risk of sequelae after Chlamydia trachomatis genital infection in women. J Infect Dis 201(Suppl 2):S134–S155. doi:10.1086/652395
Taylor BD, Darville T, Tan C, Bavoil PM, Ness RB, Haggerty CL (2011) The role of Chlamydia trachomatis polymorphic membrane proteins in inflammation and sequelae among women with pelvic inflammatory disease. Infect Dis Obstet Gynecol 2011:989762. doi:10.1155/2011/989762
Coughlan C, Ledger W (2008) In-vitro fertilisation. Obstet Gynaecol Reprod Med 18(11):300–306
Conflict of interest
The authors have none to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
C. Heilmaier and K. Kostev contributed equally.
Rights and permissions
About this article
Cite this article
Ziller, V., Heilmaier, C. & Kostev, K. Time to pregnancy in subfertile women in German gynecological practices: analysis of a representative cohort of more than 60,000 patients. Arch Gynecol Obstet 291, 657–662 (2015). https://doi.org/10.1007/s00404-014-3449-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-014-3449-4