Abstract
Purpose
Anterior cruciate ligament (ACL) reconstruction has been under intensive discussion and debate, although the anatomy of this ligament was resolved thoroughly almost 200 years ago. The ACL consist of two bundles, anteromedial (AM) and posterolateral (PL). The conventional single-bundle method reconstructs the AM bundle only, while the modern double-bundle technique recreates both bundles for their anatomical sites.
Methods
An English language literature search was undertaken over the years 2000–2012 for ACL reconstruction, double-bundle versus single bundle technique. The search found 14 RCTs and two meta-analyses published to date.
Results
Two of the 14 studies (14 %) showed no difference between the two reconstruction methods while the remaining majority (12 trials, 86 %) concluded that the DB technique was better than the SB method. After the DB reconstruction, rotational stability of the knee was better in seven studies (50 %) and anteroposterior stability in six (43 %). No study spoke for the single-bundle technique. In addition, with the double-bundle technique knee scores were reported to be better in five (36 %) studies, and three trials (21 %) revealed less reoperations in the double-bundle group.
Conclusions
The double-bundle ACL reconstruction technique was reported to have better or at least the same results as the conventional single-bundle method—even at a five-year follow-up. However, the majority of these studies had a rather short follow-up, and thus, longer studies are needed to confirm the true long-term results of ACL surgery. Long follow-up periods are also needed to find out whether double-bundle ACL reconstruction can eventually prevent knee osteoarthritis.
Similar content being viewed by others
Introduction
The double-bundle structure of the human anterior cruciate ligament was described almost 200 years ago by the Weber brothers [1]. Since then there has been a variety of different reconstruction techniques using different grafts and fixation methods [1]. Open surgery was the practice until the late 1990s, when arthroscopic techniques developed quickly and the goal in ACL surgery shifted to anatomical mini-invasive techniques [1].
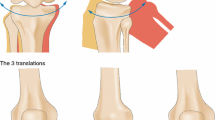
Regardless of the surgical intervention method used, the key element in ACL surgery remains knee and ACL anatomy, which have been resolved thoroughly for the tibial and femoral sides [2–17]. The ACL has two bundles, anteromedial and posterolateral, the names given from the tibial insertion site. The ACL bundles originating from the anteromedial portion of the tibial attachment are inserted into the high and deep portion of the femoral attachment in flexion, whereas those from the anterolateral portion are inserted into high and shallow portions of the femoral site [18]. Bundles originating from the posteromedial portion of the tibia are inserted into low and deep portions of the femoral footprint, and those from the posterolateral portion of the tibia into low and shallow portions of the femoral footprint. The anatomical placements of the individual bundles remain the same, obviously, regardless of the flexion angle of the knee, but the functional anatomy changes in different knee flexion angles. The AM bundle is reported to become loose when the knee is near extension and to tighten in flexion, while the PL bundle acts vice versa and also during internal and external rotation of the tibia [19–27].
The main indication for reconstruction of the torn ACL is a repeated giving way symptom despite proper knee rehabilitation [28, 29]. In addition, some studies conclude that high-demand patients such as athletes should be treated operatively more actively than non-athletes [30, 31]. However, none of the current ACL treatment methods, whether operative or conservative, has been able to prevent subsequent degenerative changes in the knee joint [32].
In the single-bundle ACL reconstruction, which previously was the gold standard, only the AM bundle is recreated. It does not prevent the post-surgery laxity, especially in the rotational plane, and therefore, a more anatomical method or double-bundle technique was developed [33]. In the double-bundle technique both bundles of the ACL are reconstructed.
This article focuses on the clinical results of the double-bundle method by reviewing studies that have compared the double-bundle and single-bundle techniques using a randomised trial design.
Materials and methods
An English language literature search was performed in the PubMed database with keywords “double-bundle versus single-bundle technique and ACL reconstruction”. The search was limited to studies published between January 1, 2000 and May 31, 2012. Articles included in this review were all prospective and randomised, controlled trials (level I) or meta-analyses. The future aspects of ACL surgery are also discussed at the end of this article.
Randomised controlled studies
The search revealed 14 prospective and randomised controlled studies comparing single-bundle versus double-bundle ACL reconstruction. The first study was by Adachi et al. in 2004 [34]. They had 55 patients in the single-bundle group (SB) and 53 in the double-bundle group (DB) with follow-up time of 24 to 36 months. Their operative technique in the DB group consisted of one tunnel in the tibial side and two tunnels in the femoral side, and the femoral tunnels were made by the transtibial technique, so the DB technique was not anatomical. There were significantly more notchplasties made in the SB group than the DB group, but there were not any other statistically significant differences between the groups.
Muneta et al. published their results in 2007 [35]. They had 34 patients in both groups and their follow-up time was 18–40 months (mean 25 months). They also created femoral tunnels in the transtibial manner. Their conclusion was that the DB group had statistically more stable knees in the antero-posterior and rotational planes. Another study concluding that the DB group had better rotational laxity is by Järvelä [36] with 12–20 months (mean 14 months) of follow-up. In this study, the femoral side tunnels were made using the free-hand technique through an anteromedial portal. Järvelä et al. [37] reported longer follow-up (24–35 months) results in 2008. The study design included an SB group with metallic screws (N = 25), an SB group with bioabsorbable screws (N = 27) and a DB group with bioabsorbable screws (N = 25). Their conclusion was that the DB group had the best rotational stability of the knee. Another finding was that the DB group had less graft failures compared to any of the SB groups.
Siebold et al. [38] reported results of 70 patients with 13–24 months (mean 19 months) follow-up. Their main finding was that the DB group had better rotational stability and objective knee score. Anterior laxity was also reported to be better in the DB group, but the difference was not statistically significant.
Zaffagnini et al. [39] published their study of 72 patients with follow-up of three years in 2008. Their operative technique was somewhat different from any of those previously reported, since their SB group had an additional extra-articular sling and the DB group had only one tunnel in the femoral and also in the tibial side with the anteromedial bundle made with an “over the top” passage of the graft. Nevertheless, they concluded that the DB group had significantly better results in terms of subjective, objective, and functional evaluations of the knee. Anterior stability was also significantly better in the DB group.
More recently Zaffagnini et al. [40] reported a longer follow-up study of eight years. In this study, the operation method in the DB group was the same as described above, but the SB group was reconstructed with lateralised bone-patellar tendon-bone technique. Their conclusions were that the DB group had higher Tegner activity level, better recovery in the passive range of motion of the knee, and faster sport resumption. The knees in the DB group were also more stable in the rotational plane and had less re-interventions than those in the SB group. In addition, radiographic evaluation showed lower objective degenerative changes in the DB group at the eight-year follow-up.
Ibrahim et al. [41] had altogether 200 patients in their study, in which there were 50 patients in the DB group, 48 patients in the SB group with Endobutton fixation, 52 patients in the SB group with RigidFix fixation and 50 patients in the SB group with bioabsorbable Transfix II fixation. Follow-up time was 25–38 months (mean 29 months). Their conclusion was that the best stability in antero-posterior and rotational planes was in the DB group.
Streich et al. [42] conducted a study of 50 male patients with follow-up of 23–25 months (mean 24). Their main finding was that contrary to their hypothesis there was no significant difference between the SB and the DB group regarding stability or knee evaluation forms. Sastre et al. [43] had similar results in their study at the two-year follow-up. Aglietti et al. [44] reported two-year results in 2010. Their RCT consisted of 35 patients in SB and DB groups. The DB reported to have better anterior stability, better VAS and final objective IKDC score.
Suomalainen et al. [45] published their two-year RCT results of 153 patients in 2011. The SB group had 78 and the DB group 75 patients. Their main finding in this study was that the DB group had significantly lower rate of graft ruptures and subsequent ACL re-reconstructions compared to the SB group. Another finding was that there was no statistically significant difference in the stability measurements between these two groups.
Hussein et al. [46] conducted a study in which there were 72 patients in the conventional single-bundle group, 78 patients in the anatomical single-bundle group and 131 patients in the anatomical double-bundle group. The conventional single-bundle procedure’s femoral tunnel was made transtibially, but the anatomical reconstructions via the anteromedial portal. The follow-up time in all groups was 39–63 months (mean 51 months). The main finding of this study was that the DB group had the best stability in anteroposterior and rotational planes. In addition, the DB procedure resulted in better scores than the conventional single-bundle procedure in the Lysholm and IKDC evaluations. The range of motion was better in the DB group than in the conventional SB group as well. The anatomical SB group was ranked second in stability measurements but in the other evaluations there was no statistically significant difference.
The longest follow-up (five years) study published to date on single bundle versus anatomical double-bundle anterior cruciate ligament reconstruction is by Suomalainen et al. [47]. There were three groups in this study with 30 patients in each: single-bundle with bioabsorbable screws, single-bundle with metallic screws and double-bundle with bioabsorbable screws. The main findings in this study was that the stability measurements were similar between all the three groups, but the double-bundle group had significantly fewer ACL revisions for graft rupture compared to both single-bundle groups.
Details of the studies discussed are presented in Table 1. The main conclusion drawn from these level one trials is that although the double bundle ACL reconstruction method is a demanding surgical procedure none of the studies has reported that the DB method is inferior to the SB reconstruction. On the contrary, the double-bundle method seems to give better overall results than the single-bundle method (12 studies out of the 14 published to date), and only two studies conclude that these two ACL reconstruction techniques are equal regarding anteroposterior and rotational knee laxity and knee scores.
Meta-analysis
Meredick et al. [48] published a meta-analysis on ACL surgery in 2008 focusing on single-bundle versus double-bundle ACL reconstruction methods. They concluded that there is no evidence that the double-bundle method is better than its single-bundle counterpart. However, since then several high-quality prospective, randomised studies have been published with different conclusions (see above).
The most recent meta-analysis was made by Zhu et al. [49]. They concluded, in contrast to Meredick, that the double-bundle ACL reconstruction method was superior to the single-bundle technique. They observed that the double-bundle technique resulted in more stable knees in the anteroposterior and rotational planes and created less complications. In addition, the overall IKDC knee score was significantly better in the double-bundle group.
Future aspects of the double-bundle ACL surgery
The ACL reconstruction surgery has walked a long road to where it is today, from open surgery in the middle of the night to a delicate elective arthroscopic manoeuvre with two bundles reconstructed. It has been a hot topic in every arthroscopic symposium held in the 21st century.
Anterior cruciate ligament reconstruction can improve patients’ daily life remarkably, but the results are good only if the grafts are in anatomical places. The double-bundle ACL reconstruction can be more difficult than the single-bundle method since it has two drill holes in the tibial as well femoral side. Navigation was thought to be the solution that would help to conduct more anatomical ACL reconstructions also with the double-bundle method. Endele et al. [50] conducted a study, in which they compared computer navigation with a free-hand technique in a single-bundle ACL reconstruction. There was no statistical difference between these groups at the two-year follow-up and the conclusion was that manual surgery is as good as computer-aided ACL reconstruction, at least in the hands of an experienced orthopaedic surgeon.
Deeper into the “layers” of the ACL surgery goes the so-called ACL remnant preserving technique. Its ultimate purpose is to try to leave the ACL stump intact and to reconstruct the ACL into this remnant. The idea underlying is that the preserved tissue would enhance proprioception, vascularity and biomechanics and thereafter result in clinically better knees. Papalia et al. [51] conducted a review article about this subject. There was no clear evidence to support this remnant preserving conception and they suggested better studies with longer follow-up times. A similar idea is in the selective bundle reconstruction technique, which replaces only the torn part of the ACL and leaves the intact bundle in place. To date, no long-term follow-ups are available.
Summary
This English language literature review shows that the double-bundle ACL reconstruction technique gives better or at least similar results to the conventional single-bundle method even in five-year follow-up. However, longer follow-up studies are needed to see the true long-term results of ACL surgery and to find out whether double-bundle ACL reconstruction can eventually prevent knee osteoarthritis.
References
Schindler OS (2012) Surgery for anterior cruciate ligament deficiency: a historical perspective. Knee Surg Sports Traumatol Arthrosc 20:5–47. doi:10.1007/s00167-011-1756-x
Takahashi M, Doi M, Abe M, Suzuki D, Nagano A (2006) Anatomical study of the femoral and tibial insertions of the anteromedial and posterolateral bundles of human anterior cruciate ligament. Am J Sports Med 34:787–792. doi:10.1177/0363546505282625
Ferretti M, Ekdahl M, Shen W, Fu FH (2007) Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy 23:1218–1225. doi:10.1016/j.arthro.2007.09.008
Edwards A, Bull AM, Amis AA (2007) The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament: Part 1: tibial attachment. Knee Surg Sports Traumatol Arthrosc 15:1414–1421. doi:10.1007/s00167-007-0417-6
Edwards A, Bull AM, Amis AA (2008) The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament. Part 2: femoral attachment. Knee Surg Sports Traumatol Arthrosc 16:29–36. doi:10.1007/s00167-007-0410-0
Ferretti M, Doca D, Ingham SM, Cohen M, Fu FH (2012) Bony and soft tissue landmarks of the ACL tibial insertion site: an anatomical study. Knee Surg Sports Traumatol Arthrosc 20:62–68. doi:10.1007/s00167-011-1592-z
Luites JW, Wymenga AB, Blankevoort L, Kooloos JG (2007) Description of the attachment geometry of the anteromedial and posterolateral bundles of the ACL from arthroscopic perspective for anatomical tunnel placement. Knee Surg Sports Traumatol Arthrosc 15:1422–1431. doi:10.1007/s00167-007-0402-0
Steckel H, Starman JS, Baums MH, Klinger HM, Schultz W, Fu FH (2007) Anatomy of the anterior cruciate ligament double bundle structure: a macroscopic evaluation. Scand J Med Sci Sports 17:387–392. doi:10.1111/j.1600-0838.2006.00579.x
Purnell ML, Larson AI, Clancy W (2008) Anterior cruciate ligament insertions on the tibia and femur and their relationships to critical bony landmarks using high-resolution volume-rendering computed tomography. Am J Sports Med 36:2083–2090. doi:10.1177/0363546508319896
Siebold R, Ellert T, Metz S, Metz J (2008) Tibial insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry, arthroscopic landmarks, and orientation model for bone tunnel placement. Arthroscopy 24:154–161. doi:10.1016/j.arthro.2007.08.006
Siebold R, Ellert T, Metz S, Metz J (2008) Femoral insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry and arthroscopic orientation models for double-bundle bone tunnel placement—a cadaver study. Arthroscopy 24:585–592. doi:10.1016/j.arthro.2007.12.008
Zantop T, Wellmann M, Fu FH, Petersen W (2008) Tunnel positioning of anteromedial and posterolateral bundles in anatomic anterior cruciate ligament reconstruction: anatomic and radiographic findings. Am J Sports Med 36:65–72. doi:10.1177/0363546507308361
Katouda M, Soejima T, Kanazawa T, Tabuchi K, Yamaki K, Nagata K (2011) Relationship between thickness of the anteromedial bundle and thickness of the posterolateral bundle in the normal ACL. Knee Surg Sports Traumatol Arthrosc 19:1293–1298. doi:10.1007/s00167-011-1417-0
Kopf S, Pombo MW, Szczodry M, Irrgang JJ, Fu FH (2011) Size variability of the human anterior cruciate ligament insertion sites. Am J Sports Med 39:108–113. doi:10.1177/0363546510377399
Ziegler CG, Pietrini SD, Westerhaus BD, Anderson CJ, Wijdicks CA, Johansen S, Engebretsen L, LaPrade RF (2011) Arthroscopically pertinent landmarks for tunnel positioning in single-bundle and double-bundle anterior cruciate ligament reconstructions. Am J Sports Med 39:743–752. doi:10.1177/0363546510387511
Pietrini SD, Ziegler CG, Anderson CJ, Wijdicks CA, Westerhaus BD, Johansen S, Engebretsen L, LaPrade RF (2011) Radiographic landmarks for tunnel positioning in double-bundle ACL reconstructions. Knee Surg Sports Traumatol Arthrosc 19:792–800. doi:10.1007/s00167-010-1372-1
Otsubo H, Shino K, Suzuki D, Kamiya T, Suzuki T, Watanabe K, Fujimiya M, Iwahashi T, Yamashita T (2012) The arrangement and the attachment areas of three ACL bundles. Knee Surg Sports Traumatol Arthrosc 20:127–134. doi:10.1007/s00167-011-1576-z
Hara K, Mochizuki T, Sekiya I, Yamaguchi K, Akita K, Muneta T (2009) Anatomy of normal human anterior cruciate ligament attachments evaluated by divided small bundles. Am J Sports Med 37:2386–2391. doi:10.1177/0363546509340404
Colombet P, Robinson J, Christel P, Franceschi JP, Djian P, Bellier G, Sbihi A (2006) Morphology of anterior cruciate ligament attachments for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy 22:984–992. doi:10.1016/j.arthro.2006.04.102
Zantop T, Herbort M, Raschke MJ, Fu FH, Petersen W (2007) The role of the anteromedial and posterolateral bundles of the anterior cruciate ligament in anterior tibial translation and internal rotation. Am J Sports Med 35:223–227. doi:10.1177/0363546506294571
Lorbach O, Pape D, Maas S, Zerbe T, Busch L, Kohn D, Seil R (2010) Influence of the anteromedial and posterolateral bundles of the anterior cruciate ligament on external and internal tibiofemoral rotation. Am J Sports Med 38:721–727. doi:10.1177/0363546509353133
Markolf KL, Park S, Jackson SR, McAllister DR (2008) Contributions of the posterolateral bundle of the anterior cruciate ligament to anterior-posterior knee laxity and ligament forces. Arthroscopy 24:805–809. doi:10.1016/j.arthro.2008.02.012
Wu JL, Seon JK, Gadikota HR, Hosseini A, Sutton KM, Gill TJ, Li G (2010) In situ forces in the anteromedial and posterolateral bundles of the anterior cruciate ligament under simulated functional loading conditions. Am J Sports Med 38:558–563. doi:10.1177/0363546509350110
Fujie H, Otsubo H, Fukano S, Suzuki T, Suzuki D, Mae T, Shino K (2011) Mechanical functions of the three bundles consisting of the human anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc 19(Suppl 1):S47–S53. doi:10.1007/s00167-011-1513-1
Amis AA (2012) The functions of the fibre bundles of the anterior cruciate ligament in anterior drawer, rotational laxity and the pivot shift. Knee Surg Sports Traumatol Arthrosc 20:613–620. doi:10.1007/s00167-011-1864-7
Kato Y, Ingham SJ, Maeyama A, Lertwanich P, Wang JH, Mifune Y, Kramer S, Smolinski P, Fu FH (2012) Biomechanics of the human triple-bundle anterior cruciate ligament. Arthroscopy 28:247–254. doi:10.1016/j.arthro.2011.07.019
Wunschel M, Muller O, Lo J, Obloh C, Wulker N (2010) The anterior cruciate ligament provides resistance to externally applied anterior tibial force but not to internal rotational torque during simulated weight-bearing flexion. Arthroscopy 26:1520–1527. doi:10.1016/j.arthro.2010.04.069
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS (2010) A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 363:331–342. doi:10.1056/NEJMoa0907797
Smith TO, Davies L, Hing CB (2010) Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 18:304–311. doi:10.1007/s00167-009-0965-z
Delince P, Ghafil D (2012) Anterior cruciate ligament tears: conservative or surgical treatment? A critical review of the literature. Knee Surg Sports Traumatol Arthrosc 20:48–61. doi:10.1007/s00167-011-1614-x
Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE (2005) Treatment of anterior cruciate ligament injuries, part I. Am J Sports Med 33:1579–1602. doi:10.1177/0363546505279913
Samuelsson K, Andersson D, Karlsson J (2009) Treatment of anterior cruciate ligament injuries with special reference to graft type and surgical technique: an assessment of randomized controlled trials. Arthroscopy 25:1139–1174. doi:10.1016/j.arthro.2009.07.021
Pombo MW, Shen W, Fu FH (2008) Anatomic double-bundle anterior cruciate ligament reconstruction: where are we today? Arthroscopy 24:1168–1177. doi:10.1016/j.arthro.2008.05.021
Adachi N, Ochi M, Uchio Y, Iwasa J, Kuriwaka M, Ito Y (2004) Reconstruction of the anterior cruciate ligament. Single- versus double-bundle multistranded hamstring tendons. J Bone Joint Surg Br 86:515–520
Muneta T, Koga H, Mochizuki T, Ju YJ, Hara K, Nimura A, Yagishita K, Sekiya I (2007) A prospective randomized study of 4-strand semitendinosus tendon anterior cruciate ligament reconstruction comparing single-bundle and double-bundle techniques. Arthroscopy 23:618–628. doi:10.1016/j.arthro.2007.04.010
Jarvela T (2007) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective, randomize clinical study. Knee Surg Sports Traumatol Arthrosc 15:500–507. doi:10.1007/s00167-006-0254-z
Jarvela T, Moisala AS, Sihvonen R, Jarvela S, Kannus P, Jarvinen M (2008) Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized, clinical study with 2-year results. Am J Sports Med 36:290–297. doi:10.1177/0363546507308360
Siebold R, Dehler C, Ellert T (2008) Prospective randomized comparison of double-bundle versus single-bundle anterior cruciate ligament reconstruction. Arthroscopy 24:137–145. doi:10.1016/j.arthro.2007.11.013
Zaffagnini S, Bruni D, Russo A, Takazawa Y, Lo Presti M, Giordano G, Marcacci M (2008) ST/G ACL reconstruction: double strand plus extra-articular sling vs double bundle, randomized study at 3-year follow-up. Scand J Med Sci Sports 18:573–581. doi:10.1111/j.1600-0838.2007.00697.x
Zaffagnini S, Bruni D, Marcheggiani Muccioli GM, Bonanzinga T, Lopomo N, Bignozzi S, Marcacci M (2011) Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc 19:390–397. doi:10.1007/s00167-010-1225-y
Ibrahim SA, Hamido F, Al Misfer AK, Mahgoob A, Ghafar SA, Alhran H (2009) Anterior cruciate ligament reconstruction using autologous hamstring double bundle graft compared with single bundle procedures. J Bone Joint Surg Br 91:1310–1315. doi:10.1302/0301-620X.91B10.21886
Streich NA, Friedrich K, Gotterbarm T, Schmitt H (2008) Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc 16:232–238. doi:10.1007/s00167-007-0480-z
Sastre S, Popescu D, Nunez M, Pomes J, Tomas X, Peidro L (2010) Double-bundle versus single-bundle ACL reconstruction using the horizontal femoral position: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 18:32–36. doi:10.1007/s00167-009-0844-7
Aglietti P, Giron F, Losco M, Cuomo P, Ciardullo A, Mondanelli N (2010) Comparison between single-and double-bundle anterior cruciate ligament reconstruction: a prospective, randomized, single-blinded clinical trial. Am J Sports Med 38:25–34. doi:10.1177/0363546509347096
Suomalainen P, Moisala AS, Paakkala A, Kannus P, Jarvela T (2011) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: randomized clinical and magnetic resonance imaging study with 2-year follow-up. Am J Sports Med 39:1615–1622. doi:10.1177/0363546511405024
Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH (2012) Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med 40:512–520. doi:10.1177/0363546511426416
Suomalainen P, Jarvela T, Paakkala A, Kannus P, Jarvinen M (2012) Double-bundle versus single-bundle anterior cruciate ligament reconstruction: a prospective randomized study with 5-year results. Am J Sports Med 40:1511–1518. doi:10.1177/0363546512448177
Meredick RB, Vance KJ, Appleby D, Lubowitz JH (2008) Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med 36:1414–1421. doi:10.1177/0363546508317964
Zhu Y, Tang RK, Zhao P, Zhu SS, Li YG, Li JB (2012) Double-bundle reconstruction results in superior clinical outcome than single-bundle reconstruction. Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-012-2073-8
Endele D, Jung C, Becker U, Bauer G, Mauch F (2009) Anterior cruciate ligament reconstruction with and without computer navigation: a clinical and magnetic resonance imaging evaluation 2 years after surgery. Arthroscopy 25:1067–1074. doi:10.1016/j.arthro.2009.05.016
Papalia R, Franceschi F, Vasta S, Di Martino A, Maffulli N, Denaro V (2012) Sparing the anterior cruciate ligament remnant: is it worth the hassle? Br Med Bull. doi:10.1093/bmb/ldr053
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suomalainen, P., Kannus, P. & Järvelä, T. Double-bundle Anterior Cruciate Ligament reconstruction: a review of literature. International Orthopaedics (SICOT) 37, 227–232 (2013). https://doi.org/10.1007/s00264-012-1680-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-012-1680-9