Abstract
Paroxysmal nocturnal hemoglobinuria (PNH) is a disease with variable presentation, including classical PNH (cPNH) and PNH with aplastic anemia (AA-PNH). Here, we describe bone marrow (BM) histology related to clinical findings in 67 patients with a PNH clone. Patients were divided in AA-PNH (n = 39) and cPNH (n = 28) based on clinical criteria and were compared to 17 AA patients without PNH clone. Median PNH clone size was higher in cPNH (75 %) than in AA-PNH (10 %) (p < 0.0001). BM cellularity was normal or increased in 65 % of cPNH, while it was decreased in AA-PNH and AA (95 % and 100 %) (p < 0.0001). Myelopoiesis and megakaryopoiesis were decreased in 85 % and 100 % of AA-PNH and 100 % of AA patients, but also in 86 % and 46 % of cPNH patients, even when peripheral blood values were normal. The percentage of CD59-deficient late-stage myeloid cells determined immunohistochemically correlated to PNH granulocyte clone size. Lymphoid nodules and increased mast cell numbers were present in all groups but more frequently in AA-PNH (38 % and 73 %) than in cPNH (20 % and 43 %). BM iron was decreased in 88 % of cPNH, while it was increased in AA-PNH (64 %) and AA (100 %) (p < 0.0001). Hemolysis was present in all cPNH but also in AA-PNH patients (67 %). In conclusion, cPNH patients had more cellular BM and more prominent erythropoiesis than AA-PNH patients. Nonetheless, cPNH patients also show AA features such as myeloid and megakaryocyte hypoplasia and inflammatory infiltrates, although more subtle than in AA-PNH. No significant differences were found between BM of AA patients with and without PNH clone.
Similar content being viewed by others
Introduction
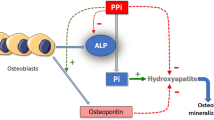
PNH is a very rare disease characterized by an acquired mutation of the PIG-A gene in the hematopoietic stem cell (HSC). The PIG-A gene product is essential in the synthesis of GPI anchors, which tether several proteins to the cell membrane. Therefore, this mutation results in a clone of blood cells with deficiency of GPI-anchored proteins at the cell membrane. Deficiency of the GPI-anchored complement inhibitors CD59 and CD55 on PNH erythrocytes renders these susceptible to complement-mediated lysis, resulting in hemolysis, the most prominent clinical feature of classical PNH (cPNH) [1].
The clinical spectrum of PNH is highly variable, ranging from cPNH patients with large clone sizes associated with severe hemolysis and a higher risk of thrombosis, to patients with relatively small clone sizes who usually do not have clinically relevant hemolysis but present with prominent pancytopenia. These latter patients often have underlying bone marrow diseases such as aplastic anemia (AA) or myelodysplastic syndromes (MDS). In fact, a PNH clone is a frequent finding in AA (20–55 % of patients) [2] and in some cases of MDS (estimated prevalence of 10 %) [3–6]. The close relationship between these diseases is further underlined by the fact that PNH frequently evolves from AA or rarely vice versa during the course of disease [7].
Immune-mediated BM failure is proposed as a common pathogenetic mechanism explaining the pancytopenia encountered in AA and MDS with a PNH clone, but also frequently in cPNH. Although usually more overt in AA and MDS, bi- or pancytopenia is found in 20–30 % of all PNH patients [7–9]. The observation that AA patients with a small PNH clone appear to respond better to immune suppressive therapy than those without supports a role for immune-mediated BM failure in PNH [4, 10]. In addition, oligoclonal T cell populations with potential autoreactivity towards the HSC were detected in patients with AA, PNH, and MDS [11–16]. The expansion of a PNH clone, which is observed in some AA patients in the course of disease, may be attributed to selective immune-mediated damage to normal HSC and not GPI-deficient HSC [17, 18]. A higher degree of apoptosis in normal HSC compared to GPI-deficient HSC further supports this hypothesis [19–21].
The current working classification for PNH as proposed by the International PNH interest group (IPIG) distinguishes cPNH, PNH in the setting of another specified BM disorder, diagnosed at any time, and subclinical PNH [1]. Patients with clinical PNH may be treated with the complement inhibitor eculizumab which effectively blocks intravascular hemolysis [22–24]; if the underlying bone marrow disease prevails, immune suppressive drugs may be considered. The IPIG classification however does not adequately represent the heterogeneous clinical picture of PNH. For example, cPNH patients may also have (mild) cytopenias. In addition, the clinical picture often changes in the course of disease, as patients with AA can progress to clinical PNH and sometimes vice versa. These factors complicate diagnosis and treatment decisions.
The IPIG recommends a full BM examination at diagnosis of PNH for classification and exclusion of other BM failure syndromes. However, a comprehensive overview of the spectrum of BM histology in patients with a PNH clone in different presentations is still unavailable. In this study, we aim to provide such an overview in a large series of patients. To this end, we divided patients with a PNH clone in two groups based on clinical picture and peripheral blood counts: one group with peripheral blood counts fulfilling criteria of aplastic anemia (AA-PNH) and the other having clinical or laboratory evidence of hemolysis and peripheral blood counts not fulfilling those criteria (cPNH). Histology was correlated with clinical features such as hemolysis and PNH clone size. To investigate differences between AA patients with a PNH clone and those without, a group of AA patients without PNH clone was included. Finally, we have assessed the utility of CD59 as a marker to assess GPI deficiency in the various lineages and stages of hematopoietic differentiation in BM biopsies by CD59 immunohistochemical stainings.
Methods
Patient characteristics
We reviewed 67 diagnostic bone marrow biopsies (BMB) of all patients with a PNH clone who presented at the Radboud University Nijmegen Medical Centre (RUNMC) (n = 58) or the Hospices Civils de Lyon (n = 8) between 1991 and 2010. BMB of patients with a PNH clone and evidence of MDS were excluded. The study was approved by the RUNMC medical ethical committee.
To evaluate differences in bone BM histology in the different presentations of PNH, patients were divided in two groups based on peripheral blood counts. The first group (n = 39) was composed of patients with a PNH clone and peripheral blood counts fulfilling the criteria for aplastic anemia as defined by the International Agranulocytosis and Aplastic Anemia Study Group [25], i.e., at least two out of the following: untransfused hemoglobin <100 g/l, platelet count <50 × 109/l, and/or neutrophil count <1.5 × 109/l in the absence of other causes. In the second group (n = 28), patients with clinical evidence of intravascular hemolysis and peripheral blood counts not fulfilling the criteria of AA were included. Henceforward, in this article, these two patient groups will be referred to as AA-PNH and cPNH, respectively. BMB of AA-PNH and cPNH patients were compared to an age-matched control group consisting of AA patients (n = 17) who never developed a PNH clone. Non-severe AA (NSAA), severe AA (SAA), and very severe AA (VSAA) were defined according to previously published guidelines [26].
PNH clone size was determined by flow cytometric measurement of the percentage of granulocytes in the peripheral blood with deficiency of at least two GPI-anchored proteins or fluorescently labeled aerolysin (FLAER), according to standards at the time of diagnosis [1]. Data on PNH granulocyte clone size as assessed by flow cytometry, hemolysis parameters, and peripheral blood counts at diagnosis were collected and correlated to histological findings such as cellularity, iron stores, and the presence of hypoplasia in different lineages. The presence of hemolysis was defined as increased lactate dehydrogenase (LDH) and decreased or undetectable haptoglobin levels. Hemolysis parameters were assessed at first detection of the PNH clone. The clinical disease was also followed in time.
Histology
Slides of BMB embedded in paraffin and/or plastic were received from several referral centers and were evaluated without knowledge of the clinical data. Stainings that were evaluated included hematoxylin and eosin (H&E), periodic acid-Schiff (PAS), Leder, Giemsa, Laguesse or Gomori, and iron stains.
Cellularity was defined as the percentage of BM space occupied by cells other than fat cells. The age-related cellularity was defined as normal (<40 years: 50–70 %; 40–60 years: 40–60 %; >60 years: 30–50 %), decreased or increased [27, 28]. The ratio between myeloid and erythroid cells (ME ratio) was defined as normal when between 4 and 1. Erythroid hyperplasia was defined as a predominance of erythroid precursors over myeloid cells (ME ratio < 1). Fibrosis was graded according to Thiele et al. [29].
Inflammatory cells were evaluated by counting the average number of mast cells per high power field (HPF, 40×) in at least ten fields and recording the number of lymphoid nodules and increased numbers of plasma cells (at least three groups of >8 cells). The slides of eight PNH BMB (n = 3 cPNH, n = 5 AA-PNH) were stained with an antibody to mast cell tryptase (clone AA1, DAKO, Cambridgeshire, UK) to check for degranulated mast cells that are not identified by Giemsa staining.
CD59 immunohistochemical staining
To determine the percentage of GPI-deficient cells in the various lineages and stages of hematopoietic differentiation, an immunohistochemical CD59 staining was performed on BMB of five cPNH, three AA-PNH patients with sufficient cellularity, and five healthy control BMB. CD59 was chosen as it is expressed at high levels in all lineages and stages of differentiation in the bone marrow [30].
Antigen retrieval was performed in pH 6.0 sodium citrate at 96 °C on 4 μm thick paraffin embedded BMB sections. After blocking of endogenous peroxidase, slides were exposed to the primary CD59 antibody (Clone MEM43/5, Exbio, Vestec, Czech Republic) for 1 h at room temperature. After incubation with the secondary HRP-conjugated goat anti-mouse/rabbit/rat antibody (PowerVision, Immunologic, Duiven, the Netherlands), slides were developed with DAB and counterstained with hematoxylin. CD59 negative cells were microscopically analyzed and scored by the morphological appearance of megakaryocytes, late-stage myeloid, plasma cells, erythrons, and capillaries.
Statistical analysis
Fisher's exact test or Chi-square test was used to determine differences between the frequency of histological characteristics in the AA-PNH versus the cPNH and in the AA-PNH versus the AA group. Linear regression analysis was performed to determine correlations between clinical parameters and/or histological parameters.
Results
Clinical characteristics of the AA-PNH, cPNH, and AA patients without a PNH clone are summarized in Table 1. Histological features are summarized in Table 2.
Clinical features
Median follow-up of cPNH patients was 3 years (range 0.5–19 years), 4 years for AA-PNH patients (range 0.5–20 years), and 2 years (range 0.25–12.5 years) for AA patients. 91 % of cPNH, 73 % of AA-PNH, and 65 % of AA patients were alive at the end of follow-up. Median age at diagnosis was comparable in the three groups at 37, 35, and 40 years for AA-PNH, cPNH, and AA with a similar range. In the AA-PNH and AA groups, men and women were about equally distributed, whereas the cPNH group had a higher proportion of men (61 %).
The size of the PNH granulocyte clone at diagnosis was significantly different (p < 0.0001, unpaired t test) in AA-PNH and cPNH with medians of 10 % (range 1–100 %) and 75 % (range 8–100 %), respectively. While the vast majority of cPNH patients (85 %) had PNH granulocyte clones of more than 30 %, this was only the case in 34 % of the AA-PNH group. PNH clones below 10 % were almost exclusively detected in the AA-PNH group (39 % of AA-PNH patients) compared to only one patient in the cPNH group (Table 1). This particular patient had only laboratory evidence of hemolysis, a PNH granulocyte clone of 8 %, and completely normal peripheral blood counts, whereas his BM was hypocellular.
In the majority of AA-PNH patients (26/39, 67 %), the PNH clone was detected at first presentation. In the remaining 13/39 (33 %) of AA-PNH patients, the presence of a PNH clone was either not assessed by flow cytometry at disease onset or detected later in the course of disease (median duration from disease onset to first detection of the PNH clone 0.8 years, range 0.25–3 years).
Patients in the cPNH group had by definition clinical (hemoglobinuria, jaundice) and/or laboratory evidence of hemolysis (LDH ≥ 450 U/L, decreased haptoglobin). Hemolysis was also observed in 67 % of patients who presented with AA-PNH. However, compared to the cPNH group, hemolysis was generally mild, and LDH levels were lower (median 482 U/L in AA-PNH versus 1,940 U/L in cPNH). In the majority of AA-PNH patients, hemolysis was subclinical and only detected by elevated LDH levels and/or undetectable haptoglobin levels (in 54 % and 55 % of AA-PNH patients, respectively). A significant correlation (r 2 0.22, p < 0.0001, linear regression analysis) between LDH levels and PNH granulocyte clone size was found in the combined AA-PNH and cPNH patient group (Supplementary Fig. 1).
cPNH patient BMB have normal to increased cellularity, erythroid hyperplasia, and myeloid hypoplasia whereas AA-PNH patients show hypocellular BM with myeloid and erythroid hypoplasia. a–b, d BMB of a 71-year-old male cPNH patient, showing increased BM cellularity and erythroid hyperplasia (a HE 5×, b HE 20×) and myeloid hypoplasia (d Leder staining 5×). c BMB of a 61-year-old male AA-PNH patient with overall patchy BM cellularity and central BM spaces with less than 5 % cellularity and hemosiderosis (HE 2.5×)
Cytogenetic abnormalities were found in the BM of three of 30 AA-PNH patients (loss of the Y chromosome in two patients in 15 % of metaphases, monosomy 21 in 3 % in the other), in one of 19 cPNH patients examined (trisomy 8 in 1.5 % of cells by FISH analysis), and in one of 12 AA patients (t 5;13 in 20/20 metaphases). None of the patients with cytogenetic abnormalities had abnormalities in BM morphology (data not shown) and histology consistent with a diagnosis of MDS, nor did they develop MDS later during follow-up (median 2.5 years, range 1–7 years).
One AA-PNH patient developed chronic myelomonocytic leukemia (CMML), another refractory anemia with excess blasts (MDS-RAEB), 5 and 3 years after initial diagnosis of AA-PNH, respectively. Remarkably, in both cases, the PNH clone could not be detected anymore at the time of CMML/MDS diagnosis, suggesting that the malignant clone did not arise from the PNH clone. None of the cPNH patients developed hematological malignancies in the course of the disease. One AA patient developed a T cell large granular lymphocytic leukemia 1 year after diagnosis of AA.
Bone marrow cellularity
As expected, in the AA-PNH group, cellularity was decreased in 95 % of patients. The cPNH group differed significantly from the AA-PNH group with decreased cellularity present in only 36 % of patients (p < 0.0001, Chi-square test). Instead, most cPNH patients had a normal (29 %) to hypercellular (36 %) BM that was dominated by a hyperplastic erythropoiesis (Fig. 1a, b). We found no differences in peripheral blood WBC, platelet count, or PNH clone size between cPNH patients with normal or increased versus those with decreased BM cellularity (data not shown). By definition, all AA patients had decreased BM cellularity. In 82 % of AA-PNH and 100 % of AA patients, the BM showed patchy areas with <10 % cellularity (Fig. 1c), whereas in only 2 (7 %) of cPNH patients, this was the case. Relative erythroid hyperplasia with ME ratios ranging from 1 to 0.2 was seen in the majority of cPNH (86 %), AA-PNH (76 %), and evaluable AA patients (50 %). However, an absolute increase in erythropoiesis was predominantly observed in cPNH patients (64 %, Fig. 1a, b) compared to only 13 % of AA-PNH patients (p < 0.0001, Fisher's exact test) and none in AA.
Interestingly, in the cPNH patient group, despite a hypercellular BM, myeloid hypoplasia was histologically present in the vast majority of patients (86 %) (Fig. 1d), even in those with normal absolute neutrophil (ANC > 1.5 × 109/l) and white blood cell (WBC) counts (>3.5 × 109/l). In only 9 of 24 cPNH patients (38 %) with myeloid hypoplasia, neutropenia and/or leukopenia was observed. Myeloid hypoplasia was frequently observed in AA-PNH BMB (85 %) and in all AA patients. The remaining AA-PNH patients showed a left-shifted myelopoiesis. Both the prevalence (74 %, 20 %, and 94 % for AA-PNH, cPNH and AA respectively) and severity of peripheral blood neutropenia were generally higher in the AA-PNH group compared to the cPNH group and highest in the AA group (Table 1). In the AA-PNH group, the majority of patients (82 %) had non-severe AA (NSAA), and the remainder had severe AA (SAA). In the AA group, AA was non-severe in 24 %, severe in 47 %, and very severe in 29 % of patients.
The number of megakaryocytes was decreased in 13/28 (46 %) cPNH patients. In the majority of these patients (9/13, 69 %), megakaryocyte hypoplasia corresponded to mild peripheral blood thrombocytopenia (platelet count between 50 and 150 × 109/l). In the other four patients with megakaryocyte hypoplasia, normal platelet counts were found. Significantly different from cPNH (p < 0.0001), megakaryocytes were decreased or absent in all patients with AA-PNH and AA. This was also reflected in more severe thrombocytopenia in AA-PNH and AA patients (<50 × 109/L in 87 % and 88 %, and between 50 and 150 × 109/L in 13 % and 12 % of AA-PNH and AA, respectively) than in cPNH patients.
Inflammatory infiltrates
Lymphoid nodules were more frequently observed in AA-PNH (38 %) compared to cPNH (20 %; p = 0.05, Fisher’s exact test) and AA patients (13 %; p = 0.02, Fisher’s exact test) (Fig. 2a, b). In the patients with lymphoid nodules and available immunohistochemical stains (n = 3; 2 AA-PNH, 1 cPNH), lymphoid nodules were shown to consist of either B and T cells (n = 2, Fig. 2c) or T cells only (n = 1). In ten AA-PNH patients and three cPNH patients, large numbers of interstitial T cells (n = 10, Fig. 2d), or B and T cells (n = 4) were found.
Lymphoid nodules and/or increased numbers of T cells are mainly present in AA-PNH patient BMB. a–b BMB of two different AA-PNH patients showing lymphoid nodules (arrows) (a 61-year-old male, HE 2.5×, b 67-year-old female, HE 10×). c Immunohistochemical staining of the same BMB as a showing that the lymphoid nodule consists of B cells (CD20, 5×). d Immunohistochemical staining of a BMB of a 42-year-old female with AA-PNH, showing a diffuse T cell infiltration throughout the BM (CD3, 10×)
Increased numbers of mast cells were observed more often in AA-PNH (73 %) than in cPNH (43 %; p = 0.05, Fisher's exact test) (Fig. 3a, b). Up to an average of ten mast cells/HPF were seen. Although anti-tryptase immunohistochemistry was more sensitive than the Giemsa stain in detecting mast cells (overall average 5.9 compared to 2.8 cells/HPF with Giemsa), both stains correlated well in eight BMB tested (r 2 0.93, p < 0.0001, linear regression analysis, Fig. 3b). The AA control group did not differ significantly from the AA-PNH group with 76 % of patients having increased mast cells. The plasma cell infiltrate in the AA-PNH group was comparable to the AA group with 17 % and 20 % of patients having an increased number of plasma cells, respectively. One of the patients in the AA-PNH group fulfilled the clinical diagnosis of monoclonal gammopathy of unknown significance (MGUS). By flow cytometric analysis, it was determined that the plasma cells in this patient did not belong to the PNH clone (data not shown). None of the cPNH patients had an increased number of plasma cells.
Comparison of increased numbers of mast cells in AA-PNH BMB by conventional and immunohistochemical staining. BMB of a 48-year-old female AA-PNH patient showing increased numbers of mast cells (average number 5.4 cells/HPF) in Giemsa staining 40× (a) and 11.1 cells/HPF in tryptase staining 40× (b). Correlation between average numbers of mast cells/HPF counted in Giemsa staining (x-axis) and average numbers of mast cells/HPF counted in anti-tryptase stainings (y-axis) (c)
Iron
The majority of both AA-PNH (64 %) and AA patients (100 %) had increased iron stores in macrophages. In contrast, iron was decreased or completely absent in 88 % of cPNH patients, significantly differing from AA-PNH patients (p < 0.0001). In AA-PNH patients with decreased iron, no correlation was found with the presence of hemolysis (p = 0.43, Fisher's exact test).
Hemorrhage and congestion
Congestion of BM sinusoids was present in both AA-PNH (55 %, Fig. 4a), cPNH (73 %, Fig. 4b), and AA patients (75 %). In part of these patients (52 % of AA-PNH, 59 % of PNH), large numbers of mature erythrocytes were found extravascularly in otherwise intact BM specimens, possibly representing vascular damage and resulting hemorrhage. There was no correlation with either low platelet counts or use of anticoagulant medication (data not shown).
Congestion of blood vessels is a frequent finding in both AA-PNH and cPNH patients. a Congested blood vessel (arrow) in an AA-PNH BMB containing both intact and possibly lysed erythrocytes (Giemsa 40×). b Large numbers of mature erythrocytes present in the interstitium in otherwise intact specimen of a cPNH patient (b) (Giemsa 20×)
CD59 staining
In all AA-PNH (n = 3) and cPNH BMB (n = 5) tested, CD59-deficient late-stage myeloid cells (median 92 % and 60 % respectively), erythrons (median 80 % and 96 %), and megakaryocytes (median 85 % and 75 %) dominated. In contrast, in healthy controls, CD59-negative late-stage myeloid cells, erythrons, megakaryocytes, and plasma cells were rarely detected (medians 1 %, 0 %, 16 % and 0 %, respectively, Table 3, Fig. 5). The percentage of CD59-deficient late-stage myeloid cells as determined by immunohistochemistry correlated to the peripheral blood PNH granulocyte clone size as measured by flow cytometry (r 2 0.53, p = 0.03, linear regression analysis, Fig. 5e). The percentage of CD59-deficient plasma cells was highly variable but generally lower than the percentage of CD59-deficient cells in other lineages (Table 3). Interestingly, similar to healthy controls, capillaries in AA-PNH and cPNH patients were uniformly strongly positive, indicating that endothelial cells in PNH BM are not derived from GPI-deficient hematopoietic stem cells (Table 3, Fig. 5). The staining pattern of CD59 was not only membranous but also cytoplasmic in all positive cells, both from PNH patients and controls.
CD59 expression in the bone marrow of PNH patients and controls. CD59 immunohistochemistry on BMB of cPNH, AA-PNH patients, and healthy controls. a Overview of CD59 staining in a BMB of a 36-year-old male AA-PNH patient (left panel) with the majority of cells CD59 negative (blue), but strongly positive (brown) endothelial cells, compared to a healthy control (right panel) with expression of CD59 on all cells (20×). b Both CD59 positive (left panel) and CD59 negative (right panel) erythrons in a 35-year-old female cPNH patient (40×). c (Arrows from left to right, 40×): CD59 positive myeloid cells (left two arrows), CD59 negative megakaryocyte, CD59 positive plasma cells surrounding CD59 positive endothelial cells, and CD59 negative myeloid cells (right two arrows) in an 18-year-old female cPNH patient. d CD59 positive megakaryocyte in a 35-year-old female cPNH patient (40×). e PNH granulocyte clone size in the blood (percent) versus CD59 negative late stage myeloid cells in the BMB determined by CD59 immunohistochemistry (percent)
Discussion
The clinical spectrum of PNH is highly variable, ranging from patients with predominant hemolysis to patients with prominent BM failure without clinically relevant hemolysis. Here, we reviewed BMB of 67 patients with a PNH clone, subdivided in cPNH and AA-PNH based on clinical characteristics. Although AA-PNH and cPNH patients have obvious differences in BM histology, these patient groups also show remarkable histological similarities.
We observed decreased overall cellularity in almost all AA-PNH patients, whereas cellularity was increased in the majority of cPNH patients, mainly due to a strongly enhanced erythropoiesis. However, despite increased erythropoiesis, some cPNH patients show overall decreased BM cellularity. Theoretically, this interesting group may represent patients at an earlier stage of disease currently undergoing clonal expansion, and thus having a smaller PNH clone. Alternatively, these patients may currently develop AA. However, neither peripheral blood values nor clone sizes were lower in cPNH patients with decreased cellularity versus those with normal or increased cellularity, arguing against this hypothesis. Concurrent viral infections could be an alternative explanation in occasional patients. A prospective study and longer follow-up is required to see whether these patients are more prone to develop AA in the future.
As expected, we found an absolute decrease of the myeloid lineage in the AA-PNH and AA group. Myeloid hypoplasia was however also observed in the majority of cPNH patients, even in those with normal WBC counts. In cPNH patients, myeloid hypoplasia was often masked by a strongly increased erythropoiesis, resulting in an overall normal or increased BM cellularity. In addition, megakaryopoiesis was also decreased in 46 % of cPNH patients, even in occasional patients with normal platelet counts. Histological findings thus confirm that BM hypoplasia is a frequent feature of cPNH, although more subtle, not always clinically apparent and easily overlooked due to the prominent erythropoiesis. These results are possibly biased by the fact that a BMB is more likely performed in cPNH patients with cytopenias.
Our findings underline that the current working classification for PNH is of limited clinical utility. According to the IPIG classification, classic PNH patients do not have a defined bone marrow abnormality. Yet, in this study, marrow hypoplasia was demonstrated in the vast majority of cPNH patients. Thus, discriminating PNH in the setting of another BM disorder and classic PNH is extremely difficult. Hypoplasia in cPNH patients is usually subtle, and the clinical picture often does not correspond to BM findings. In such cases, our finding of areas of severely hypocellular BM interspersed with areas of normal cellularity, which occurred almost exclusively in AA-PNH, might contribute to the distinction with cPNH.
Diagnosis of BM failure disease relies on integrated histological, morphological, cytogenetic, and clinical findings. In this study, unfortunately, we did not have the opportunity to revise BM aspirate morphology. We excluded patients who were diagnosed with MDS at or before the time of PNH diagnosis. None but two patients developed MDS during follow-up; however, at that time, the PNH clone had disappeared. Therefore, we think it is unlikely that our cohort contained MDS patients at the time of diagnosis of PNH. However, we may have missed subtle morphological abnormalities insufficient to diagnose MDS. As shown by Araten et al. [31], such abnormalities are often found in patients with a PNH clone. Also in AA, dyserythropoiesis is a frequent finding [32]. We identified cytogenetic abnormalities in 9 % of patients with a PNH clone, which was less frequent than in the series of Araten et al. [31]. Especially in patients with a hypocellular BM, a BMB has additional value in excluding or confirming MDS as another means to assess cellularity, the presence of fibrosis, abnormally localized immature precursors (ALIPs), and increases in CD34+ blast counts [33, 34]. In our study, none of the patients had increased CD34+ blast percentages (immunohistochemical staining available in 37 %), fibrosis, or ALIPs.
Interestingly, in this study, we found a pronounced presence of inflammatory infiltrates involving increased mast cells, lymphoid nodules, and plasma cells in the AA and AA-PNH BMB, but also in some cases of cPNH. Previous studies already showed oligoclonal T cell expansions in peripheral blood in AA, AA-PNH, and cPNH [11–16]. The T cell infiltrates found in some AA-PNH and cPNH patients in our study fit the hypothesis of T cell-mediated BM damage in PNH. Increased BM mast cells and plasma cells were previously reported in various BM failure syndromes, including PNH [35–37]. These may suggest an additional role of the B cell compartment and innate immunity in the suppression of hematopoiesis in AA-PNH. Several autoantibodies have been found in AA and AA-PNH; however, a causal role for these antibodies was never proven [38–42].
The mechanism behind the expansion of PIG-A mutated HSC in PNH at the expense of normal HSC remains elusive. As supported by evidence from several experimental studies, immune-mediated BM failure may play a role in PNH clonal expansion by selective damage to normal HSC. Confirming other studies [43, 44], we found larger PNH clones in cPNH than in AA-PNH patients. In addition, in cPNH, we found a higher BM cellularity and significantly less pronounced signs of inflammation. These differences may reflect variations in the nature or timing of HSC injury. In this series, lymphoid nodules were also less frequent in AA than in AA-PNH. No other significant clinical or histological differences were found between AA-PNH and AA patients that might account for the occurrence of a PNH clone in AA-PNH.
In 67 % of AA-PNH patients, hemolysis was recorded, and by definition in all cPNH patients. As shown previously, the degree of hemolysis as determined by LDH levels correlated with PNH clone size [44]. Bone marrow iron stores were decreased in most cPNH patients, probably due to increased hematopoiesis and iron loss by hemoglobinuria. In contrast, the majority of AA-PNH patients had increased iron deposition in BM macrophages. This is unlikely to be explained by transfusions since in this study diagnostic BMB were evaluated. Alternatively, decreased iron usage due to diminished hematopoiesis may lead to excess deposition in macrophages, as described in other conditions of ineffective hematopoiesis. Impaired erythropoiesis may also result in increased growth differentiation factor 15 (GDF15) levels which block hepcidin production leading to increased iron absorption in the gut [45].
The remarkable finding of congested blood vessels and hemorrhage in the majority of BMB in all patient groups is unexplained. This phenomenon was previously described in a series of aplastic anemia, however in that study, the presence of a PNH clone could not be assessed reliably as flow cytometry was not available yet [36]. It could point to an inflammatory response with subsequent endothelial damage and may be aggravated by thrombocytopenia. Complement-mediated damage of GPI-deficient endothelial cells is an unlikely explanation, as we show that endothelial cells uniformly express CD59 in both AA-PNH and cPNH.
Our results on CD59 expression in a limited set of healthy and patient BMB indicate that CD59 is a useful marker to immunohistochemically assess GPI deficiency in sufficiently cellular BMB. The cytoplasmic staining in addition to the membranous expression was unexpected but a well-known pattern for several other anti-CD59 antibodies [46]. The reason for this cytoplasmic staining is unknown. A variable intensity of the positive staining cells can be attributed to varying expression levels for CD59 in PNH cells, as is known from flow cytometry. A partial deficiency in GPI anchors (type II cells) results in a lower expression of CD59, while type III cells are completely devoid of CD59. Interestingly, both in AA-PNH and cPNH, compared to other lineages, plasma cells contained a lower percentage of CD59 negative cells. Others have previously shown smaller PNH lymphocyte clones than red cell and granulocyte clones, possibly explained by the longer life span of lymphocytes, which were generated before the onset of PNH [47]. In contrast to peripheral blood, where the PNH erythrocyte clone is smaller than the PNH granulocyte clone size due to continuous lysis of PNH red cells, we did not find a similar difference between the proportion of GPI-deficient erythroid precursors and late-stage myeloid cells in BM. This is consistent with the previous observation that in PNH patients the proportion of GPI-deficient cells in reticulocytes is comparable to neutrophils and higher than in erythrocytes [48]. It might indicate that complement-mediated destruction of PNH red cells mainly takes place in the peripheral blood and not in the BM.
To our knowledge, this is the first large series describing various aspects of BM histology in patients with a PNH clone. We have demonstrated that BM histology at presentation cannot clearly differentiate between AA and AA-PNH. cPNH and AA-PNH however are obviously different with respect to a lower BM cellularity and a more pronounced inflammatory infiltrate in AA-PNH. When looking more closely though, cPNH resembles AA-PNH more than initially apparent, as AA features, such as myeloid and megakaryocyte hypoplasia, increased inflammatory cells and decreased cellularity are also found in many cPNH patients. This further contributes to the notion that both entities need to be considered as different ends of a continuous spectrum of immune-mediated BM failure syndromes rather than separate entities as the current clinical working classification suggests.
Reference
Parker C, Omine M, Richards S, Nishimura J, Bessler M, Ware R, Hillmen P, Luzzatto L, Young N, Kinoshita T, Rosse W, Socie G (2005) Diagnosis and management of paroxysmal nocturnal hemoglobinuria. Blood 106(12):3699–3709
Schrezenmeier H, Hertenstein B, Wagner B, Raghavachar A, Heimpel H (1995) A pathogenetic link between aplastic anemia and paroxysmal nocturnal hemoglobinuria is suggested by a high frequency of aplastic anemia patients with a deficiency of phosphatidylinositol glycan anchored proteins. Exp Hematol 23(1):81–87
Iwanaga M, Furukawa K, Amenomori T, Mori H, Nakamura H, Fuchigami K, Kamihira S, Nakakuma H, Tomonaga M (1998) Paroxysmal nocturnal haemoglobinuria clones in patients with myelodysplastic syndromes. Br J Haematol 102(2):465–474
Wang H, Chuhjo T, Yasue S, Omine M, Nakao S (2002) Clinical significance of a minor population of paroxysmal nocturnal hemoglobinuria-type cells in bone marrow failure syndrome. Blood 100(12):3897–3902
Wang SA, Pozdnyakova O, Jorgensen JL, Medeiros LJ, Stachurski D, Anderson M, Raza A, Woda BA (2009) Detection of paroxysmal nocturnal hemoglobinuria clones in patients with myelodysplastic syndromes and related bone marrow diseases, with emphasis on diagnostic pitfalls and caveats. Haematologica 94(1):29–37
Dunn DE, Tanawattanacharoen P, Boccuni P, Nagakura S, Green SW, Kirby MR, Kumar MS, Rosenfeld S, Young NS (1999) Paroxysmal nocturnal hemoglobinuria cells in patients with bone marrow failure syndromes. Ann Intern Med 131(6):401–408
Hillmen P, Lewis SM, Bessler M, Luzzatto L, Dacie JV (1995) Natural history of paroxysmal nocturnal hemoglobinuria. N Engl J Med 333(19):1253–1258
de Latour RP, Mary JY, Salanoubat C, Terriou L, Etienne G, Mohty M, Roth S, de Guilbert S, Maury S, Cahn JY, Socie G (2008) Paroxysmal nocturnal hemoglobinuria: natural history of disease subcategories. Blood 112(8):3099–3106
Socie G, Mary JY, de Gramont A, Rio B, Leporrier M, Rose C, Heudier P, Rochant H, Cahn JY, Gluckman E (1996) Paroxysmal nocturnal haemoglobinuria: long-term follow-up and prognostic factors. French Society of Haematology. Lancet 348(9027):573–577
Sugimori C, Chuhjo T, Feng X, Yamazaki H, Takami A, Teramura M, Mizoguchi H, Omine M, Nakao S (2006) Minor population of CD55–CD59-blood cells predicts prognosis and response to immunosuppressive therapy in patients with aplastic anemia. Blood 107(4):1308–1314
Karadimitris A, Manavalan JS, Thaler HT, Notaro R, Araten DJ, Nafa K, Roberts IA, Weksler ME, Luzzatto L (2000) Abnormal T-cell repertoire is consistent with immune process underlying the pathogenesis of paroxysmal nocturnal hemoglobinuria. Blood 96(7):2613–2620
Risitano AM, Kook H, Zeng W, Chen G, Young NS, Maciejewski JP (2002) Oligoclonal and polyclonal CD4 and CD8 lymphocytes in aplastic anemia and paroxysmal nocturnal hemoglobinuria measured by V beta CDR3 spectratyping and flow cytometry. Blood 100(1):178–183
Risitano AM, Maciejewski JP, Green S, Plasilova M, Zeng W, Young NS (2004) In-vivo dominant immune responses in aplastic anaemia: molecular tracking of putatively pathogenetic T-cell clones by TCR beta-CDR3 sequencing. Lancet 364(9431):355–364
Wlodarski MW, Gondek LP, Nearman ZP, Plasilova M, Kalaycio M, Hsi ED, Maciejewski JP (2006) Molecular strategies for detection and quantitation of clonal cytotoxic T-cell responses in aplastic anemia and myelodysplastic syndrome. Blood 108(8):2632–2641
Gargiulo L, Lastraioli S, Cerruti G, Serra M, Loiacono F, Zupo S, Luzzatto L, Notaro R (2007) Highly homologous T-cell receptor beta sequences support a common target for autoreactive T cells in most patients with paroxysmal nocturnal hemoglobinuria. Blood 109(11):5036–5042
Risitano AM, Maciejewski JP, Muranski P, Wlodarski M, O'Keefe C, Sloand EM, Young NS (2005) Large granular lymphocyte (LGL)-like clonal expansions in paroxysmal nocturnal hemoglobinuria (PNH) patients. Leukemia 19(2):217–222
Murakami Y, Kosaka H, Maeda Y, Nishimura J, Inoue N, Ohishi K, Okabe M, Takeda J, Kinoshita T (2002) Inefficient response of T lymphocytes to glycosylphosphatidylinositol anchor-negative cells: implications for paroxysmal nocturnal hemoglobinuria. Blood 100(12):4116–4122
Hanaoka N, Kawaguchi T, Horikawa K, Nagakura S, Mitsuya H, Nakakuma H (2006) Immunoselection by natural killer cells of PIGA mutant cells missing stress-inducible ULBP. Blood 107(3):1184–1191
Chen R, Nagarajan S, Prince GM, Maheshwari U, Terstappen LW, Kaplan DR, Gerson SL, Albert JM, Dunn DE, Lazarus HM, Medof ME (2000) Impaired growth and elevated fas receptor expression in PIGA(+) stem cells in primary paroxysmal nocturnal hemoglobinuria. J Clin Invest 106(5):689–696
Chen G, Zeng W, Maciejewski JP, Kcyvanfar K, Billings EM, Young NS (2005) Differential gene expression in hematopoietic progenitors from paroxysmal nocturnal hemoglobinuria patients reveals an apoptosis/immune response in 'normal' phenotype cells. Leukemia 19(5):862–868
Chen G, Kirby M, Zeng W, Young NS, Maciejewski JP (2002) Superior growth of glycophosphatidy linositol-anchored protein-deficient progenitor cells in vitro is due to the higher apoptotic rate of progenitors with normal phenotype in vivo. Exp Hematol 30(7):774–782
Hillmen P, Hall C, Marsh JC, Elebute M, Bombara MP, Petro BE, Cullen MJ, Richards SJ, Rollins SA, Mojcik CF, Rother RP (2004) Effect of eculizumab on hemolysis and transfusion requirements in patients with paroxysmal nocturnal hemoglobinuria. N Engl J Med 350(6):552–559
Schubert J, Hillmen P, Roth A, Young NS, Elebute MO, Szer J, Gianfaldoni G, Socie G, Browne P, Geller R, Rother RP, Muus P (2008) Eculizumab, a terminal complement inhibitor, improves anaemia in patients with paroxysmal nocturnal haemoglobinuria. Br J Haematol 142(2):263–272
Hillmen P, Young NS, Schubert J, Brodsky RA, Socie G, Muus P, Roth A, Szer J, Elebute MO, Nakamura R, Browne P, Risitano AM, Hill A, Schrezenmeier H, Fu CL, Maciejewski J, Rollins SA, Mojcik CF, Rother RP, Luzzatto L (2006) The complement inhibitor eculizumab in paroxysmal nocturnal hemoglobinuria. N Engl J Med 355(12):1233–1243
(1987) Incidence of aplastic anemia: the relevance of diagnostic criteria. By the International Agranulocytosis and Aplastic Anemia Study: Blood 70(6):1718–1721
Marsh JC, Ball SE, Cavenagh J, Darbyshire P, Dokal I, Gordon-Smith EC, Keidan J, Laurie A, Martin A, Mercieca J, Killick SB, Stewart R, Yin JA (2009) Guidelines for the diagnosis and management of aplastic anaemia. Br J Haematol 147(1):43–70
Hartsock RJ, Smith EB, Petty CS (1965) Normal variations with aging of the amount of hematopoietic tissue in bone marrow from the anterior iliac crest. A study made from 177 cases of sudden death examined by necropsy. Am J Clin Pathol 43:326–331
Ogawa T, Kitagawa M, Hirokawa K (2000) Age-related changes of human bone marrow: a histometric estimation of proliferative cells, apoptotic cells, T cells, B cells and macrophages. Mech Ageing Dev 117(1–3):57–68
Thiele J, Kvasnicka HM, Facchetti F, Franco V, van der Walt J, Orazi A (2005) European consensus on grading bone marrow fibrosis and assessment of cellularity. Haematologica 90(8):1128–1132
Hernandez-Campo PM, Almeida J, Matarraz S, de Santiago M, Sanchez ML, Orfao A (2007) Quantitative analysis of the expression of glycosylphosphatidylinositol-anchored proteins during the maturation of different hematopoietic cell compartments of normal bone marrow. Cytometry B Clin Cytom 72(1):34–42
Araten DJ, Swirsky D, Karadimitris A, Notaro R, Nafa K, Bessler M, Thaler HT, Castro-Malaspina H, Childs BH, Boulad F, Weiss M, Anagnostopoulos N, Kutlar A, Savage DG, Maziarz RT, Jhanwar S, Luzzatto L (2001) Cytogenetic and morphological abnormalities in paroxysmal nocturnal haemoglobinuria. Br J Haematol 115(2):360–368
Frisch B, Lewis SM (1974) The bone marrow in aplastic anaemia: diagnostic and prognostic features. J Clin Pathol 27(3):231–241
Bennett JM, Orazi A (2009) Diagnostic criteria to distinguish hypocellular acute myeloid leukemia from hypocellular myelodysplastic syndromes and aplastic anemia: recommendations for a standardized approach. Haematologica 94(2):264–268
Horny HP, Sotlar K, Valent P (2007) Diagnostic value of histology and immunohistochemistry in myelodysplastic syndromes. Leuk Res 31(12):1609–1616
Prokocimer M, Polliack A (1981) Increased bone marrow mast cells in preleukemic syndromes, acute leukemia, and lymphoproliferative disorders. Am J Clin Pathol 75(1):34–38
Te Velde J, Haak HL (1977) Aplastic anaemia. Histological investigation of methacrylate embedded bone marrow biopsy specimens; correlation with survival after conventional treatment in 15 adult patients. Br J Haematol 35(1):61–69
Leguit RJ, Van Den Tweel JG (2010) The pathology of bone marrow failure. Histopathology 57(5):655–670
Feng X, Chuhjo T, Sugimori C, Kotani T, Lu X, Takami A, Takamatsu H, Yamazaki H, Nakao S (2004) Diazepam-binding inhibitor-related protein 1: a candidate autoantigen in acquired aplastic anemia patients harboring a minor population of paroxysmal nocturnal hemoglobinuria-type cells. Blood 104(8):2425–2431
Hirano N, Butler MO, Guinan EC, Nadler LM, Kojima S (2005) Presence of anti-kinectin and anti-PMS1 antibodies in Japanese aplastic anaemia patients. Br J Haematol 128(2):221–223
Hirano N, Butler MO, Von Bergwelt-Baildon MS, Maecker B, Schultze JL, O'Connor KC, Schur PH, Kojima S, Guinan EC, Nadler LM (2003) Autoantibodies frequently detected in patients with aplastic anemia. Blood 102(13):4567–4575
Alahmad A, Preuss KD, Schenk J, Fureder W, Schrezenmeier H, Muller-Lantzsch N, Schubert J, Pfreundschuh M (2010) Desmoplakin and KIF20B as target antigens in patients with paroxysmal nocturnal haemoglobinuria. Br J Haematol 151(3):273–280
Takamatsu H, Feng X, Chuhjo T, Lu X, Sugimori C, Okawa K, Yamamoto M, Iseki S, Nakao S (2006) Specific antibodies to moesin, a membrane-cytoskeleton linker protein, are frequently detected in patients with acquired aplastic anemia. Blood 109(6):2514–2520
Scheinberg P, Marte M, Nunez O, Young NS (2010) Paroxysmal nocturnal hemoglobinuria clones in severe aplastic anemia patients treated with horse anti-thymocyte globulin plus cyclosporine. Haematologica 95(7):1075–1080
Maciejewski JP, Rivera C, Kook H, Dunn D, Young NS (2001) Relationship between bone marrow failure syndromes and the presence of glycophosphatidyl inositol-anchored protein-deficient clones. Br J Haematol 115(4):1015–1022
Tanno T, Miller JL (2010) Iron loading and overloading due to ineffective erythropoiesis. Adv Hematol 2010:358283
The Human Protein Atlas (http://www.proteinatlas.org/ENSG00000085063/normal/bone+marrow)
Piedras J, Lopez-Karpovitch X (2000) Flow cytometric analysis of glycosylphosphatidyl-inositol-anchored proteins to assess paroxysmal nocturnal hemoglobinuria clone size. Cytometry 42(4):234–238
Ware RE, Rosse WF, Hall SE (1995) Immunophenotypic analysis of reticulocytes in paroxysmal nocturnal hemoglobinuria. Blood 86(4):1586–1589
Acknowledgments
We thank all pathologists who have contributed to this study by providing BMB of patients with a PNH clone for revision and all hematologists who referred patients to us. Professor Dr Gérard Socié, Hôpital Saint Louis, Paris, is thanked for helpful advice.
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Fig. 1
Correlation between LDH levels and PNH granulocyte clone size. PNH granulocyte clone size (%) versus LDH levels (U/l) in the total group of AA-PNH and cPNH patients with available LDH levels at the time of first detection of the PNH clone (n = 64). Each dot represents a single patient. r 2 and p value were calculated by linear regression analysis (TIFF 324 kb)
Rights and permissions
About this article
Cite this article
van Bijnen, S.T.A., Ffrench, M., Kruijt, N. et al. Bone marrow histology in patients with a paroxysmal nocturnal hemoglobinuria clone correlated with clinical parameters. J Hematopathol 6, 71–82 (2013). https://doi.org/10.1007/s12308-013-0179-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12308-013-0179-7