Abstract
Background
Morbid obesity results in marked respiratory pathophysiologic changes that may lead to impaired intraoperative gas exchange. The decelerating inspiratory flow and constant inspiratory airway pressure resulting from pressure-controlled ventilation (PCV) may be more adapted to these changes and improve gas exchanges compared with volume-controlled ventilation (VCV).
Methods
Forty morbidly obese patients scheduled for gastric bypass were included in this study. Total intravenous anesthesia was given using the target-controlled infusion technique. During the first intraoperative hour, VCV was used and the tidal volume was adjusted to keep end-tidal PCO2 around 35 mmHg. After 1 h, patients were randomly allocated to 30-min VCV followed by 30-min PCV or the opposite sequence using a Siemens® Servo 300. FiO2 was 0.6. During PCV, airway pressure was adjusted to provide the same tidal volume as during VCV. Arterial blood was sampled for gas analysis every 15 min. Ventilatory parameters were also recorded.
Results
Peak inspiratory airway pressures were significantly lower during PCV than during VCV (P < 0.0001). The other ventilatory parameters were similar during the two periods of ventilation. PaO2 and PaCO2 were not significantly different during PCV and VCV.
Conclusion
PCV does not improve gas exchange in morbidly obese patients undergoing gastric bypass compared to VCV.
Similar content being viewed by others
Introduction
Atelectasis develops immediately after the induction of general anesthesia and increases intraoperative shunt leading to impairment of gas exchange and potentially to hypoxemia [1, 2]. Morbid obesity results in several pathophysiologic changes of the respiratory system mechanics that promote the development of intraoperative atelectasis and exaggerate the impairment of gas exchange [3, 4]. As a consequence, arterial oxygenation is inversely related to body mass index (BMI) [4].
Several ventilatory strategies have been proposed to prevent atelectasis and improve arterial oxygenation in morbidly obese patients, but remain controversial. The use of large tidal volumes produced conflicting results [3, 5, 6]. Pelosi et al. reported that application of a 10-cm H2O positive end-expiratory pressure (PEEP) increases PaO2 in morbidly obese patients [7]. This beneficial effect was not found by other authors [8]. Preoperative continuous positive airway pressure followed by 5-min mechanical ventilation with PEEP before intubation prevents atelectasis formation and subsequently improves arterial oxygenation [9, 10]. However many practitioners advocate the use of a rapid sequence induction without ventilation in morbidly obese patients [11]. Preoxygenation with 60% oxygen concentration was shown to reduce the size of atelectasis in nonobese patients compared to 100% oxygen concentration [12]. This measure is however debatable in morbidly obese patients, as their markedly reduced functional residual capacity shortens the duration of nonhypoxic apnea. Finally, alveolar recruitment maneuver combined with PEEP also improves arterial oxygenation. However, this strategy results in hemodynamic alterations requiring vasopressor administration during laparoscopic bariatric surgery [13].
Volume-controlled ventilation (VCV) with constant flow rate is the most commonly used ventilatory mode during anesthesia. Pressure-controlled ventilation (PCV) is one of the strategies proposed to improve gas exchange in hypoxic intensive care unit patients, especially those with adult respiratory distress syndrome [14]. Indeed, during PCV, pressure gradient between the proximal airway and the alveoli is maximal at the beginning of the inspiration and the bulk of the tidal volume is delivered early during the inspiratory phase, which potentially facilitates recruitment of unstable alveoli [15]. Moreover, compared to VCV with the same tidal volume and inspiratory time, PCV tends to produce higher mean airway pressures [16] and thereby can improve arterial oxygenation [17]. Finally, keeping the inspiratory pressure constant reduces ventilatory inhomogeneities by allowing redistribution of the tidal volume from alveoli with low time constant to alveoli with longer time constant [15]. Morbidly obese patients who have decreased lung volumes, decreased pulmonary compliance, and increased airway resistance are especially prone to intraoperative hypoxemia. During mechanical ventilation, they develop both increased pulmonary ventilation–perfusion mismatches and pulmonary atelectasis [3, 4, 18], which make them good candidates to benefit from the characteristics of PCV. We therefore tested the hypothesis that PCV improves intraoperative gas exchange in morbidly obese patients compared with VCV.
Materials and Methods
After approval of the Institution Ethics Committee of CHU de Liège (Liège, Belgium) and written informed consent, we enrolled 40 ASA II–III patients scheduled for Roux-en-Y gastric bypass surgery. The laparoscopic approach was used in 16 patients whereas open surgery was performed in the 24 remaining patients.
Anesthesia
After an overnight fasting, all patients were orally premedicated with 10 mg domperidone, 150 mg ranitidine, 50 mg hydroxyzine, and 0.5 mg alprazolam 2 h before surgery. Anesthesia was standardized in all patients. After a 5-min preoxygenation and denitrogenation period with 100% oxygen, a rapid sequence induction of anesthesia was used. Propofol and remifentanil were administered using a target-controlled infusion technique (propofol: Schnider’s model and remifentanil: Minto’s model). Succinylcholine 1 mg kg−1 was used to facilitate tracheal intubation with an orotracheal tube of 8 mm diameter. Propofol effect-site concentration first set at 6 μg/ml was then adjusted to keep the bispectral index of the electroencephalogram (BIS™, Aspect Medical Systems, A-2000 monitor, averaging time = 30 s, Newton, MA, USA) around 40. Remifentanil effect-site concentration first set at 4.5 ng/ml was then titrated to keep the mean arterial pressure within 15% of preinduction values or between 90 and 105 mmHg if the preinduction mean arterial pressure was superior to 110 mmHg. If necessary, nicardipine was titrated to treat hypertension, but no cardiovascular medication known to affect the BIS of the electroencephalogram and/or metabolism (β-blocking agents, clonidine, …) were administered intraoperatively. A radial artery was catheterized after the induction of anesthesia to monitor arterial pressure and to draw blood samples for blood gas analysis. Intraoperative muscle relaxation was achieved with cis-atracurium 0.15 mg/kg followed by a continuous infusion of 2 μg kg−1 min−1; full muscle relaxation (no response to train of four stimulation) was maintained during surgery (NMT, Datex-Ohmeda S/5 monitor [Datex-Ohmeda, Helsinki, Finland]). Esophageal temperature was continuously monitored. Core temperature was kept above 36.0°C using a forced air warming blanket (Bair Hugger®) 15 min before anesthesia and during the surgery. Ringer’s lactate solution (750 ml/h) was infused throughout surgery.
Ventilation
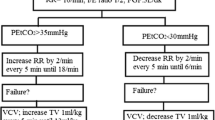
After orotracheal intubation lungs were ventilated using a Siemens® Servo 300 ventilator (Siemens, Solna, Sweden). During the first intraoperative hour, VCV was used. The respiratory rate was set to 12/min and the tidal volume was adjusted to maintain end-tidal carbon dioxide tension (PETCO2) around 35 mmHg. The FiO2 was set to 0.6 (air/oxygen mixture), as it was associated with a mean PaO2 of 150 mmHg in a preliminary study. The inspiratory time over the expiratory time ratio (I/E ratio) was 1:2. An inspiratory pause equal to 25% of the inspiratory time was used during VCV. One hour after the beginning of surgery, intraoperative conditions were considered stable, i.e., patient position (10° head-up position), intraabdominal CO2 pressure, or retractors traction were not changed anymore. Patients were then randomly assigned to VCV for 30 min followed by PCV for another 30-min period (VCPC group) or to the opposite sequence of these modes of ventilation (PCVC group). Randomization was performed using the online randomizer (Graphpad software, San Diego, CA, USA). During VCV, ventilatory parameters were kept unchanged. During PCV, the insufflation time equaled the inspiratory time of VCV. The inspiratory pressure was then adjusted to provide the same tidal volume as in VCV. A PEEP of 5 cm H2O was applied only in case of hypoxemia (SpO2 < 90%) and maintained thereafter. During both ventilation periods, the depth of anesthesia assessed by the BIS of the electroencephalogram, the effect-site concentrations of propofol and remifentanil, and muscle relaxation were not changed.
Parameters
Systolic, diastolic, and mean arterial blood pressures; heart rate; PETCO2; SpO2; BIS value; and core temperature were continuously monitored on a Datex-Ohmeda S/5 monitor (Datex-Ohmeda, Helsinki, Finland). The peak, plateau, and mean inspiratory airway pressures were measured at each ventilatory cycle by the Siemens® Servo 300 ventilator. All these parameters were recorded every 15-min during the study period. At the same times, arterial blood samples were drawn to measure PaCO2 and PaO2. Intrinsic PEEP was measured by maintaining an expiratory pause for 10 s.
Statistical Analysis
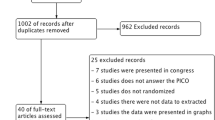
Our estimate sample size was based on PaO2 measured in a pilot study using similar protocol (mean PaO2 = 158 mmHg with a SD of 46 mmHg). For five intensivists of our institution, a 30-mmHg difference in PaO2 would be clinically significant. Thirty-eight patients would thus provide an 80% power for detecting a 30-mmHg difference between the PaO2 of each ventilation period at an alpha level of 0.05.
Data are presented as the means ± SDs unless otherwise stated and were compared using paired Student’s t test or ANOVA for repeated measures when appropriate (Graphpad Software Prism 4.0c). Relationships between initial PaO2 or BMI and difference in PaO2 between PCV and VCV were analyzed using linear regression. P ≤ 0.05 was considered statistically significant.
Results
Patient data are presented in Table 1. Hemodynamic and anesthesia parameters were similar during VCV and PCV (Table 2). Peak inspiratory airway pressures were significantly (P < 0.001) lower during PCV than during VCV, but the other ventilatory parameters were similar during both ventilatory periods (Table 3). An intrinsic PEEP (3.0 ±1.2 cm H2O) was detected in six patients but remained similar during VCV and PCV. A 5-cm H2O extrinsic PEEP was applied in two patients with hypoxemia during the stabilization period before the measurements and resulted in the improvement of SpO2.
Mean PaO2 and mean PaCO2 were not significantly affected by the ventilatory mode (Fig. 1). However, individual responses to PCV were highly variable (Fig. 2). In ten patients, PaO2 increased by more than 30 mmHg at the end of the 30-min PCV compared to the end of the 30-min VCV, whereas in eight patients, PaO2 decreased by more than 30 mmHg at the end of the 30-min PCV. In the other 22 patients, changes in PaO2 remained within 30 mmHg.
No correlation was found between PaO2 measured at the beginning of the study period and the difference between PaO2 measured at the end of the 30-min PCV and at the end of the 30-min VCV (ΔPaO2PCV30 − VCV30; P = 0.87; Fig. 3a). The ΔPaO2PCV30 − VCV30 tends to be positively correlated with BMI although not significantly (P = 0.15; Fig. 3b).
Gender did not affect the ΔPaO2PCV30 − VCV30 : 10 ± 42 mmHg vs 3.5 ± 42 mmHg for males and females, respectively (P = 0.631). The changes in PaO2 during 30-min PCV were not significantly different in both groups: ΔPaO2 PCV30 − PCV0 = 4.7 ± 7 vs 25 ± 10 mmHg ΔPaO2 in the PC–VC and VC–PV groups, respectively (P = 0.1).
PaO2 and PaCO2 were not significantly different between the two ventilation periods whatever the surgical approach, laparotomy or laparoscopy (Fig. 4). However, PaO2 (P < 0.001) and PaCO2 (P < 0.0001) were significantly greater during laparoscopy than during laparotomy.
Effects of the surgical approach, laparotomy (Tomy; open symbols) or laparoscopy (Scopy; black symbols), on the changes in PaO2 (a) and PaCO2 (b) during the 30-min periods of VCV (squares) or PCV (circles). Data are presented as the means ± SDs; n = 24 for laparotomy and n = 16 for laparoscopy. Only the SDs of the PCV groups are shown for clarity; the SDs of both groups are similar. No significant differences between PCV and VCV. Significant differences between laparotomy and laparoscopy for PaO2 (P < 0.001) and for PaCO2 (P < 0.0001)
Discussion
This study demonstrates that PCV does not improve gas exchange compared to VCV in morbidly obese patients undergoing abdominal surgery. Mean and plateau airway pressures are similar during both ventilation periods.
In this study, all the ventilatory parameters were kept identical during PCV and VCV except the insufflation flow pattern. The change in insufflation flow pattern alone did not significantly affect gas exchange in our morbidly obese patients. Other ventilatory parameters should be adjusted to take advantage of the decelerating inspiratory flow during PCV. Benefits of PCV would partly result from increased mean airway pressure compared to VCV [15, 16]. In our study, however, mean airway pressures were similar during both ventilation periods. Although we prolonged the insufflation time during PCV to equal the inspiratory time set during VCV, the insufflation time was maybe still too short to allow equilibration of pressures in the lungs and to increase mean airway pressure [17, 19]. Accordingly, Lessard et al. compared VCV and PCV with I/E ratios of 1:2, 2:1, and 3:1 in ARDS patients. VCV and PVC 1:2 resulted in comparable mean airway pressures. On the contrary, when the I/E ratio was increased to 2:1, mean airway pressure became higher during PCV than during VCV [20]. Increasing the inspiratory time could also prolong the residency time of oxygen in the alveoli and consequently improve oxygenation. The impact of the inspiratory time is probably more crucial in case of lungs with heterogeneous time constants, a likely situation in anesthetized morbidly obese patients [21]. In such conditions, short insufflation times hamper ventilation of alveoli with long time constants [22]. Finally, PCV with an I/E ratio of 1:2 did not result in intrinsic PEEP compared to VCV. Intrinsic PEEP was however proposed to participate in gas exchange improvement during PCV [23]. Together, all these data suggest that the insufflation flow pattern of PCV is not effective alone to increase arterial oxygen tension in morbidly obese patients undergoing abdominal surgery but might need to be associated with prolonged I/E ratio to improve gas exchange. Accordingly, studies reporting better arterial oxygen tension during PCV used prolonged inspiratory times [15]. In this regard, monitoring the flow curve is helpful in adjusting the insufflation time during PCV to allow the end-inspiratory flow to reach down zero [24].
In our study, we did not apply any extrinsic PEEP, except in the case of hypoxemia to avoid the introduction of an additional confounding parameter. PEEP is however helpful in maintaining the alveoli opened, decreases total respiratory system resistance in obese patients [7], and might thereby facilitate pressures equilibration in the lungs during PCV and improve gas exchange. Whether the potential benefit of PEEP would be greater during PCV than during VCV has not been investigated.
Gas exchanges were measured 1 h after the beginning of surgery and more than 90 min after the induction of anesthesia to allow stabilization of all factors potentially affecting ventilatory mechanics and metabolism. Atelectasis develops within a few minutes after the induction of anesthesia particularly when patients are preoxygenated with 100% oxygen like in our study [12]. Eradication of these atelectases requires sustained period of ventilation with high airway pressures [25]. Therefore, PCV without high levels of PEEP would have not been effective in reversing these atelectases even if initiated immediately after the induction of anesthesia.
Although there were no significant differences between the means of PaO2 during the two ventilation periods, it should be noted that the PaO2 of half the patients was nevertheless improved by PCV, sometimes markedly. Because of the variability in the response to PCV, we consider it is worth to test this ventilatory mode in case of hypoxemia developing in morbidly obese patients. We examined whether the initial PaO2 or the BMI might predict patient responsiveness to PCV. No significant correlations between each of these two parameters on one hand and the change in PaO2 induced by PCV on the other hand were however observed [24]. Finally, the surgical approach, laparoscopy vs laparotomy, did not affect the effect of PCV on PaO2. PaO2 and PaCO2 were greater during laparoscopy than laparotomy. Reduced venous admixture during laparoscopy [26] and CO2 absorption during CO2-pneumoperitoneum [27] explain these observations.
PCV allows suppressing the peak inspiratory pressure compared to VCV. This results from the different insufflation flow patterns used in each of these modes of ventilation. The airway pressure during PCV and the plateau airway pressure during VCV were however similar. Nevertheless, the suppression of the peak airway pressure during PCV might limit heterogeneous ventilation of lungs with heterogeneous time constants, i.e., reduced overdistension and overpressure in short time constant bronchoalevolar units [24]. This condition may exist in some morbidly obese patients.
In conclusion, we demonstrated that if all ventilatory parameters during PCV and VCV are kept similar, the different inspiratory flow used in each of these two modes of ventilation does not significantly affect gas exchange in morbidly obese patients undergoing abdominal surgery. However, the variability in the response to PCV does not preclude from testing this mode of ventilation in case of intraoperative hypoxemia developing in these patients.
References
Duggan M, Kavanagh BP. Pulmonary atelectasis: a pathogenic perioperative entity. Anesthesiology 2005;102:838–54.
Hedenstierna G, Edmark L. The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med 2005;31:1327–35.
Shenkman Z, Shir Y, Brodsky JB. Perioperative management of the obese patient. Br J Anaesth 1993;70:349–59.
Pelosi P, Croci M, Ravagnan I, et al. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg 1998;87:654–60.
Bardoczky GI, Yernault JC, Houben JJ, et al. Large tidal volume ventilation does not improve oxygenation in morbidly obese patients during anesthesia. Anesth Analg 1995;81:385–8.
Sprung J, Whalley DG, Falcone T, et al. The effects of tidal volume and respiratory rate on oxygenation and respiratory mechanics during laparoscopy in morbidly obese patients. Anesth Analg 2003;97:268–74.
Pelosi P, Ravagnan I, Giurati G, et al. Positive end-expiratory pressure improves respiratory function in obese but not in normal subjects during anesthesia and paralysis. Anesthesiology 1999;91:1221–31.
Santesson J. Oxygen transport and venous admixture in the extremely obese. Influence of anaesthesia and artificial ventilation with and without positive end-expiratory pressure. Acta Anaesthesiol Scand 1976;20:387–94.
Gander S, Frascarolo P, Suter M, et al. Positive end-expiratory pressure during induction of general anesthesia increases duration of nonhypoxic apnea in morbidly obese patients. Anesth Analg 2005;100:580–4.
Coussa M, Proietti S, Schnyder P, et al. Prevention of atelectasis formation during the induction of general anesthesia in morbidly obese patients. Anesth Analg 2004;98:1491–5.
Adams JP, Murphy PG. Obesity in anaesthesia and intensive care. Br J Anaesth 2000;85:91–108.
Edmark L, Kostova-Aherdan K, Enlund M, et al. Optimal oxygen concentration during induction of general anesthesia. Anesthesiology 2003;98:28–33.
Whalen FX, Gajic O, Thompson GB, et al. The effects of the alveolar recruitment maneuver and positive end-expiratory pressure on arterial oxygenation during laparoscopic bariatric surgery. Anesth Analg 2006;102:298–305.
Al-Saady N, Bennett ED. Decelerating inspiratory flow waveform improves lung mechanics and gas exchange in patients on intermittent positive-pressure ventilation. Intensive Care Med 1985;11:68–75.
Campbell RS, Davis BR. Pressure-controlled versus volume-controlled ventilation: does it matter? Respir Care 2002;47:416–24.
Markstrom AM, Lichtwarck-Aschoff M, Svensson BA, et al. Ventilation with constant versus decelerating inspiratory flow in experimentally induced acute respiratory failure. Anesthesiology 1996;84:882–9.
Marini JJ, Ravenscraft SA. Mean airway pressure: physiologic determinants and clinical importance—part 2: clinical implications. Crit Care Med 1992;20:1604–16.
Pelosi P, Croci M, Ravagnan I, et al. Total respiratory system, lung, and chest wall mechanics in sedated–paralyzed postoperative morbidly obese patients. Chest 1996;109:144–51.
Marini JJ, Ravenscraft SA. Mean airway pressure: physiologic determinants and clinical importance—part 1: physiologic determinants and measurements. Crit Care Med 1992;20:1461–72.
Lessard MR, Guerot E, Lorino H, et al. Effects of pressure-controlled with different I:E ratios versus volume-controlled ventilation on respiratory mechanics, gas exchange, and hemodynamics in patients with adult respiratory distress syndrome. Anesthesiology 1994;80:983–91.
Pelosi P, Croci M, Ravagnan I, et al. Respiratory system mechanics in sedated, paralyzed, morbidly obese patients. J Appl Physiol 1997;82:811–8.
El-Khatib MF, Jamaleddine G. Mean alveolar pressure during constant-flow and constant-pressure inflation of diseased lungs. Respir Care 2001;46:678–85.
Yanos J, Watling SM, Verhey J. The physiologic effects of inverse ratio ventilation. Chest 1998;114:834–8.
Nichols D, Haranath S. Pressure control ventilation. Crit Care Clin 2007;23:183–99; viii–ix.
Rothen HU, Sporre B, Engberg G, et al. Re-expansion of atelectasis during general anaesthesia: a computed tomography study. Br J Anaesth 1993;71:788–95.
Andersson L, Lagerstrand L, Thorne A, et al. Effect of CO(2) pneumoperitoneum on ventilation–perfusion relationships during laparoscopic cholecystectomy. Acta Anaesthesiol Scand 2002;46:552–60.
Joris JL, Noirot DP, Legrand MJ, et al. Hemodynamic changes during laparoscopic cholecystectomy. Anesth Analg 1993;76:1067–71.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hans, G.A., Prégaldien, A.A., Kaba, A. et al. Pressure-controlled Ventilation Does Not Improve Gas Exchange in Morbidly Obese Patients Undergoing Abdominal Surgery. OBES SURG 18, 71–76 (2008). https://doi.org/10.1007/s11695-007-9300-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-007-9300-2