Abstract
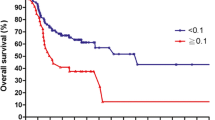
The lymph node ratio (LNR) combines two types of information—about the extent of neck dissection and about the extent of the pathological examination of the specimen—and thus represents an interesting variable for risk assessment in patients with head and neck cancer. This retrospective study with data from January 1, 1980, to December 31, 2010, evaluates the utility of the LNR as a potential prognostic predictor in patients with laryngeal squamous cell carcinoma (LSCC). A total of 202 consecutive patients with regionally metastasized LSCC who underwent primary surgery with or without adjuvant treatment were included. The mean follow-up period was 4.4 years. The LNR was calculated as the ratio of positive nodes to the total number of nodes removed during neck dissection. Multivariate analysis was carried out. Peak values as averaged clusters of individual LNRs were registered at three points (LNR 0.05, 0.07, and 0.09). LNR 0.09 was a significant prognostic parameter in the Cox regression model (P = 0.007). Patients with an LNR > 0.09 had a hazard ratio of 2.065 for a disease-specific survival event in comparison with LNR < 0.09. The most accurate LNR for LSCC is expected to be located in the range of 0.08–0.1. The LNR seems to be of limited value for the decision-making process in the treatment of patients with LSCC, in comparison with other locations. Prospective trials will be required in order to allow evidence-based recommendations for treatment decisions based on the LNR.





Similar content being viewed by others
References
Mamelle G, Pampurik J, Luboinski B, Lancar R, Lusinchi A, Bosq J (1994) Lymph node prognostic factors in head and neck squamous cell carcinomas. Am J Surg 168:494–498
Lanzer M, Kruse A, Lübbers HT, Zemann W, Reinisch S (2012) Lymph node ratio and capsule penetration as independent risk factors in head and neck squamous cell carcinoma. Head Neck Oncol 4:89
Liao CT, Hsueh C, Lee LY et al (2012) Neck dissection field and lymph node density predict prognosis in patients with oral cavity cancer and pathological node metastases treated with adjuvant therapy. Oral Oncol 48:329–336
Kim SY, Nam SY, Choi SH, Cho KJ, Roh JL (2012) Prognostic value of lymph node density in node-positive patients with oral squamous cell carcinoma. Ann Surg Oncol 18:2310–2317
Ebrahimi A, Clark JR, Zhang WJ et al (2011) Lymph node ratio as an independent prognostic factor in oral squamous cell carcinoma. Head Neck 33:1245–1251
Shrime MG, Bachar G, Lea J et al (2009) Nodal ratio as an independent predictor of survival in squamous cell carcinoma of the oral cavity. Head Neck 31:1482–1488
Gil Z, Carlson DL, Boyle JO et al (2009) Lymph node density is a significant predictor of outcome in patients with oral cancer. Cancer 115:5700–5710
Urban D, Gluck I, Pfeffer MR, Symon Z, Lawrence YR (2013) Lymph node ratio predicts the benefit of post-operative radiotherapy in oral cavity cancer. Radiother Oncol 106:74–79
Künzel J, Psychogios G, Mantsopoulos K, Grundtner P, Waldfahrer F, Iro H. (2013) Lymph node ratio as a predictor of outcome in patients with oropharyngeal cancer. Eur Arch Otorhinolaryngol Jun 19
Moe K, Wolf GT, Fisher SG, Hong WK (1996) Regional metastases in patients with advanced laryngeal cancer. Department of Veterans affairs laryngeal cancer study group. Arch Otolaryngol Head Neck Surg 122:644–648
Wittekind C (2010) 2010 TNM system: on the 7th edition of TNM classification of malignant tumors. Pathologe 31:331–332. German
Bernier J, Domenge C, Ozsahin M et al (2004) Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med 350:1945–1952
Cooper JS, Pajak TF, Forastiere AA et al (2004) Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med 350:1937–1944
Heagerty PJ, Lumley T, Pepe MS (2000) Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics 56:337–344
Concato J, Peduzzi P, Holfold TR et al (1995) Importance of events per independent variable in proportional hazards analysis. I. Background, goals, and general strategy. J Clin Epidemiol 48:1495–1501
Vittinghoff E, McCulloch CE (2007) Relaxing the rule of ten events per variable in logistic and cox regression. Am J Epidemiol 165:710–718
Pantel M, Guntinas-Lichius O (2012) [Laryngeal carcinoma: epidemiology, risk factors and survival]. HNO 60:32–40. German
Ferlito A, Silver CE, Rinaldo A, Smith RV (2000) Surgical treatment of the neck in cancer of the larynx. ORL J Otorhinolaryngol Relat Spec 62:217–225
Ganly I, Patel SG, Matsuo J et al (2009) Predictors of outcome for advanced-stage supraglottic laryngeal cancer. Head Neck 31:1489–1495
Spector GJ, Sessions DG, Lenox J, Newland D, Simpson J, Haughey BH (2004) Management of stage IV glottic carcinoma: therapeutic outcomes. Laryngoscope 114:1438–1446
Guntinas-Lichius O, Wendt T, Buentzel J et al (2010) Head and neck cancer in Germany: a site-specific analysis of survival of the Thuringian cancer registration database. J Cancer Res Clin Oncol 136:55–63
Sessions DG, Lenox J, Spector GJ (2005) Supraglottic laryngeal cancer: analysis of treatment results. Laryngoscope 115:1402–1410
Ferlito A, Rinaldo A, Devaney KO et al (2002) Prognostic significance of microscopic and macroscopic extracapsular spread from metastatic tumor in the cervical lymph nodes. Oral Oncol 38:747–751
Psychogios G, Mantsopoulos K, Koch M et al (2013) Elective neck dissection vs observation in transorally treated early head and neck carcinomas with cN0 neck. Acta Otolaryngol 133:313–317
Psychogios G, Mantsopoulos K, Bohr C, Koch M, Zenk J, Iro H (2013) Incidence of occult cervical metastasis in head and neck carcinomas: development over time. J Surg Oncol 107:384–387
Wang YL, Feng SH, Zhu J et al (2013) Impact of lymph node ratio on the survival of patients with hypopharyngeal squamous cell carcinoma: a population-based analysis. PLoS ONE 8:e56613
Acknowledgments
The authors would like to thank Mr. Philipp Grundtner for the management and statistical analysis of the data.
Conflict of interest
The author and contributing authors hereby state that there were no conflicts of interest during the preparation of this study and there are no financial disclosures to make.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Künzel, J., Mantsopoulos, K., Psychogios, G. et al. Lymph node ratio is of limited value for the decision-making process in the treatment of patients with laryngeal cancer. Eur Arch Otorhinolaryngol 272, 453–461 (2015). https://doi.org/10.1007/s00405-014-2997-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-014-2997-3