Abstract
Until now, the anatomic extent of tumor (TNM classification) has been, by far, the most important factor to predict the prognosis of colorectal cancer patients. However, in recent years, data collected from large cohorts of human cancers demonstrated that the immune contexture of the primary tumors is an essential prognostic factor for patients' disease-free and overall survival. Global analysis of tumor microenvironment showed that the nature, the functional orientation, the density, and the location of adaptive immune cells within distinct tumor regions influence the risk of relapse events. An immune classification of the patients was proposed based on the density and the immune cell location within the tumor. The immune classification has a prognostic value that is superior to the TNM classification, and tumor invasion is statistically dependent on the host immune reaction. Tumor and immunological markers predicted by systems biology methods are involved in the shaping of an efficient immune reaction and can serve as targets for novel therapeutic approaches. Thus, the strength of the immune reaction could advance our understanding of cancer evolution and have important consequences in clinical practice.
Similar content being viewed by others
TNM staging: T is for T cells and M is for memory [1]
The outcome prediction in cancer is usually achieved by evaluating tissue samples obtained during surgical removal of the primary tumor, mostly focusing on their histological characteristics. These include an atypical cell morphology, tissue integrity, aberrant expression of markers of malignant transformation, senescence and proliferation, various characteristics of the invasive margin (IM), depth of invasion, and the extent of vascularization. In addition, histological or radiological analysis of both, tumor-draining and regional lymph nodes, as well as of distant organs can be carried out looking for evidence of metastases. Based on these data, the evaluation of cancer progression is performed and further serves to estimate the patient prognosis. Available statistical data of patients with similar progression characteristics and their actual outcome parameters such as average disease-free (DFS), disease-specific (DSS), and overall survival (OS) are used for the estimation. Until now, tumor staging (AJCC/UICC-TNM classification) summarizes data on tumor burden (T), presence of cancer cells in draining and regional lymph nodes (N), and evidence for metastases (M). With the large amount of statistical data available on cancer patients' survival with a given progression stage, such approaches have been shown to be valuable in estimating the outcome in cancer [2–4].
Still, it is well known that the cancer outcome can significantly vary between patients within the same histological tumor stage. The progression of advanced-stage cancer can remain stable for years, and partial or full regression of large metastatic lesions can also occur spontaneously. For example, considering only the chest metastatic tumors, 76 reports have demonstrated spontaneous regression [5]. The most common primary tumors were renal cell carcinoma, and also hepatocellular carcinoma, endometrial stromal sarcoma, pleomorphic liposarcoma, and esophageal cancer. Similarly, spontaneous regression of metastases from melanoma, and spontaneous remissions in colorectal cancer (CRC) metastases were shown [6, 7].
On the other hand, the rapid relapse and death of early cancer patients were reported, even after an apparently complete surgical removal of the tumor, with undetectable levels of residual tumor burden and without signs of metastasis. One reason for the limited accuracy of the traditional staging in predicting the outcome of the patients could be the usual estimation of the tumor progression as a largely autonomous process, focusing only on cancer cells and without considering the evolution of the cancer as a balance of factors which can enhance or suppress the tumor [8].
Recently, many reports supporting the hypothesis that cancer development is strongly influenced by the host's immune system were published [8, 9]. This underlines the importance of the systemic and local immunological markers that even at the level of clinically apparent tumors should be evaluated in predicting the outcome [8, 10]. Moreover, such markers were shown to be superior to the AJCC/UICC-TNM staging in estimating DFS, DSS, and OS [11–13]. In fact, the conventional histological criteria were dependent on the intratumoral immune reaction of the host, particularly on cytotoxic and memory T cells [1].
The infiltration of the center (CT) and of the IM of the tumor by cytotoxic CD8+ and memory CD45RO + T cells was shown to have a prognostic discriminatory power superior to standard staging systems AJCC/UICC-TNM. The quantification of those tumor-infiltrating T cells, allowed to define a novel scoring system with strong correlation with clinical outcome. This immune-based score ranges from 4 (high density of CD8+ and CD45RO + T cells in CT and IM) to 0. Those results demonstrate several key findings. First, patients with high immune scores have increased disease-free and overall survival as compared with low immune scored patients. The immune score is superior in predicting the disease outcome as compared to clinical parameters, including TNM staging. Second, there is an inverse correlation between immune cell density and tumor stage. The growth of the primary tumor and the metastatic spread were associated with decreased intratumoral immune T-cell density. The most infiltrated tumors were in majority (60%) in situ or T1 stage tumors. In contrast, only 18% of T4 tumors were high T cell infiltrated. Moreover, there were no tumors in situ or T1 stage showing weak immune cell density, whereas 45% of T4 tumors had low immune scores. Thus, it is likely that a strong intratumoral immune response protects against tumor progression, and a minimal tumor burden is associated with high densities of CD8+ and GZMB + cytotoxic T cells. Third, in patients who did not relapse, the density of CD8-infiltrates was inversely correlated with T stage. In contrast, in patients with recurrence, the number of CD8+ cells was low regardless of the T stage of the tumor. Thus, the data suggest that even in the case of a minimal tumor invasion, patients with a low immune score will be likely to experience a disease relapse. For these patients, surgery may not be curative. Remarkably, the prognostic power of the immune score was retained regardless of whether the tumor tissue was obtained from a CRC patient with stage I or stage IV [11, 13].
A novel classification of colorectal cancer patients based on the immune score
In multivariate Cox analyses for DFS, DSS, and OS, we showed that the immune parameters remained significant, whereas the histopathological parameters did not (including T stage and N stage) [11, 13]. Thus, based on the inverse interrelation between the immune density and the tumor stage, it can be hypothesized that the prognostic value of the TNM staging could partially reflect the quality and density of infiltrating immune cells. Whether or not immune cells are directly implicated in the control of tumor dissemination is not answered. However, it is tempting to think that a weak in situ immune infiltrate reflects a defect of the host response to the tumor challenge. This leads to an inefficient control of early metastatic (tumor emboli) and possibly to a defect in the generation of systemic effectors capable of controlling the micrometastatic disease in lymph nodes, peripheral blood, peritoneal cavity, or bone marrow [14]. Interestingly, the long-lasting anti-tumor capacities of memory T cells have been shown in a mouse model of colon carcinoma metastases [15]. Those cells are maintained in the body for long periods of time.
In the view of our results [11, 13, 16], it could be wise to include immune markers to evaluate the prognosis of CRC patients. Given the fact that the assessment of intratumoral cytotoxic and memory T lymphocytes density provides an indicator of tumor recurrence beyond the AJCC/UICC-TNM staging, we propose a novel classification based on the evaluation of the host immune reaction (Im classification).
Immune scoring in early stage colorectal cancers
As stated above, in early-stage CRC patients with no detectable lymph node or distant metastasis, surgery is the state of the art. However, a significant number of patients (20–25%) will recur indicating that they already had occult metastasis at the time of surgery. There is presently no marker to identify the group of relapsing patients that might benefit of adjuvant therapy. We thus undertook a large study on 602 early-stage CRC patients (stages I–II) to assess the importance of the immune pattern from the surgically removed tumor in predicting recurrence and overall survival.
Based on our previous observations, we chose to classify the patients based on the immune score (Im0 to Im4) that quantifies the intratumoral CD45RO + and CD8+ T cells. Forty-two percent of the patients presented a high infiltration of CD8+ and CD45RO + cells in CT and IM (Im4), whereas 4% had a low infiltration of these cells in both regions (Im0). Univariate analysis showed significant differences in DFS, DSS, and OS among immune score based patient groups. Im4 patients were at low risk, with 5-year DFS and OS rates of 95.2% and 86.2%, respectively. In contrast, Im0 were at high risk, with 5-year DFS and OS rates of 25% and 27.5%, respectively. Im1 and Im2 patients experienced a similar bad postoperative outcome. Indeed, the cumulative DFS and OS rates of the Im1 and Im2 patients were 56.4% and 61.6%, respectively [16].
These data indicate that a stratification of the patients based on the intratumoral CD8+ and CD45RO + cell density could be of interest in clinical practice. In multivariate analysis, the immune score and bowel perforation remained the only independent prognostic factors, whereas T stage was no longer significant. Of note, perforation represented only 3.4% of the patients, and this proportion tends to decrease with earlier detection of CRC in recent years. The immune score allowed the classification of patients into groups with distinct clinical outcome [16]. Thus, we propose to include in clinical practice the strong and reproducible intratumoral immune score.
Immune scoring and modulation of the immune reaction
T helper cells
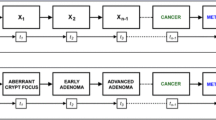
We analyzed the functional immune coordination and the cytotoxic T cell markers in relation to T helper subpopulations (Th1, Th2, Th17, and Treg) [17–19]. Figure 1 summarizes the four major groups of patients according to immune status and outcome. Unsupervised hierarchical clustering of a correlation matrix revealed functional clusters of genes associated with Th17, Th2, Th1, Treg, and cytotoxicity. Patients with high expression of the Th17 cluster had a poor prognosis, whereas patients with high expression of the Th1 cluster had a prolonged disease-free survival. In contrast, no prediction of the prognosis was associated with Th2 cluster. The combined analysis of cytotoxic and Th17 clusters gave a better discrimination for relapse. These results were confirmed by in situ analysis of the immune density from CT and IM [18].
General scheme of immune control of metastatic spread and clinical outcome. Four major groups of patients were found according to immune status and relapse. Optimal immune response is characterized by high-immune T cell infiltration, immune coordination, low VEGF expression, and low Th17 density. Altered immune reaction is either, (1) high-immune T cell infiltration and absence of immune coordination or increased VEGF expression, (2) heterogeneous-immune T cell infiltration between CT and IM regions, and high or heterogeneous Th17 densities, and (3) low-immune T cell infiltration and absence of immune coordination
Patients with high density of IL17+ cells had a poor prognosis, whereas patients with high density of CD8+ cells had a prolonged DFS. The combination of these two markers also gave a better discrimination of patients. In particular, patients with heterogeneous densities of CD8+ cells in CT and IM having an intermediate outcome could be discriminated in good or bad survivor depending on the densities of the IL17+ cells [18]. As previously reported [20], we found that an improved survival associated with a high density of tumor-infiltrating FoxP3+ cells suggesting no major immunosuppressive role of Treg cells in CRC.
T regulatory cells and prognosis
It was reported an analysis of T cell infiltrates in large cohorts of stage II and III CRC patients [20]. Similar to our findings, they confirmed a low density of CD45RO + cells in patients with early signs of metastasis. They found also that CD45RO + and CD8+ T cells correlate with microsatellite instability in the tumor. High densities of intratumoral CD45RO+, CD8+, and strikingly FoxP3+ cells correlate with a good prognosis.
The question of the prognostic value of regulatory T cells in human cancers appears indeed to be a complex issue. Curiel et al. [21] reported that the presence of high density of CD3+ CD4+ CD25+ FoxP3+ cells in malignant ascites of ovarian carcinoma correlated with advanced tumor staging and reduced survival. Those results were confirmed in other solid tumors, such as pancreatic ductal adenocarcinoma [22] or hepatocarcinoma [23]. Those findings gained a large interest since they supported the appealing hypothesis that the induction of Treg could be a major escape mechanism for human tumors. In this light, Treg could represent not only a prognostic marker but, even more importantly, a target for immunotherapy.
However, in follicular lymphoma and Hodgkin's lymphoma [24, 25] high density of intratumoral Treg was shown to correlate with good prognosis. FoxP3+ T cell infiltration in head and neck cancer was associated with a better loco-regional control of the tumor. Multivariate analysis showed that the significant prognostic factors related to loco-regional control were the T stage and the intratumoral Treg infiltration [26]. In CRC, high densities of FoxP3+ T cells were associated with microsatellite instability [27, 28], feature usually associated with favorable prognosis. We found no association between the expression of FoxP3, CTLA4, GITR, IL10, and TGFb and the presence of lymph node or distant metastasis. In ovarian carcinoma, the absolute number of FoxP3+ lymphocytes infiltrating the tumor epithelium was an independent prognostic factor for longer DSS in advanced stage and metastatic patients [29]. The issue is therefore still open and needs more precise analysis of the relative proportion of Treg versus helper and cytotoxic T cells, their spatial distribution in tumor, invaded lymph nodes and blood, of CD4 or CD8 FoxP3+ subpopulations [30], as well as their functionality [31]. Even more, the T cell plasticity where Treg can lose FoxP3 expression and change their phenotype [32], and reversely, FoxP3-T cells can acquire FoxP3, without becoming regulatory [33], adds complexity to these analysis.
Immune scoring in other cancer types
Is the immune score specific to CRC, or it could be applied to other cancer types as well? There have been many reports showing that intratumoral CD8+ T cells are independent predictors of survival or disease outcome in a variety of malignancies, either alone or in conjunction with additional immune markers. High density of lymphocytes, especially T cells, has been reported of good prognosis in melanoma, breast cancer, ovarian cancer, non-Hodgkin's lymphoma, head and neck cancer, non-small cell lung cancer (NSCLC), esophagus cancer, urothelial carcinoma, endometrial cancer, malignant pleural mesothelioma [34–40]. This supports the idea that the immune contexture, particularly elaborated in CRC [12], could be a general phenomenon.
One of the most studied human malignancies is CRC. The first reports on a beneficial effect of lymphocytic infiltration in CRC have been published 30–20 years ago [41–44]. They were confirmed recently by studies underlining the prominent role of memory T cells [14] and CD8+ T cells [45] in predicting disease-free and overall survival.
It is interesting to note that it does not only concern various organs (breast, colon, lung, head and neck, kidney, bladder, ovary, prostate…), but also various cancer cell types (adenocarcinoma, squamous cell carcinoma, large cell cancer, melanoma…). It concerns tumors considered as immunogenic in which the success of active immunotherapies with IL2, IFN, or TIL has been documented [46], such as melanoma or renal cell cancer as well as tumors in which there is, so far, no success of these approaches which leaves open the search for alternative novel immunotherapies.
This diversity in type of malignancy and stage of the disease suggest that immune score may be a useful addition to the evaluation of many tumor types. Whether a universal consensus immune score can be generated is unknown; however, there are many common features in the host immune response against many cancer types. Considering the probable universal character of the immune control of tumors, it is essential to stop ignoring it as a prognostic factor [8] and to introduce the immune score as a marker to classify cancers [13, 16]. This marker has a dual advantage: firstly, it appears to be the strongest prognostic factor for disease-free and overall survival particularly in early-stage cancers and secondly, it provides a tool or a target for novel therapeutic approaches. A better understanding of the interplay between the immune contexture, the inflammatory context, the vascularization in the microenvironment and the tumor cells is also necessary. Where an efficient immune reaction is generated and ultimately towards what antigens is directed are major questions still to answer. Better understanding of these elements and interactions should lead to the development of novel, more efficient therapeutic strategies.
References
Broussard EK, Disis ML (2011) TNM staging in colorectal cancer: T is for T cell and M is for memory. J Clin Oncol 29:601–603
Locker GY, Hamilton S, Harris J, Jessup JM, Kemeny N et al (2006) ASCO 2006 update of recommendations for the use of tumor markers in gastrointestinal cancer. J Clin Oncol 24:5313–5327
Sobin L, Wittekind C (2002) TNM classification of malignant tumors, 6th edn. Wiley-Liss, New York
Weitz J, Koch M, Debus J, Hohler T, Galle PR et al (2005) Colorectal cancer. Lancet 365:153–165
Kumar T, Patel N, Talwar A (2010) Spontaneous regression of thoracic malignancies. Respir Med 104:1543–1550
Bir AS, Fora AA, Levea C, Fakih MG (2009) Spontaneous regression of colorectal cancer metastatic to retroperitoneal lymph nodes. Anticancer Res 29:465–468
Kalialis LV, Drzewiecki KT, Klyver H (2009) Spontaneous regression of metastases from melanoma: review of the literature. Melanoma Res 19:275–282
Bindea G, Mlecnik B, Fridman WH, Pages F, Galon J (2010) Natural immunity to cancer in humans. Curr Opin Immunol 22:215–222
Pages F, Galon J, Fridman WH (2008) The essential role of the in situ immune reaction in human colorectal cancer. J Leukoc Biol 84:981–987
Pages F, Galon J, Dieu-Nosjean MC, Tartour E, Sautes-Fridman C et al (2010) Immune infiltration in human tumors: a prognostic factor that should not be ignored. Oncogene 29:1093–1102
Galon J, Costes A, Sanchez-Cabo F, Kirilovsky A, Mlecnik B et al (2006) Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 313:1960–1964
Galon J, Fridman WH, Pages F (2007) The adaptive immunologic microenvironment in colorectal cancer: a novel perspective. Cancer Res 67:1883–1886
Mlecnik B, Tosolini M, Kirilovsky A, Berger A, Bindea G et al (2011) Histopathologic-based prognostic factors of colorectal cancers are associated with the state of the local immune reaction. J Clin Oncol 29:610–618
Pages F, Berger A, Camus M, Sanchez-Cabo F, Costes A et al (2005) Effector memory T cells, early metastasis, and survival in colorectal cancer. N Engl J Med 353:2654–2666
Xiang R, Lode HN, Gillies SD, Reisfeld RA (1999) T cell memory against colon carcinoma is long-lived in the absence of antigen. J Immunol 163:3676–3683
Pages F, Kirilovsky A, Mlecnik B, Asslaber M, Tosolini M et al (2009) In situ cytotoxic and memory T cells predict outcome in patients with early-stage colorectal cancer. J Clin Oncol 27:5944–5951
Camus M, Tosolini M, Mlecnik B, Pages F, Kirilovsky A et al (2009) Coordination of intratumoral immune reaction and human colorectal cancer recurrence. Cancer Res 69:2685–2693
Tosolini M, Kirilovsky A, Mlecnik B, Fredriksen T, Mauger S et al (2011) Clinical impact of different classes of infiltrating T cytotoxic and helper cells (Th1, Th2, Treg, Th17) in patients with colorectal cancer. Cancer Res 71:1263–1271
Mlecnik B, Tosolini M, Charoentong P, Kirilovsky A, Bindea G et al (2010) Biomolecular network reconstruction identifies T-cell homing factors associated with survival in colorectal cancer. Gastroenterology 138:1429–1440
Salama P, Phillips M, Grieu F, Morris M, Zeps N et al (2009) Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J Clin Oncol 27:186–192
Curiel TJ, Coukos G, Zou L, Alvarez X, Cheng P et al (2004) Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival. Nat Med 10:942–949
Hiraoka N, Onozato K, Kosuge T, Hirohashi S (2006) Prevalence of FOXP3+ regulatory T cells increases during the progression of pancreatic ductal adenocarcinoma and its premalignant lesions. Clin Cancer Res 12:5423–5434
Fu J, Xu D, Liu Z, Shi M, Zhao P et al (2007) Increased regulatory T cells correlate with CD8 T-cell impairment and poor survival in hepatocellular carcinoma patients. Gastroenterology 132:2328–2339
Carreras J, Lopez-Guillermo A, Fox BC, Colomo L, Martinez A et al (2006) High numbers of tumor-infiltrating FOXP3-positive regulatory T cells are associated with improved overall survival in follicular lymphoma. Blood 108:2957–2964
Tzankov A, Meier C, Hirschmann P, Went P, Pileri SA et al (2008) Correlation of high numbers of intratumoral FOXP3+ regulatory T cells with improved survival in germinal center-like diffuse large B-cell lymphoma, follicular lymphoma and classical Hodgkin's lymphoma. Haematologica 93:193–200
Badoual C, Hans S, Rodriguez J, Peyrard S, Klein C et al (2006) Prognostic value of tumor-infiltrating CD4+ T-cell subpopulations in head and neck cancers. Clin Cancer Res 12:465–472
Le Gouvello S, Bastuji-Garin S, Aloulou N, Mansour H, Chaumette MT et al (2008) High prevalence of Foxp3 and IL17 in MMR-proficient colorectal carcinomas. Gut 57:772–779
Michel S, Benner A, Tariverdian M, Wentzensen N, Hoefler P et al (2008) High density of FOXP3-positive T cells infiltrating colorectal cancers with microsatellite instability. Br J Cancer 99:1867–1873
Leffers N, Gooden MJ, de Jong RA, Hoogeboom BN, ten Hoor KA et al (2009) Prognostic significance of tumor-infiltrating T-lymphocytes in primary and metastatic lesions of advanced stage ovarian cancer. Cancer Immunol Immunother 58:449–459
Chaput N, Louafi S, Bardier A, Charlotte F, Vaillant JC et al (2009) Identification of CD8 + CD25 + Foxp3+ suppressive T cells in colorectal cancer tissue. Gut 58:520–529
Badoual C, Hans S, Fridman WH, Brasnu D, Erdman S et al (2009) Revisiting the prognostic value of regulatory T cells in patients with cancer. J Clin Oncol 27:e5–e6
Komatsu N, Mariotti-Ferrandiz ME, Wang Y, Malissen B, Waldmann H et al (2009) Heterogeneity of natural Foxp3+ T cells: a committed regulatory T-cell lineage and an uncommitted minor population retaining plasticity. Proc Natl Acad Sci USA 106:1903–1908
Hoffmann P, Boeld TJ, Eder R, Huehn J, Floess S et al (2009) Loss of FOXP3 expression in natural human CD4 + CD25+ regulatory T cells upon repetitive in vitro stimulation. Eur J Immunol 39:1088–1097
Anraku M, Cunningham KS, Yun Z, Tsao MS, Zhang L et al (2008) Impact of tumor-infiltrating T cells on survival in patients with malignant pleural mesothelioma. J Thorac Cardiovasc Surg 135:823–829
Clemente CG, Mihm MC Jr, Bufalino R, Zurrida S, Collini P et al (1996) Prognostic value of tumor infiltrating lymphocytes in the vertical growth phase of primary cutaneous melanoma. Cancer 77:1303–1310
de Jong RA, Leffers N, Boezen HM, ten Hoor KA, van der Zee AG et al (2009) Presence of tumor-infiltrating lymphocytes is an independent prognostic factor in type I and II endometrial cancer. Gynecol Oncol 114:105–110
Dunn GP, Old LJ, Schreiber RD (2004) The three Es of cancer immunoediting. Annu Rev Immunol 22:329–360
Schumacher K, Haensch W, Roefzaad C, Schlag PM (2001) Prognostic significance of activated CD8(+) T cell infiltrations within esophageal carcinomas. Cancer Res 61:3932–3936
Zhang L, Conejo-Garcia JR, Katsaros D, Gimotty PA, Massobrio M et al (2003) Intratumoral T cells, recurrence, and survival in epithelial ovarian cancer. N Engl J Med 348:203–213
Dieu-Nosjean MC, Antoine M, Danel C, Heudes D, Wislez M et al (2008) Long-term survival for patients with non-small-cell lung cancer with intratumoral lymphoid structures. J Clin Oncol 26:4410–4417
Halvorsen TB, Seim E (1989) Association between invasiveness, inflammatory reaction, desmoplasia and survival in colorectal cancer. J Clin Pathol 42:162–166
House AK, Watt AG (1979) Survival and the immune response in patients with carcinoma of the colorectum. Gut 20:868–874
Jass JR (1986) Lymphocytic infiltration and survival in rectal cancer. J Clin Pathol 39:585–589
Svennevig JL, Lunde OC, Holter J, Bjorgsvik D (1984) Lymphoid infiltration and prognosis in colorectal carcinoma. Br J Cancer 49:375–377
Naito Y, Saito K, Shiiba K, Ohuchi A, Saigenji K et al (1998) CD8+ T cells infiltrated within cancer cell nests as a prognostic factor in human colorectal cancer. Cancer Res 58:3491–3494
Kirkwood JM, Tarhini AA (2009) Biomarkers of therapeutic response in melanoma and renal cell carcinoma: potential inroads to improved immunotherapy. J Clin Oncol 27:2583–2585
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is published as part of the Special Issue on Prognostic Impact of Anti-Cancer Immune Responses [33:5].
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Bindea, G., Mlecnik, B., Fridman, WH. et al. The prognostic impact of anti-cancer immune response: a novel classification of cancer patients. Semin Immunopathol 33, 335–340 (2011). https://doi.org/10.1007/s00281-011-0264-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-011-0264-x