Abstract
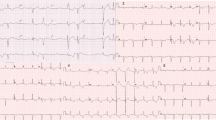
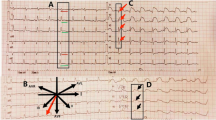
We report the case of a female patient with congenital complete atrioventricular block who developed torsade de pointes (TdP) in the course of takotsubo cardiomyopathy. On the basis of this case, we show that the electrocardiographic evolutionary changes with QT interval prolongation (in the course of takotsubo cardiomyopathy) may be a TdP threatening period in patients with underlying predispositions. After reviewing the literature, we also present the electrocardiographic similarities between takotsubo cardiomyopathy and other acute heart diseases associated with a large amount of stunned myocardium, i.e., other stress-related cardiomyopathies (e.g., those associated with subarachnoid hemorrhage, pheochromocytoma, or severe illnesses) as well as a reperfused myocardial infarction. QT interval prolongation is a common feature in the subacute phase of these entities; however, excessive QT prolongation may be a sign of predisposition to TdP. In such instances, measures should be taken to monitor cardiac rhythm closely and to prevent or treat TdP appropriately. Taking into account the risk of TdP, it is reasonable to consider takotsubo cardiomyopathy as a potential cause of acquired long QT syndrome.
Zusammenfassung
Berichtet wird über den Fall einer Patientin mit kongenitalem atrioventrikulärem (AV-)Block, bei der eine Torsade de pointes (TdP) im Rahmen einer Takotsubo-Kardiomyopathie auftrat. Auf der Grundlage diese Falls wird gezeigt, dass ein Elektrokardiographie(EKG)-Verlauf mit QT-Intervall-Verlängerung (im Rahmen der Takotsubo-Kardiomyopathie) eine Phase erhöhten Risikos für eine TdP bei Patienten mit entsprechender Prädisposition darstellen kann. Nach einer Übersicht über die Literatur werden auch Ähnlichkeiten im EKG zwischen Takotsubo-Kardiomyopathie und anderen akuten Herzerkrankungen beschrieben, die mit einem hohen Anteil reperfundierten, hypokinetischen Myokards („stunned myocardium“) einhergehen, z. B. andere stressbedingte Kardiomyopathien (wie bei Subarachnoidalblutung, Phäochromozytom oder schweren Erkrankungen) oder ein reperfundierter Herzinfarkt. Die QT-Intervall-Verlängerung tritt häufig in der subakuten Phase dieser Erkrankungen auf, eine ausgeprägte QT-Verlängerung kann jedoch Zeichen der Prädisposition zur TdP sein. In solchen Fällen sollten Maßnahmen zur engmaschigen Überwachung des Herzrhythmus und zur Vorbeugung oder angemessenen Behandlung einer TdP ergriffen werden. Angesichts des Risikos einer TdP sollte die Takotsubo-Kardiomyopathie als potenzielle Ursache eines erworbenen langen QT-Syndroms angesehen werden.




Similar content being viewed by others
References
Dote K, Sato H, Tateishi H et al (1991) Myocardial stunning due to simultaneous multivessel coronary spasms: a review of 5 cases. J Cardiol 21:203–214
Tsuchihashi K, Ueshima K, Uchida T et al (2001) Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction: Angina Pectoris-Myocardial Infarction Investigations in Japan. J Am Coll Cardiol 38:11–18
Sacha J, Maselko J, Wester A et al (2007) Left ventricular apical rupture caused by takotsubo cardiomyopathy—comprehensive pathological heart investigation. Circ J 71:982–985
Raddino R, Pedrinazzi P, Zanini G et al (2008) Out-of-hospital cardiac arrest caused by transient left ventricular apical ballooning syndrome. Int J Cardiol 128:e31–e33
Lee PH, Song JK, Sun BJ et al (2010) Outcomes of patients with stress-induced cardiomyopathy diagnosed by echocardiography in a tertiary referral hospital. J Am Soc Echocardiogr 23:766–771
Kurisu S, Inoue I, Kawagoe T et al (2004) Time course of electrocardiographic changes in patients with tako-tsubo syndrome comparison with acute myocardial infarction with minimal enzymatic release. Circ J 68:77–81
Sommargren CE (2002) Electrocardiographic abnormalities in patients with subarachnoid hemorrhage. Am J Crit Care 11:48–56
Agarwal V, Kant G, Hans N, Messerli FH (2011) Takotsubo-like cardiomyopathy in pheochromocytoma. Int J Cardiol 153:241–248
Sharkey SW, Shear W, Hodges M, Herzog CA (1998) Reversible myocardial contraction abnormalities in patients with an acute noncardiac ilness. Chest 114:98–105
Park JH, Kang SJ, Song JK et al (2005) Left ventricular apical ballooning due to severe physical stress in patients admitted to the medical ICU. Chest 128:296–302
Bybee KA, Prasad A (2008) Stress-related cardiomyopathy syndromes. Circulation 118:397–409
Sacha J (2012) Letter by Sacha regarding article, “Clinical and genetic determinants of torsade de pointes risk”. Circulation 126:e309
Ghosh S, Apte P, Maroz N et al (2009) Takotsubo cardiomyopathy as a potential cause of long QT syndrome and torsades de pointes. Int J Cardiol 136:225–227
Topilski I, Rogowski O, Rosso R et al (2007) The morphology of the QT interval predicts torsade de pointes during acquired bradyarrhythmias. J Am Coll Cardiol 49:320–328
Nakajima T, Kagoshima T, Fujimoto S et al (1996) The deeper the negativity of the T waves recorded, the greater is the effectiveness of reperfusion of the myocardium. Cardiology 87:91–97
Abraham J, Mudd JO, Kapur N et al (2009) Stress cardiomyopathy after intravenous administration of catecholamines and beta-receptor agonists. J Am Coll Cardiol 53:1320–1325
Wittstein IS, Thiemann DR, Lima JA et al (2005) Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med 352:539–548
Janse MJ (2004) Historical vignette: the long QT syndrome and the sympathetic nerves. Heart Rhythm 1:284
Priori SG, Corr PB (1990) Mechanisms underlying early and delayed afterdepolarizations induced by catecholamines. Am J Physiol 258:H1796–1805
Behr ER, Mahida S (2009) Takotsubo cardiomyopathy and the long-QT syndrome: an insult to repolarization reserve. Europace 11:697–700
Jensen G, Sigurd B, Sandoe E (1975) Adams-Stokes seizures due to ventricular tachydysrhythmias in patients with heart block: prevalence and problems of management. Chest 67:43–48
Dib C, Prasad A, Friedman PA et al (2008) Malignant arrhythmia in apical ballooning syndrome: risk factors and outcomes. Indian Pacing Electrophysiol J 8:182–192
Kirchhof P, Franz MR, Bardai A, Wilde AM (2009) Giant T-U waves precede torsades de pointes in long QT syndrome: a systematic electrocardiographic analysis in patients with acquired and congenital QT prolongation. J Am Coll Cardiol 54:143–149
Kawasaki R, Machado C, Reinoehl J et al (1995) Increased propensity of women to develop torsades de pointes during complete heart block. J Cardiovasc Electrophysiol 6:1032–1038
Roden DM (2006) Long QT syndrome: reduced repolarization reserve and the genetic link. J Intern Med 259:59–69
Samuelov-Kinori L, Kinori M, Kogan Y et al (2009) Takotsubo cardiomyopathy and QT interval prolongation: who are the patients at risk for torsades de pointes? J Electrocardiol 42:353–357.e1
Madias C, Fitzgibbons TP, Alsheikh-Ali AA et al (2011) Acquired long QT syndrome from stress cardiomyopathy is associated with ventricular arrhythmias and torsades de pointes. Heart Rhythm 8:555–561
Halkin A, Roth A, Lurie I et al (2001) Pause-dependent torsade de pointes following acute myocardial infarction: a variant of the acquired long QT syndrome. J Am Coll Cardiol 38:1168–1174
Bonnemeier H, Ortak J, Bode F et al (2006) Modulation of ventricular repolarization in patients with transient left ventricular apical ballooning: a case control study. J Cardiovasc Electrophysiol 17:1340–1347
Conflict of interest
On behalf of all authors, the corresponding author states that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sacha, J., Wester, A., Hordynski, G. et al. QT interval prolongation during ECG evolution in takotsubo cardiomyopathy poses a threat of torsade de pointes to predisposed patients. Herz 38, 790–795 (2013). https://doi.org/10.1007/s00059-013-3756-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-013-3756-8