Abstract
Background
Complete heart block is considered a unique and rare complication of Takotsubo cardiomyopathy, an otherwise self-resolving disease. When this occurs, there is a double clinical dilemma: first to find out which triggered the other and second, to decide whether or not to implant a permanent pacemaker.
Case presentation
We present a case of a 77 years-old female patient, with previous medical history of arterial hypertension, diabetes mellitus, dyslipidemia and bifascicular block known since 2013. She came to the emergency department after recurrent syncopal episodes. At admission a complete heart block was diagnosed, and it was implanted a single chamber temporary pacemaker. The patient remained in disproportional acute decompensated heart failure despite pacemaker implantation. She denied chest pain although referring an episode of self-limiting chest pain 2 days before, after an argument with the family. Blood analysis showed an important rise in NTproBNP and troponin levels. Transthoracic echocardiogram showed a dilated left ventricle with akinesia of apical and mid segments, hyperkinesia of basal segments and severely depressed left ventricle ejection fraction. Coronary angiography showed no significant lesions and the diagnosis of Takotsubo cardiomyopathy was suspected. During the following days, she recovered her own intrinsic rhythm. Electrocardiogram evolved with deep T-wave inversion and prolonged QT interval and transthoracic echocardiogram showed resolution of the previous alterations. Despite complete reversion of rhythm alteration, it was decided to implant a permanent pacemaker.
Conclusions
We describe a rare, life-threatening and often underdiagnosed complication of the stress cardiomyopathy. Furthermore, we performed a literature revision of this rare complication and discussed the therapeutic challenge encountered in such patients.
Similar content being viewed by others
Background
Takotsubo cardiomyopathy (TC) is an increasingly diagnosed clinical entity that usually mimics an acute coronary syndrome [1,2,3]. The diagnosis requires the presence of temporary left ventricular apical ballooning induced by stress, in the absence of significant coronary heart stenosis [1,2,3]. Although the overall prognosis is often favorable, in rarer cases, it can be associated with life-threatening complications, such as cardiac arrhythmias [2]. We present a case of a patient with a complete heart block (CHB) that was after all a TC.
Clinical case presentation
The authors present a 77-year-old woman with previous medical history of arterial hypertension, diabetes mellitus, dyslipidemia, bifascicular block known since 2013 and depression, medicated accordingly.
She came to the emergency department (ED) due to multiple episodes of syncope in the last 24 h. No symptoms including chest pain were reported.
During clinical observation she was prostrated, hypotensive (95/77 mmHg) and severely bradycardic (20–30 bpm). The skin showed signs of poor perfusion. Cardiac and pulmonary auscultation were unremarkable, and there was no peripheral oedema.
Electrocardiogram (ECG) showed a CHB with broad QRS complexes and T wave inversion in the inferior leads. Blood gas analysis revealed a metabolic acidosis and hyperlactacidemia (pH: 7.30, pO2 89 mmol/L, pCO2: 35 mmol/L, HCO3: 17.1 mmol/L, sO2: 96.9% and lactates: 4.6 mmol/L). Initial blood analysis revealed worsening renal function (creatinine level 1.5 mg/dL) with hyperkalaemia (6.1 mmol/L), hepatic enzyme rise (AST 319 UI/L, ALT 324 UI/L) and a mild elevation of high sensitivity T troponin level (26 ng/L).
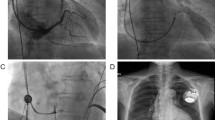
The diagnosis of non-pharmacological CHB was made and she started isoproterenol perfusion, with no response. A single chamber temporary pacemaker (PM) was implanted.
Besides the improvement in low-output state and after potassium correction, she remained in CHB supported by the temporary pacemaker. About 24-h later, she had an episode of acute dyspnoea and peripheral desaturation. The patient denied having chest pain, although she reported an episode of self-limited retrosternal chest pain 2 days before de admission, after a severe argument with her grandchildren (Fig. 1).
ECG evolution during hospitalization—image 1 showing CHB with broad QRS complexes and T wave inversion in the inferior leads; image 2 and 3 showing sinus rhythm with left anterior fascicular block combined with complete right bundle branch block, deep T waves inversion from V1 to V6 and in the inferior leads and a prolonged QTc interval (500 ms). Image 3 after implanting dual chamber permanent pacemaker. Image 5 shows improvement in electrocardiographic changes, with QTc normalization
A transthoracic echocardiogram (TTE) showed a dilated left ventricle (LV) with akinesia of apical and mid segments, hyperkinesia of basal segments and severely depressed left ventricle ejection fraction (LVEF) (Additional file 1: Video 1). There was a significant rise in troponin and NT-proBNP levels (670 ng/L and 19 260 pg/mL, respectively). The coronary angiography showed no significant lesions, and the diagnosis of TC was suspected. During the following days, the patient presented clinical improvement and recovered her own intrinsic rhythm. The ECG evolved with deep T wave inversion and a prolonged QTc interval (500 ms) (Fig. 1). TTE revaluation showed improvement in LV wall motion abnormalities and LVEF (Additional file 2: Video 2). The diagnosis of TC complicated with CHB was considered the most probable diagnosis (94.8% chance), according to the interTAK diagnostic score of 78.
Taking into account the presence of bifascicular block in the pre-hospitalization ECG, it was decided to implant a double chamber permanent pacemaker and the patient was discharged one day after.
Six months later, the pacemaker review appointment confirmed a low percentage of ventricular and atrial pacing (9% and 30%, respectively).
Discussion
TC was firstly described by Dote et al. in Japan, during the year of 1991. Its name was inspired on typical TTE findings: the presence of LV apical ballooning, which resembles a Japanese octopus pot [3, 6, 7]. This non-ischemic cardiomyopathy is characterized by a reversible LV systolic dysfunction, usually triggered by a major physical or emotional stress [1–3, 6,7]. It is estimated that 90% of TC occur in post-menopausal women with more than 60 years old, as it was the case of our patient [1,2,3]. Although the pathophysiology is still not well understood, this predominance of the age and gender seems to be related to oestrogen-induced glucocorticoid and catecholamine response to stress [2, 6, 7].
Usually, these patients present with symptoms and ECG/TTE findings than resemble an ongoing acute coronary syndrome [1,2,3]. However, in some cases, rhythm disturbances may be present, representing confounding factor. Within these, atrial fibrillation is the most common one (5–15% of the cases), followed by ventricular arrythmias [1, 4]. Bradycardia due to advanced atrioventricular (AV) block occurs rarely, being described in only 5% of the cases [5]. In these cases, clinical dilemma is twofold: first to find out which triggered the other and second to decide whether or not to implant cardiac devices [9].
Regarding the first part, it is always extremely difficult to determine for certain which one was the cause and the consequence. However, and looking retrospectively, our patient had almost all the hallmark features of a CHB complicating a TC: the patient was considered to have high risk to develop TC (age, post-menopausal and depression), had a previous episode of chest pain triggered by emotional stress, the ECG at admission had already T-wave inversion which could be an indirect signal, there was resolution of the CHB concomitant with the improvement of LVEF and the patient had an InterTAK diagnostic score of 78.
In 2017, J R Ghadri et al. proposed a new clinical score (InterTAK diagnostic Score), which could be easily acquired in the ED, in order to facilitate the diagnosis of this syndrome [8]. This clinical score included 7 variables (female gender, emotional trigger, physical trigger, absence of ST-segment depression, psychiatric disorders, neurological disorders and QTc prolongation), each one corresponding to a score, that added together would give a certain probability of having the disease [8]. In our case, the patient had 5 out of 7 criteria, which gave her a very high probability of having this syndrome (94.6%).
The performance of an early TTE (at admission) and a detailed medical history may have avoided a delay in diagnosis.
When CHB complicates TC, it can be temporary, reversing after a few days, or it can be permanent, leading to pacemaker implantation. The specific damaged caused in the AV conduction system and the differences between temporary or permanent AV block are still not well understood.
The decision to implant a permanent pacemaker in patients who develop a TC-related CHB is still a matter of debate, not only because the timeline between the resolution of segmental changes/LVEF and the AV block is not well defined, but also because, in some cases, the improvement may not even be concordant [2]. According to literature, there are 24 reported cases of AV block complicating TC, of which only 4 did not implanted a cardiac device [7,9]. The main reason for not implanting a pacemaker in these cases was the complete resolution of AV block during hospitalization [9]. Among patients who underwent implantation of cardiac device, only 2 had documented remission of the AV block [9].
According to our understanding, this case would be the fifth clinical case of a transient AV conduction disorder in a patient with TC reported in the literature, and the first being submitted to pacemaker implantation. The decision of implant a dual chamber pacemaker in this patient was challenging and difficult, especially due to the lack of documented evidence in the literature. However, considering that this was a patient with a bifascicular block with high probability of disease progression, it was decided to implant it.
Conclusion
This clinical case documents one of the rarest and most potentially fatal complications of a syndrome considered by many as benign. It also highlights the importance of a detailed clinical history combined with echocardiography in the diagnosis of TC which can be decisive in the initial approach to the patient. Further studies and guidelines are necessary to define the best management of patients with fatal arrythmias and AV block in the setting of TC.
Availability of data and materials
Not applicable.
Abbreviations
- AV:
-
Atrioventricular
- CHB:
-
Complete heart block
- ECG:
-
Electrocardiogram
- ED:
-
Emergency department
- LV:
-
Left ventricle
- LVEF:
-
Left ventricle ejection fraction
- TC:
-
Takotsubo cardiomyopathy
- TTE:
-
Transthoracic echocardiogram
References
Lyon AR, Bossone E, Schneider B, et al. Current state of knowledge on takotsubo syndrome: a position statement from the Taskforce on Takotsubo syndrome of the Heart failure association of the European Society of Cardiology. Eur J Heart Fail. 2015. https://doi.org/10.1002/ejhf.424.
Inayat F, Virk H, Ullah W, Riaz I. Takotsubo cardiomyopathy-related complete heart block and torsade de pointes. BMJ Case Rep. 2017. https://doi.org/10.1136/bcr-2016-218017.
Afzal A, Watson J, Choi J, Schussler J, Assar M. Takostubo cardiomyopathy in the setting of complete heart blocks. Bayl Univ Med Cent. 2018. https://doi.org/10.1080/08998280.2018.1499314.
Schneider B, Athanasiadis A, Schwab J, et al. Complications in the clinical course of tako-tsubo cardiomyopathy. Int J Cardiol. 2014. https://doi.org/10.1016/j.ijcard.2014.07.002.
Inoue M, Kanaya H, Matsubara T, Uno Y, Yasuda T, Miwa K. Complete atrioventricular block associated with Takotsubo cardiomyopathy. Circ J. 2008. https://doi.org/10.1253/circj.CJ-08-0219.
Saadatifar H, Dehdar F, Saadatifar S, Farahani M. Takotsubo cardiomyopathy with significant coronary artery stenosis and atrioventricular conduction block: a rare case report with 3 year follow-up. Res Cardiovasc Med. 2016. https://doi.org/10.5812/cardiovascmed.27839.
Sugiura T, Dobi Y, Yamashita S, et al. Midventricular ballooning Takotsubo cardiomyopathy complicated by transient complete atrioventricular block. Intern Med. 2013. https://doi.org/10.2169/internalmedicine.52.0721.
Ghadri JR, Cammann V, Jurisic S, et al. A novel clinical score (InterTAK Diagnostic Score) to differentiate takotsubo syndrome from acute coronary syndrome: results from the International Takotsubo Registry. Eur J Heart Fail. 2016. https://doi.org/10.1002/ejhf.683.
McGee MJ, Yu W, McCarthy J, Barlow M, Hackworthy R. Complete heart block complicating takotsubo syndrome: a case report and literature review. Case Rep Cardiol. 2020. https://doi.org/10.1155/2020/7614836.
Acknowledgements
Not applicable.
Funding
There are no sources of funding to be reported.
Author information
Authors and Affiliations
Contributions
AB: writing and revision. JS: writing. ACG: writing and revision. OS: Revision. RM: Revision. SA: Revision. LB: Revision. HP: Revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
The patient’s consent for publication was obtained.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Video 1. A transthoracic echocardiogram (TTE) showed a dilated left ventricle (LV) with akinesia of apical and mid segments, hyperkinesia of basal segments and severely depressed left ventricle ejection fraction (LVEF).
Additional file 2: Video 2. TTE revaluation showed improvement in LV wall motion abnormalities and LVEF.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Briosa, A., Santos, J., Gomes, A.C. et al. “Blocked broken heart syndrome”: an unusual case of a complete atrioventricular block complicating a Takotsubo cardiomyopathy. Int J Arrhythm 23, 18 (2022). https://doi.org/10.1186/s42444-022-00069-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42444-022-00069-9