Abstract
Background
Much effort has been made over the last two decades to educate and train healthcare professionals working on antimicrobial resistance in French hospitals. However, little has been done in France to assess perceptions, attitudes and knowledge regarding multidrug resistant organisms (MDROs) and, more globally, these have never been evaluated in a large-scale population of medical and non-medical healthcare workers (HCWs). Our aim was to explore awareness among HCWs by evaluating their knowledge of MDROs and the associated control measures, by comparing perceptions between professional categories and by studying the impact of training and health beliefs.
Methods
A multicentre cross-sectional study was conducted in 58 randomly selected French healthcare facilities with questionnaires including professional and demographic characteristics, and knowledge and perception of MDRO transmission and control. A knowledge score was calculated and used in a logistic regression analysis to identify factors associated with higher knowledge of MDROs, and the association between knowledge and perception.
Results
Between June 2014 and March 2016, 8716/11,753 (participation rate, 74%) questionnaires were completed. The mean knowledge score was 4.7/8 (SD: 1.3) and 3.6/8 (SD: 1.4) in medical and non-medical HCWs, respectively. Five variables were positively associated with higher knowledge: working in a university hospital (adjusted odds ratio, 1.41, 95% CI 1.16–1.70); age classes 26–35 years (1.43, 1.23–1.6) and 36–45 years (1.19, 1.01–1.40); medical professional status (3.7, 3.09–4.44), working in an intensive care unit (1.28, 1.06–1.55), and having been trained on control of antimicrobial resistance (1.31, 1.16–1.48). After adjustment for these variables, greater knowledge was significantly associated with four cognitive factors: perceived susceptibility, attitude toward hand hygiene, self-efficacy, and motivation.
Conclusions
We found a low level of MDRO awareness and knowledge of associated control measures among French HCWs. Training on hand hygiene and measures to control MDRO spread may be helpful in shaping beliefs and perceptions on MDRO control among other possible associated factors. Messages should be tailored to professional status and their perception. Other approaches should be designed, with more effective methods of training and cognitive interventions.
Trial registration
Clinical Trials.gov NCT02265471. Registered 16 October 2014 - Retrospectively registered.
Similar content being viewed by others
Background
Antimicrobial resistance (AMR) is a growing problem worldwide. Multidrug-resistant organisms (MDROs) are challenging healthcare workers (HCWs) in their daily practice and there is an urgent need for improved infection prevention and control (IPC) practices and antimicrobial stewardship. Many guidelines and training materials have been issued for the control of MDRO transmission. Successful interventions have served as a framework for the implementation of further control programmes [1, 2]. However, recommendations alone are not enough to improve compliance with best practices. As demonstrated in the context of hand hygiene, guidelines must be associated with an implementation process considering contextual and behavioural determinants [3]. A strong association between knowledge, perceptions, and ultimately actions has been suggested in previous research on AMR [4, 5]. Some studies found an impact of knowledge, attitudes, and personal perceptions, including perceived benefits and barriers, on the behaviours and practices of HCWs in IPC [6,7,8,9].
Surveys on the knowledge and perception of AMR have primarily focused on antibiotic prescription, excluding infection control measures [10]. More recently, several studies have jointly assessed knowledge, attitudes, and practices regarding both MDROs and transmission precautions [11,12,13]. The findings indicated that few physicians were concerned with their own infection control practices, though they were aware of the threat of AMR. Most of them targeted junior doctors or medical students [14].
Our aim was to explore awareness among HCWs by evaluating their general knowledge on MDROs and associated control measures, comparing perceptions between professional categories, and studying the impact of training and beliefs. Hence, a questionnaire-based survey was developed to identify the association between knowledge, perceptions, and attitudes towards MDROs and control measures (gloves, hand hygiene).
Methods
Hospitals and participants
The study was conducted in 58 randomly selected French healthcare facilities (HCFs). Among them, nine were university hospitals or referral centres for cancer (UHs), 10 non-university public hospitals (NUPHs), 10 private HCFs, and 29 in a group mixing local hospitals (n = 10), nursing homes (n = 10), rehabilitation and long-term care facilities (LTCFs, n = 9). Random sampling was used to select participating HCFs, stratified into five geographical areas corresponding to the French interregional coordinating centres for infection prevention and control (CCLIN). This sample represented 2.0% of the total number of French HCFs (58/2931).
Each initial randomised HCF (n = 60) was contacted through the local infection prevention and control (IPC) team. A total of 46 HCFs agreed to participate during the first round of randomisation. When an HCF declined to participate (n = 21), another HCF was randomly selected following the same scheme of stratification sampling. Twelve other HCFs agreed to participate across three other rounds of sampling. The number of clinical units participating in the survey was correlated with the total number of beds in the facility, from 15 to 50% of clinical units randomly selected in large HCFs, to 100% in small HCFs. Adult and paediatric clinical units were eligible, including intensive care (ICU), medical and surgical units, rehabilitation and long-term care, emergency, outpatient, and radiology units. Eligible HCWs included physicians (senior, junior, and medical students) and non-medical professionals i.e. nurses, nurse aides, nursing students, head nurses, hospital service agents (including cleaning staff and domestic services) and medical-technical agents (including technical staff members, i.e. dieticians, X-ray technicians, physiotherapists, psychologists, …) present during the day and night shifts. HCWs in laboratories, housekeeping personnel, and administrative personnel were excluded.
Study design
This cross-sectional study was performed from June 2014 to March 2016. Interviewers included members of the study team and members of the local IPC team. The day of the survey, interviewers went through the different included units several times a day (including the night) to ask participants to complete anonymously a self-administered questionnaire requiring 10–15 min to fill. The total number of HCWs present on site the day of the survey was used to compute the participation rate. This information was provided by the local human resources services.
Questionnaire
The questionnaire was structured in three different parts: (i) professional characteristics including gender, age, professional status, job tenure, working unit, main activity of the unit, working shift, and previous training sessions during the last 3 years about hand hygiene and contact precautions; (ii) assessment of knowledge on the transmission and control of MDROs (Additional file 1: Table S1) including hand hygiene (three questions), glove use (two questions), and epidemiology of MDROs (three questions); (iii) and the perception of AMR included (Additional file 1: Table S2) the perceived threat of MDROs (three questions), individual cognitive factors for hand hygiene compliance (eight questions), based on the theory of health belief model [15,16,17]. This model enabled the assessment of the following criteria: perceived susceptibility, perceived knowledge, intention to adhere (perceived practice), attitudes toward hand hygiene, perceived behavioural norm, perceived subjective norm, self-efficacy, and motivation (Additional file 1: Table S3) regarding one specific topic. Items related to beliefs and perception were coded on a 7-point Likert scale, ranging from 1, “strongly disagree” to 7, “strongly agree” with the statement of the item. The questions were selected by the steering group which included experts in infectious diseases, public health, infection control and statistics. Questions on infection control (hand hygiene and gloves) and the epidemiology of AMR were selected according to current national guidelines. The questionnaire was first tested among individuals from various professional backgrounds, and some questions were revised slightly according to their comments.
Statistical analysis
Continuous variables were expressed as mean and standard deviation (SD) or median and interquartile range (Q1: 25th percentile; Q3: 75th percentile), and categorical variables as frequency (percentage). Comparisons between two groups were made using the Chi2 test or Student’s t test or their corresponding non-parametric versions, Fisher’s test or the Wilcoxon rank sum test, as appropriate. Comparisons between more than two groups were made using the Hochberg method for multiple comparisons in order to adjust for the alpha level. The principal endpoint was the knowledge score (KS) defined by the sum of correct answers out of eight questions (Additional file 1: Table S1). The KS was compared among HCF categories, age classes, professional statuses, working units, and other professional characteristics, using the Kruskal–Wallis test.
The KS was then categorised in two classes by its median value, KS lower than four or KS equal to or greater than four. Multivariate logistic regression models were used to assess the association between professional characteristics and KS.
For multivariate analyses, variable selection was done in order to select the best subset of predictors of knowledge. Initial selection was determined by the clinical value of predictors. Then, final selection of explanatory variables in the multivariate analysis was done using stepwise methods based on the AIC (Akaike Information Criterion). All questions about perception and beliefs on the 7-point Likert scale were dichotomised: no agreement with the proposition (“Strongly disagree”, “Disagree”, “Somewhat disagree”, “Neither agree nor disagree”, and “Somewhat agree”) and agreement with the proposition (“Agree” and “Strongly agree”). The latter denoted strong positive agreement with the proposition. All other quotations scores (from 1 to 5) were considered negative according to previous studies in the field of infection control [17]. Significant associations between perception and KS in the univariable analysis were then adjusted for significant variables in the first multivariable model. Reference groups for multivariate analysis were selected from an epidemiological perspective. R software (v3.14) was used.
Results
Healthcare facilities and participants
Among the 58 participating HCFs, a total of 8716 HCWs completed the questionnaire. The overall participation rate was 74% (8716/11,753), ranging from 35 to 100% across individual HCFs, with participations of 55% (1291/2335) for the medical healthcare workers (MWs) and 79% (7425/9418) for the non-medical healthcare workers (NMWs). The characteristics of the population are presented in Table 1. Most participants were female (7103/8716; 83%), representing 50% (63/291) and 88% (6469/7425) of MWs and NMWs, respectively. The median age was 33 (Q1; Q3, 27; 47) years old and 37 (28; 48) years old in MWs and NMWs, respectively. Overall, 5753 (68%) and 2787 (34%) HCWs declared having been trained on hand hygiene and control of AMR over the 3 years prior to the survey, respectively.
Awareness and associated factors
The mean KS on AMR and control measures was 4.7/8 among MWs and 3.6/8 among NMWs (P < 0.0001) (Table 2). They both differed between the type of HCFs (p < 0.001), with a medical KS significantly higher in UHs, and a non-medical KS significantly lower in the LTCF group.
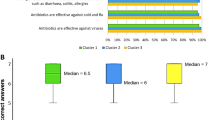
Most respondents wrongly thought that hand hygiene was more important after than before contact with a patient (58% MWs, 52% NMWs); alcohol-based hand rub (AHR) was correctly considered more effective than antiseptic or plain soap (76% MWs, 50% NMWs) (Additional file 1: Table S1). A large proportion, (> 90%) believed that gloves were indicated for contact precautions. Standard precautions (hand hygiene after contact with the patient’s environment and no glove wearing for contact with the patient’s intact skin) were correctly known (higher than 80% in both MWs and NMWs).
Knowledge on the MDRO epidemiology was greater among MWs; 85% of MWs and 67% of NMWs considered that methicillin-resistant Staphylococcus aureus (MRSA) was mainly hand-transmitted. A large proportion of respondents thought that rates of both MRSA (89% MWs, 95% NMWs) and extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBLPE) (83% MWs, 42% NMWs) were increasing in France.
In the univariate analysis (Table 3), variables associated with a KS ≥ 4 were: the category of HCF, male gender, an age between 26 and 35 years, the medical professional status, a shorter current job tenure, working in an ICU and having been trained on AMR control measures. In the multivariate logistic regression analysis, five variables remained positively associated with greater knowledge: working in a UH (adjusted odds ratio, 1.41; 95% CI, 1.16–1.70; p < 0.005); age classes 26–35 years (1.43, 1.23–1.67, p < 0.0001) and 36–45 years (1.19, 1.01–1.40, p = 0.037); medical professional status (3.70, 3.09–4.44, p < 0.0001), working in an ICU (1.28, 1.06–1.55, p = 0.011) and having been trained on control of AMR within the previous 3 years (1.31, 1.16–1.48, p < 0.0001). Working in rehabilitation and long-term care units (0.81, 0.68–0.96, p = 0.014) was negatively associated with a higher KS.
Knowledge score and perceptions
After adjustment for variables significantly associated with better knowledge (type of HCF, male gender, age, medical professional status, working unit, and having received training sessions), a higher KS was significantly associated with four cognitive factors: perceived susceptibility (2.33, 95% CI, 1.95–2.78, p < 0.0001), positive attitude toward hand hygiene (1.98, 1.65–2.37, p < 0.0001), self–efficacy (1.22, 1.09–1.38, p < 0.001), and motivation (1.42, 1.24–1.62, p < 0.0001) (Table 4).
Perceptions of the antimicrobial resistance threat
Most participants perceived AMR as a national problem (Additional file 1: Table S2) (98% MWs, 88% NMWs), while fewer (66% MWs, 40% NMWs) viewed AMR as a local problem, with a low impact on their daily practices (65% MWs, 38% NMWs).
Discussion
To date, this is the first study evaluating the association between knowledge of AMR epidemiology, the associated control measures, and the individual cognitive factors, including both MWs and NMWs from a national representative population of HCFs. The 74% participation rate was unexpectedly high and may be ascribable to the active participation of IPC teams and the direct physical contact of investigators with ward staff. This large panel therefore accurately reflects the situation in France and enabled comparison of the KS in different categories of HCFs and types of healthcare units.
We found poor knowledge of current AMR epidemiology and modest knowledge of best practices in prevention of cross-transmission. Variations were observed across professional categories, highlighting two profiles. Professionals with the highest knowledge profile were young medical doctors, working in an ICU, recently trained and with awareness of and readiness to act against AMR. This profile perceived poor compliance with hand hygiene as a breach in patient safety, with a willingness to comply with hand hygiene recommendations. The 26–35-year age class working in UHs was associated with greater knowledge, possibly reflecting improved and fresh education on the topic during medical or nursing studies. On the other hand, low knowledge was found among nurse aides from small LTCFs. Nurse aides are key people for infection control. They routinely contribute to patient care and diaper changes, with a high risk of hand contamination and subsequent transmission [18]. This strongly suggests that knowledge should primarily be improved in that population. Small HCFs should also be a target for education as they may suffer of a lack of IPC human resources.
Fifteen years after the introduction of AHR in French healthcare settings [17, 19], knowledge of hand hygiene best practices still appeared poor. AHR was considered less effective than antiseptic or plain soap in a significant proportion of respondents, as high as 50% of NMWs, which was very disappointing given the multiple national campaigns promoting AHR and the use of AHR consumption as a national quality indicator. Two previous studies reported that medical students considered poor hand hygiene compliance as one of the least important contributors to AMR [11, 20]. In consequence, educational messages provided by IPC teams should be simplified, focused on the reasons for and consequences of poor hand hygiene practices and be tailored to the healthcare professionals involved.
Furthermore, less than 50% of HCWs thought that hand hygiene was more important after than before a contact with patients. These results illustrate a general misconception of hand hygiene best practices, even though reported consumption of AHR in France is fairly high compared to other European countries [21]. Healthcare-associated infections are the result of a complex chain, including the many individuals involved in patient care. The consequences of poor hand hygiene compliance are intangible for front-line staff, not considering the actual burden of AMR for patients as a consequence of their individual practices. The perception of AMR as a national problem but not a local or individual one supports this hypothesis. Accurate feedback of local data may improve awareness of HCWs [22].
.HCWs still believe they need to wear gloves for contact precautions despite its withdrawal from French recommendations in 2010. Several guidelines have recently been issued for the control of MDRO transmission, with evolving recommendations (e.g. the debated need for contact precaution for ESBLP-E. coli) [1, 23]. These recurrent changes in recommendations may be confusing for HCWs, complicating the implementation of good practices. Sixty-eight percent of HCWs reported having received training on hand hygiene during the last 3 years. This proportion, albeit high, may be considered insufficient. Education and training of HCWs are one pillar of infection control programmes and efforts must be made to implement regular courses and target all HCW categories [24]. However, formal training should be included in a larger programme including combined measures, according to the rules of bundling and multifaceted interventions: reminders at the workplace, audit and feedback, use of AHR consumption as a performance indicator, leadership, incentive and rewards … [25]. For example, AHR consumption is a publicly released quality indicator for all healthcare facilities in France, and facilities are urged to use AHR consumption as an internal quality indicator; most healthcare facilities are registered to take part in national hand hygiene day, on the 5th of May, as well as in the national yearly week of patient safety. Until now, educational programmes have usually been based on classic presentations with lectures given to a passive audience. New technologies such as simulation, virtual reality, serious games and e-learning applications, playing with the trainee’s emotions, bring new possibilities to the field of medical training and could lead to valuable improvement in learning outcomes [26]. After adjustment for confounding variables, a higher KS was significantly associated with four cognitive factors: perceived susceptibility, attitude toward hand hygiene, self-efficacy, and motivation. Our survey, as previously described [27], suggests a perceived lack in patient safety by HCWs when hand hygiene in inadequately performed. One may consider that the perceived susceptibility, i.e. the perceived risk to patient, which was the strongest factor linked to higher knowledge, derived from the higher knowledge by itself. Nevertheless, it is unknown whether the other cognitive factors impact higher knowledge, or whether higher knowledge obtained from other sources, such as training sessions or medical education, translates into more belief in and perception of the importance of hand hygiene. The interactions probably are intricate, suggesting that training on hand hygiene and AMR is critical in shaping beliefs in and perceptions of the control of AMR. A new approach based on psychologically tailored hand hygiene interventions regarding MDRO has recently been described [28]. Tailored intervention based on the Health Action Process Approach (HAPA) led to better compliance with hand hygiene, with in turn a decrease in the MDRO infection rate.
Understanding the impact of individual infection control behaviours on AMR spread may increase the likelihood of compliance. An adapted approach is needed to heighten an individual’s understanding. A unique strategy is not sufficient in a such context and efforts should be made to implement personalised and multiple tools. One approach could be supported by evidence-based medicine. A recent study stated that recommendations appear to be imposed on medical students and junior physicians without reference to the scientific evidence, which therefore does not encourage high compliance with hand hygiene [22]. Feedback of local data could increase awareness among HCWs, while demonstrating threats in their own setting and the consequences of their own practices. On the other hand, social norms (perceived behavioural and subjective norms) are independent of awareness, but surveys have demonstrated that they shape hygiene behaviours [17, 29]. For instance, perceived peer handwashing frequency significantly impacted the behaviour of professionals. Intervention regarding social norms could be a complementary approach.
Our survey had some limitations. Firstly, the study was performed in France and was probably not representative of the healthcare systems of other countries. Indeed, to our knowledge, only one study has been conducted in several European countries, but focused on antibiotic prescribing and AMR among medical students [11]. Secondly, the questionnaire was unique and questions could have been understood differently by individuals according to their professional status. Hence, use of a 7-point scale permitted a large range of responses and more precision [30]. Thirdly, it is likely that the respondents were more motivated and better informed than non-respondents, thus increasing the rate of positive responses. However, the high participation rate could offset this bias. Finally, some answers may have been collective rather than individual, thereby falsely increasing KS.
Conclusions
In view of insufficient knowledge among HCWs, training should be extended to all HCW categories, and simplified to address simple control measures. New strategies to enhance awareness should probably incorporate different professional beliefs and contextual institutional factors, suggesting new possible areas of intervention. Non-medical HCWs with a lower educational level and small HCFs should be prioritised, by adapting IPC tools and education methods used in large university hospitals. Designing new strategies for the effective implementation of evidence-based infection control practices is essential and should be a priority at all levels.
Availability of data and materials
Tools (knowledge and perception questionnaires) are included in this published article and its supplementary information files. The datasets generated and/or analysed during the current study are not publicly available.
Abbreviations
- AHR:
-
Alcohol-based hand rub
- AMR:
-
Antimicrobial resistance
- ESBLP:
-
Extended-spectrum beta-lactamase-producing
- HAPA:
-
Health Action Process Approach
- HCF:
-
Healthcare facility
- HCW:
-
Healthcare worker
- ICU:
-
Intensive care unit
- IPC:
-
Infection prevention and control
- KS:
-
Knowledge score
- LTCF:
-
Long-term care facilities
- MDRO:
-
Multidrug-resistant organisms
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- MW:
-
Medical healthcare worker
- NMW:
-
Non-medical healthcare worker
- NUPH:
-
Non-university public hospitals
- Q1:
-
25th percentile
- Q3:
-
75th percentile
- SD:
-
Standard deviation
- UH:
-
University hospitals or referral centres for cancer
References
Tacconelli E, Cataldo MA, Dancer SJ, De Angelis G, Falcone M, Frank U, et al. ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug-resistant gram-negative bacteria in hospitalized patients. Clin Microbiol Infect. 2014;20:1–55.
Muto CA, Jernigan JA, Ostrowsky BE, Richet HM, Jarvis WR, Boyce JM, et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect Control Hosp Epidemiol. 2003;24(5):362–86.
Stewardson AJ, Sax H, Gayet-Ageron A, Touveneau S, Longtin Y, Zingg W, et al. Enhanced performance feedback and patient participation to improve hand hygiene compliance of health-care workers in the setting of established multimodal promotion: a single-Centre, cluster randomised controlled trial. Lancet Infect Dis. 2016;16(12):1345–55.
Giblin TB. Clinicians’ perceptions of the problem of antimicrobial resistance in health care facilities. Arch Intern Med. 2004;164(15):1662.
Burnett E, Kearney N, Johnston B, Corlett J, MacGillivray S. Understanding factors that impact on health care professionals’ risk perceptions and responses toward Clostridium difficile and meticillin-resistant Staphylococcus aureus: a structured literature review. Am J Infect Control. 2013;41(5):394–400.
Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Educ Q. 1988;15(2):175–83.
Wolf R, Lewis D, Cochran R, Richards C. Nursing staff perceptions of methicillin-resistant Staphylococcus aureus and infection control in a long-term care facility. J Am Med Dir Assoc. 2008;9(5):342–6.
Srinivasan A, Song X, Richards A, Sinkowitz-Cochran R, Cardo D, Rand C. A survey of knowledge, attitudes, and beliefs of house staff physicians from various specialties concerning antimicrobial use and resistance. Arch Intern Med. 2004;164(13):1451–6.
Celeste C, Jolivet S, Bonneton M, Brun-Buisson C, Jansen C. Healthcare workers’ knowledge and perceptions of the risks associated with emerging extensively drug-resistant bacteria. Méd Mal Infect. 2017;47(7):459–69.
McCullough AR, Rathbone J, Parekh S, Hoffmann TC, Del Mar CB. Not in my backyard: a systematic review of clinicians’ knowledge and beliefs about antibiotic resistance. J Antimicrob Chemother. 2015;70(9):2465–73.
Dyar OJ, Pulcini C, Howard P, Nathwani D, on behalf of ESGAP, (the ESCMID Study Group for Antibiotic Policies), et al. European medical students: a first multicentre study of knowledge, attitudes and perceptions of antibiotic prescribing and antibiotic resistance. J Antimicrob Chemother. 2014;69(3):842–6.
Milori A, Milioria E. Antibiotic resistance and infection control: physicians aspects and beliefs. J Antimicrob Agents. 2017;03(02).
Dyar O, Hills H, Seitz L-T, Perry A, Ashiru-Oredope D. Assessing the knowledge, attitudes and behaviors of human and animal health students towards antibiotic use and resistance: a pilot cross-sectional study in the UK. Antibiotics. 2018;7(1):10.
Marschall P, Hübner N-O, Maletzki S, Wilke F, Dittmann K, Kramer A. Attitudes and perceptions of health care workers in northeastern Germany about multidrug-resistant organisms. Am J Infect Control. 2016;44(6):e91–4.
Lucet J-C, Nicolas-Chanoine M-H, Roy C, Riveros-Palacios O, Diamantis S, Le Grand J, et al. Antibiotic use: knowledge and perceptions in two university hospitals. J Antimicrob Chemother. 2011;66(4):936–40.
Bouadma L, Mourvillier B, Deiler V, Derennes N, Le Corre B, Lolom I, et al. Changes in knowledge, beliefs, and perceptions throughout a multifaceted behavioral program aimed at preventing ventilator-associated pneumonia. Intensive Care Med. 2010;36(8):1341–7.
Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV. Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med. 2004;141(1):1–8.
Pessoa-Silva CL, Posfay-Barbe K, Pfister R, Touveneau S, Perneger TV, Pittet D. Attitudes and perceptions toward hand hygiene among healthcare workers caring for critically ill neonates. Infect Control Hosp Epidemiol. 2005;26(03):305–11.
Jarlier V. Curbing methicillin-resistant Staphylococcus aureus in 38 French hospitals through a 15-year institutional control program. Arch Intern Med. 2010;170(6):552.
Haque M, Iza A, Rahman N, Zulkifli Z, Ismail S. Antibiotic prescribing and resistance: knowledge level of medical students of clinical years of university sultan Zainal Abidin, Malaysia. Ther Clin Risk Manag. 2016;413.
Suetens C, Hopkins S, Kolman J, Högberg LD. European centre for disease prevention and control. Point prevalence survey of healthcare-associated infections and antimicrobial use in European acute care hospitals: 2011–2012. Luxembourg: Publications Office; 2013.
Labricciosa FM, Sartelli M, Correia S, Abbo LM, Severo M, Ansaloni L, et al. Emergency surgeons’ perceptions and attitudes towards antibiotic prescribing and resistance: a worldwide cross-sectional survey. World J Emerg Surg. 2018;13(1).
World Health Organization. Guidelines for the prevention and control of carbapenem-resistant Enterobacteriaceae, Acinetobacter baumannii and Pseudomonas aeruginosa in health care facilities. Geneva: World Health Organization; 2017.
Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, et al. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. Lancet Infect Dis. 2015;15(2):212–24.
Kingston L, O’Connell NH, Dunne CP. Hand hygiene-related clinical trials reported since 2010: a systematic review. J Hosp Infect. 2016;92(4):309–20.
Cook DA, Hatala R, Brydges R, Zendejas B, Szostek JH, Wang AT, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9).
Alothman A, Bosaeed M, Algwizani A, Alsulaiman M, Alalwan A, Binsalih S, et al. Knowledge and attitude of physicians toward prescribing antibiotics and the risk of resistance in two reference hospitals. Infect Dis Res Treat. 2016;33.
von Lengerke T, Ebadi E, Schock B, Krauth C, Lange K, Stahmeyer JT, et al. Impact of psychologically tailored hand hygiene interventions on nosocomial infections with multidrug-resistant organisms: results of the cluster-randomized controlled trial PSYGIENE. Antimicrob Resist Infect Control. 2019;8(1).
Dickie R, Rasmussen S, Cain R, Williams L, MacKay W. The effects of perceived social norms on handwashing behaviour in students. Psychol Health Med. 2018;23(2):154–9.
Alumran A, Hou X-Y, Hurst C. Validity and reliability of instruments designed to measure factors influencing the overuse of antibiotics. J Infect Public Health. 2012;5(3):221–32.
Acknowledgements
We are enormously grateful to the IPC teams, healthcare professionals, and volunteers for their participation.
The Percept-R Study Group: Aveline Isabelle (Clinique d’Alençon), Bracco Christelle (Clinique médicale et cardiologique d’Aressy), Lacombe Manuelle (La Morlande, Avallon), Colin Yolande (Centre médical L’Arbizon, Bagnères de Bigorre), Poulingue Géraldine (Centre Hospitalier de Barentin), Lesourd Fabien (Polyclinique du Plateau, Bezons), Rogues Anne-Marie (CHU de Bordeaux), Magne Béatrice (Hôpital local de Bort-Les-Orgues), Mouzaoui Marc (Hopital de Boscamnan), Daniel Petrelli (Centre Médical Chant’Ours, Briançon), Picot Franck (CH de Brive), Canivet Anne (Centre François Baclesse, Caen), Stoeckel Vincent (CH de Chalons en Champagne), Marchal Lydia (Etablissement Public Intercommunal 3H Santé, Cirey sur Vezouze), Boris Alexandre (Clinique du Dc Jean Causse, Colombiers), Tiv Michel (Centre Georges-François Leclerc, Dijon), Piriou Gilles (CH de Douarnenez), Lallart Dominique-Louis (Centre Sainte Barbe, Fouquières les Lens), Lecoq Marianne (Centre Les Jonquilles, Gainnevielle), Pina Patrick (Hôpital local Hôpital Saint Louis, Jouars Pontchartrain), Barege Patrice (Clinique Sainte-Anne, Langon), Josso Christophe (Hôpital intercommunal de la presqu’ile Estadieu, Le Croisic), Herbin Claire (EHPAD Public du Luc en Provence), Degallaix Dominique (CH Robert Bisson, Lisieux), Doublier Laetitia (Hôpital Local Lucien Boissin, Longuejumelles), Constantin Nicole (CH de Lourdes), Ludvig-Serge Aho-Glélé (CHU Dijon), Parer Sylvie (CHU de Montpellier), Minchella Amandine (ICM Institut Régional du Cancer de Montpellier), Romand Karine (Centre Hospitalier Paul Nappez, Morteau), Bentchikou Hicham (Centre de Réadaptation de Mulhouse), Petitfrère Manuel (Clinique Amboise Paré, Nancy), Lepelletier Didier (CHU de Nantes), Vaillé Jean-louis (Polyclinique Kennedy, Nimes), Houdou Sylvie (Centre François Gallouédec, Parigné-l’Évêque), Rahal Gisèle (Hôpital Privé des Peupliers), Miquel Chantal (CH de Perpignan), Jaudinot Christel (Maison de retraite Saint Thomas de Villeneuve, Plougastel) Dehaese Olivier (CH Guy Thomas, Riom), Thouvenin Dominique (Le Clos des Platanes et Hauts Buissons, Romilly sur Seine), Pascal Eliane (EHPAD Mapi, Rosny sous Bois), Marini Hélène, Merle Véronique (CHU de Rouen), Leroux Elisabeth (Centre de réadaptation Villa Notre Dame, Saint Gilles Croix De Vie), Laurent Oleessya (Hôpital privé Guillaume de Varye, Saint-Doulchard), Cavarec-Cuoq Marie-Claude (Centre médical des 7 collines, St Etienne) Carrière Isabelle (Hôpital Local Maurice André, Saint-Galmier), Millet Elisabeth (Centre Hospitalier Intercommunal Monts et Barrages, Saint-Leonard-de-Noblat), Fontaine Xavier (Château de Chaillé, Saint-Martin-lès-Melle), Markiewicz Amélie (CH de Seclin), Germain Yves (SSR des Elieux, Seichamps), Coppens Magali (Résidence Champfleury, Sèvres), Jean Sébastien Trescher (CH de Saint-Die des Vosges), Duperrier Valérie (Etablissement des Diaconesses, Strasbourg), Paba Odile (Au bon secours, Vendome), Fanck; Marie-Noëlle (EHPAD Saint François, Vernaison), Jezequel Jocelyn (CH de Verneuil-sur-Avre), Velardo Danielle, Gachot Bertrand (Institut Gustave Roussy, Villejuif), Lestra Bénédicte (Hôpital Local Claude Dejean, Villeneuve-de-Berg).
Funding
This study was supported by a public grant from the French Ministry of Health (PREPS 2012–002-0077).
Author information
Authors and Affiliations
Consortia
Contributions
GB and JCL conceived the study and are the principal investigators. MEF, FT, PA, CP, ESW, JR, JRZ contributed to the design of the study. LV coordinated recruitment and acquisition of study data. MEF managed the study data and did the statistical analyses. JCL, LV, GB, MEF contributed to the analysis of study data. All authors contributed to the interpretation of the data and approved the final version of the manuscript after critical review.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This project (Clinical trial NCT02265471) was approved by the Ethics Committee of the HUPNVS (CEERB Paris Nord, 16–018). The anonymity of all respondents was guaranteed, and only non-identifying characteristics were requested. An information form was administered to each participant. The study was approved by the French Data Protection Authority (CNIL).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Table S1. Knowledge of antimicrobial resistance and infection control measures. Table S2. Perceptions regarding antimicrobial resistance and control measures. Table S3. Questions on perception of antimicrobial resistance and control measures.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Vaillant, L., Birgand, G., Esposito-Farese, M. et al. Awareness among French healthcare workers of the transmission of multidrug resistant organisms: a large cross-sectional survey. Antimicrob Resist Infect Control 8, 173 (2019). https://doi.org/10.1186/s13756-019-0625-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-019-0625-0