Abstract
Purpose
Prevention of ventilator-associated pneumonia (VAP) requires a complex approach that should include factors affecting healthcare workers’ (HCWs) behavior. This study attempted to assess change of individual factors throughout a multifaceted program focusing on VAP prevention.
Methods
The prevention program involved all HCWs in a 20-bed medical intensive care unit (ICU) and included a multidisciplinary task force, an educational session, direct observations and performance feedback, technical improvements, and reminders. Knowledge, beliefs, and perceptions (cognitive factors) were assessed with a test and a self-reporting questionnaire based on social-cognitive theories. They were completed before and 1 and 12 months after the educational session.
Results
Of the 100 HCWs initially evaluated, 84 were present 1 year later. Overall, individual factors (knowledge and cognitive factors) changed positively and significantly, immediately after the educational session. Five cognitive factors were significantly associated with knowledge: perceived susceptibility, seriousness, knowledge, benefits, and self-efficacy (P < 0.05). The other factors, i.e., perceived barriers, subjective and behavioral norm, intention to perform action, and motivation, were not. The positive cognitive change was significantly reinforced at 1 year. Three distinct cognitive profiles derived from answers to the baseline questionnaire were individualized. The positive impact of our behavioral approach was highest for the HCW group with the lowest baseline cognitive profiles.
Conclusions
Behavior changed gradually throughout the program and was especially pronounced for HCWs with the lowest baseline cognitive profiles.
Similar content being viewed by others
Introduction
Although well-documented evidence-based ventilator-associated pneumonia (VAP) prevention guidelines exist [1], they remain poorly implemented in most intensive care units (ICUs) [2, 3]. The results of some studies indicate that multimodal interventions have the greatest chance of successfully improving adherence to practices [4–9].
We recently showed that a multifaceted program significantly improved compliance with most preventative measures that resulted in a significant, sustained reduction of VAP cases (per 1,000 ventilator-days) during the year before and 1 and 2 years after its implementation: 23.5, 14.9, and 11.5, respectively [10].
Learning from the behavioral science and social-cognitive models could improve our understanding of human behavior and HCWs’ compliance with guidelines [11, 12]. The concept of behavior is dependent on factors that predispose (knowledge, perceptions, and beliefs), enable (access), and reinforce (feedback) an individual to engage in a particular behavior. The present study assessed the modification of predisposing factors throughout our multifaceted prevention program.
Methods
Setting
Bichat–Claude-Bernard Hospital is a 950-bed university hospital, serving as a primary and tertiary care facility, located in Paris, France. The medical ICU (MICU) has 20 beds, and admits an average of 750 patients/year. The hospital’s Institutional Review Board and its Ethics Committee approved the study. All participants gave written consent prior to participation.
Study design
We prospectively assessed all HCWs’ predisposing factors (knowledge and cognitive factors: beliefs and perceptions) throughout a multifaceted behavioral program (Fig. 1), which combined: an educational session to encourage HCWs to adopt recommended practices; regular reminders and performance assessment feedback to reinforce changes; and technical improvements to facilitate compliance with the less feasible measures. Two simple devices were adopted: (1) a bicolored plastic ribbon attached at the head of the bed to indicate its appropriate elevation, and (2) continuous monitoring of tracheal cuff pressure, triggering an alarm when pressure fell below 20 cmH2O.
Recommendations focusing on eight targets, previously detailed [10], were selected on the following criteria: they had to be (1) included in recently published guidelines [1], (2) easily and precisely defined acts, and (3) directly concerned with HCWs’ bedside behaviors.
The centerpiece of the educational session consisted of a 3-h mandatory slide presentation (all aspects of VAP) with interactive discussion. After that session, each participant received a booklet containing a summary of the program.
Reminders were displayed on computer screensavers, and A3-sized color posters illustrating the eight targeted preventative measures were also posted throughout the MICU.
Performance feedback consisted of regular meetings, graphs documenting compliance, and VAP rates posted in visible places for HCWs and used as screensavers throughout the MICU.
Bedside observation was used to evaluate hand hygiene, and gowning and gloving. Backrest elevation was measured six times per day and tracheal cuff pressure was measured twice daily, at random periods. The acts necessary to satisfy the other four measures (avoid ventilator circuit disconnection and perform tracheal aspiration only when necessary, provide good oral hygiene, use an orogastric rather than a nasogastric tube, and avoid gastric overdistension) were recorded on daily nursing surveillance forms.
Two questionnaires were filled out just before the educational session, and 1 and 12 months thereafter. A 30-question test (30 min) assessed theoretical knowledge, and a self-reporting questionnaire (5 min), based on social-cognitive theories applied to health-related behaviors, assessed cognitive factors predicting a behavior (Table 1) [12, 13]. By using single questions for each item and a Likert seven-point scale for answers, we assessed ten cognitive factors. Scale points of 6 or 7, the highest positive perceptive evaluations, were considered positive answers; all other points were considered negative answers. Motivation to prevent VAP was assessed using a three-point scale, and only the response “yes” was considered a positive answer.
We distinguished an early phase, up to 1 month after the educational session, and a late phase between 1 month and 1 year thereafter.
Statistical analysis
Categorical variables expressed as percentage and continuous variables as mean ± standard deviation (SD) were compared using parametric or nonparametric tests, as appropriate. We performed two-way repeated-measures analysis of variance (with the factors being time and group). The data satisfied assumptions for two-way analysis of variance for repeated measures. When appropriate, post hoc analysis was performed using a pairwise multiple-comparison procedure (Dunn’s test). P ≤ 0.05 in a two-tailed test was considered statistically significant. All statistics and graphs were obtained with GraphPad Prism version 4.0 (GraphPad Software, San Diego, CA). Ward’s method was applied for hierarchical cluster analysis to identify groups of HCWs with similar response patterns to the self-reporting questionnaire at baseline, e.g., similar cognitive profiles, using the statistical software program XLSTAT-Pro v7.1 for Windows (Microsoft Corp., Redmond, CA).
Results
Among 104 HCWs, 102 (98%) completed the educational session and 100 (96%) completed the two questionnaires (14 physicians, 53 nurses, 28 nurse’s aides, 5 physiotherapists); a total of 84 were still working in the MICU 1 year later. The nurses and physiotherapists were analyzed jointly, hereafter referred to as nurses.
Impact of the educational session on predisposing factors
The proportion of correct answers to the knowledge test at baseline was 39 ± 11%; 1 month after the educational session it had increased to 58 ± 16% (P < 0.001).
After the educational session, positive perceptive evaluation was significantly more frequent for all cognitive factors (P < 0.05) except “perceived benefits” (P = 0.06) and “motivation” (P = 0.20) (Table 2).
Positive perceptive evaluation was significantly associated with knowledge for five cognitive factors before and after the educational session (Table 2).
To summarize the data, three composite scores were calculated as the sums of the positive answers: (1) to all questions in the self-reporting questionnaire (sum 1, from 0 to 10), (2) to questions concerning knowledge-centered cognitive factors (sum 2, from 0 to 5), (3) to questions of non-knowledge-centered cognitive factors (sum 3, from 0 to 5).
We used sums 1–3 at baseline to determine cognitive profiles, individualizing three groups according to dissimilarity indices. Profiles A (n = 22), B (n = 33), and C (n = 45) were constituted, respectively, of 4, 5 and 19 nurse’s aides; 16, 20, and 22 nurses; and 2, 8 and 4 physicians. Profile C had significantly more nurse’s aides than nurses or physicians, and profile B included more physicians than nurse’s aides. No differences in terms of other demographic data (age, sex, seniority) were observed among the three profiles (data not shown). Baseline sums 1–3 were significantly higher for profile A than for profiles B and C, and significantly higher for profile B than for profile C (P < 0.05).
The impact of the educational program on individual factors according to the HCWs’ profession or baseline cognitive profile is described in Table E1 in the Electronic Supplementary Material (ESM). In particular, sums 1–3 changed significantly after the educational session for the three HCWs professions and for the three cognitive profiles, except sum 3 for physicians and sums 1 and 3 for profile A.
Changes 1 year later
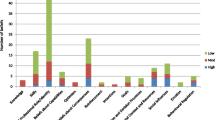
The evolutions of sums 1–3 during the study period are shown for the three different HCW populations and the three cognitive profiles in Fig. 2a and b, respectively. When factors were time and the three HCW professions, two-way repeated-measures analyses of variance indicated a group effect for sums 1 and 2 (P < 0.01), a time effect for the three sums (P < 0.01), and no significant interaction. When factors were time and the three cognitive profiles, analyses indicated a group and a time effect for all three sums (P < 0.01), and a significant interaction (P < 0.01) with reinforcing effect over time for cognitive profile C.
Changes in composite scores throughout the multifaceted program according to HCW profession (a) or cognitive profile (b) (two-way analysis of variance). a Sum of the positive answers to all questions in the self-reporting questionnaire (from 0 to 10). b Sum of the positive answers to questions concerning knowledge-centered cognitive factors: perceived susceptibility, seriousness, knowledge, benefits, and self-efficacy (from 0 to 5). c Sum of the positive answers to questions of non-knowledge-centered cognitive factors: perceived barriers, behavioral norm, subjective norm, intention-to-perform action, and motivation (from 0 to 5)
Discussion
We evaluated the association between knowledge and cognitive factors of HCWs from an MICU, as part of a multifaceted program aimed at improving compliance with VAP-prevention measures. Moreover the individual factors were evaluated thrice, thereby allowing appreciation of change over time. Three main conclusions can be drawn from our study.
First, overall, individual factors changed positively and significantly, immediately after the educational session, and some cognitive factors were significantly linked to knowledge. Pertinently, knowledge is clearly necessary, but not sufficient, to induce significant behavioral changes [14, 15]. Thus, interventions to modify behavior need to consider cognitive factors and empirical knowledge.
Second, the gradual positive modification of cognitive factors throughout the multifaceted program after the educational session suggests that the different components coalesced to induce behavioral change. Indeed, the transtheoretical approach views health behavioral change in several distinct stages [16]. This point suggests that an educational session alone is unlikely to induce profound behavioral changes, without an associated behavioral strategy.
Third, the educational session and more broadly the prevention program had its greatest impact on HCWs with the lowest baseline cognitive profiles, suggesting that targeting interventions to improve clinical practices to selected cognitive profiles might be more effective. Pertinently, we were able to distinguish three distinct cognitive profiles at baseline that were not linked to demographic characteristics. The cognitive profile depends on many factors and, consequently, cannot be predicted by simple demographic or socio-professional characteristics. However, poor impact of multidimensional approach on physicians was reported previously [17, 18]. We observed no significant change in sum 3 (assessing cognitive factors unrelated to knowledge) among physicians, but their small number did not allow us to draw any conclusions.
Our study has several limitations. First, other factors might have occurred concomitantly with the intervention that could have altered knowledge, beliefs, and perceptions. Such spontaneous positive changes are highly unlikely, in light of the well-known difficulty we humans have changing our bad habits. Second, it was not possible to link each individual predisposing factor with compliance at bedside, given the complexity of such clinical evaluations of compliance. Third, even though the sample size was large overall, the study may have lacked sufficient power to detect significant subgroup changes, e.g., physicians or profile A. Fourth, our study concerned a single MICU and these results might not be applicable to other ICUs, hospitals or another field. This possibility seems unlikely given the successful implementation of similar programs in a variety of fields and hospital settings. Finally, we are unable to predict the long-term impact of our program on cognitive factors because of the high HCW turnover in our MICU, as rapid decline over time of other initially successful procedural improvement interventions has been described [19, 20]. However, the sustained improvement at the 2-year evaluation was encouraging [10].
To our knowledge, this is the first study to document the complex relationship between knowledge and cognitive factors in the field of infection control, and to assess changes over a 1-year period. The modifications achieved might provide additional insights to devise successful strategies to promote change. We recommend that logistic and financial support be provided to prioritize educational programs targeting the most responsive populations according to their baseline cognitive profiles.
References
American Thoracic Society; Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
Rello J, Lorente C, Bodi M, Diaz E, Ricart M, Kollef MH (2002) Why do physicians not follow evidence-based guidelines for preventing ventilator-associated pneumonia? A survey based on the opinions of an international panel of intensivists. Chest 122:656–661
Ricart M, Lorente C, Diaz E, Kollef MH, Rello J (2003) Nursing adherence with evidence-based guidelines for preventing ventilator-associated pneumonia. Crit Care Med 31:2693–2696
Salahuddin N, Zafar A, Sukhyani L, Rahim S, Noor MF, Hussain K, Siddiqui S, Islam M, Husain SJ (2004) Reducing ventilator-associated pneumonia rates through a staff education programme. J Hosp Infect 57:223–227
Zack JE, Garrison T, Trovillion E, Clinkscale D, Coopersmith CM, Fraser VJ, Kollef MH (2002) Effect of an education program aimed at reducing the occurrence of ventilator-associated pneumonia. Crit Care Med 30:2407–2412
Babcock HM, Zack JE, Garrison T, Trovillion E, Jones M, Fraser VJ, Kollef MH (2004) An educational intervention to reduce ventilator-associated pneumonia in an integrated health system: a comparison of effects. Chest 125:2224–2231
Danchaivijitr S, Assanasen S, Apisarnthanarak A, Judaeng T, Pumsuwan V (2005) Effect of an education program on the prevention of ventilator-associated pneumonia: a multicenter study. J Med Assoc Thai 88(Suppl 10):S36–S41
Rosenthal VD, Guzman S, Crnich C (2006) Impact of an infection control program on rates of ventilator-associated pneumonia in intensive care units in 2 Argentinean hospitals. Am J Infect Control 34:58–63
Apisarnthanarak A, Pinitchai U, Thongphubeth K, Yuekyen C, Warren DK, Zack JE, Warachan B, Fraser VJ (2007) Effectiveness of an educational program to reduce ventilator-associated pneumonia in a tertiary care center in Thailand: a 4-year study. Clin Infect Dis 45:704–711
Bouadma L, Mourvillier B, Deiler V, Le Corre B, Lolom I, Régnier B, Wolff M, Lucet JC (2010) A multifaceted program to prevent ventilator-associated pneumonia: impact on compliance with preventive measures. Crit Care Med 38:789–796
Seto WH (1995) Staff compliance with infection control practices: application of behavioural sciences. J Hosp Infect 30(Suppl):107–115
Pittet D (2004) The Lowbury lecture: behaviour in infection control. J Hosp Infect 58:1–13
Pittet D, Simon A, Hugonnet S, Pessoa-Silva CL, Sauvan V, Perneger TV (2004) Hand hygiene among physicians: performance, beliefs, and perceptions. Ann Intern Med 141:1–8
Alvaran MS, Butz A, Larson E (1994) Opinions, knowledge, and self-reported practices related to infection control among nursing personnel in long-term care settings. Am J Infect Control 22:367–370
Madan AK, Raafat A, Hunt JP, Rentz D, Wahle MJ, Flint LM (2002) Barrier precautions in trauma: is knowledge enough? J Trauma 52:540–543
Prochaska JO, DiClemente CC (1983) Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol 51:390–395
Pittet D, Mourouga P, Perneger TV (1999) Compliance with handwashing in a teaching hospital. Infection Control Program. Ann Intern Med 130:126–130
Pittet D, Hugonnet S, Harbarth S, Mourouga P, Sauvan V, Touveneau S, Perneger TV (2000) Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Infection Control Programme. Lancet 356:1307–1312
Bittner MJ, Rich EC, Turner PD, Arnold WH Jr (2002) Limited impact of sustained simple feedback based on soap and paper towel consumption on the frequency of hand washing in an adult intensive care unit. Infect Control Hosp Epidemiol 23:120–126
Pittet D (2002) Promotion of hand hygiene: magic, hype, or scientific challenge? Infect Control Hosp Epidemiol 23:118–119
Acknowledgments
We are indebted to Janet Jacobson for editorial assistance. The authors thank the Infection Control Team and the nursing staff participating in this quality improvement project.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bouadma, L., Mourvillier, B., Deiler, V. et al. Changes in knowledge, beliefs, and perceptions throughout a multifaceted behavioral program aimed at preventing ventilator-associated pneumonia. Intensive Care Med 36, 1341–1347 (2010). https://doi.org/10.1007/s00134-010-1890-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-010-1890-9