Abstract
Background
Inhalation injury from smoke or chemical products and carbon monoxide poisoning are major causes of death in burn patients from fire accidents. Respiratory tract injuries from inhalation injury and carbon monoxide poisoning can lead to acute respiratory distress syndrome and cytokine storm syndrome. In the case of acute respiratory failure needing mechanical ventilation accompanied by cytokine storm, mortality is high and immediate adequate treatment at the emergency department is very important.
Case presentation
This report describes a case of acute respiratory distress syndrome and cytokine storm followed by carbon monoxide poisoning in a 34-year-old Korean male patient who was in a house fire, and was successfully treated by extracorporeal membrane oxygenation and direct hemoperfusion with polymyxin B-immobilized fiber column at emergency department.
Conclusions
To prevent mortality in acute respiratory distress syndrome with cytokine storm from inhalation injury and to promote a better prognosis, we suggest that early implication of extracorporeal membranous oxygenation along with direct hemoperfusion with polymyxin B-immobilized fiber column even at the emergency department should be considered.
Similar content being viewed by others
Background
Inhalation injury is considered an important cause of morbidity and mortality in patients with burns from fire accidents. Direct thermal injury in the upper airway, smoke-induced chemical irritation in the lower airway, and systematic chemical or metabolic injury with various chemicals constitute the major pathophysiological background that can lead to severe acute respiratory distress syndrome (ARDS) [1]. Carbon monoxide (CO) poisoning is a leading cause of death among poisoning deaths worldwide and is most often caused by house fires. In the case of toxic concentration, increases in carboxyhemoglobin (COHb) interfere with gas exchange in respiratory system, resulting in hypoxemia [2]. Hypoxemia from CO poisoning eventually causes tissue damage, which triggers an inflammatory response [3]. In terms of severe ARDS after inhalation injury, mortality is very high and aggressive treatment is needed in addition to conventional therapy including fluid restriction, protective ventilation, prone positioning, or nitric oxide inhalation [4]. Systemic inflammation caused by a “cytokine storm” due to excessive circulating cytokines also requires attention. Here, we present a case of CO intoxication and inhalation injury with secondary ARDS and cytokine storm in a patient who recovered after treatment with extracorporeal membrane oxygenation (ECMO) and direct hemoperfusion with polymyxin B-immobilized fiber (PMX-DHP) at the emergency department (ED).
Case presentation
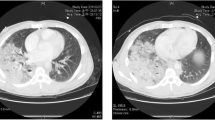
A 34-year-old Korean male with no underlying diseases was rescued from a fire in his home. When the firefighters arrived, he was lying in his bed unconscious and pulseless. Ventricular fibrillation was observed on an automated external defibrillator monitor, and 2 minutes of chest compression with 150 J shock was applied. Recovery of spontaneous circulation ensued just after defibrillation, and the patient was transferred to the emergency department (ED). Upon arrival, erythema with vesicles was found in his face, neck, chest wall, both axillary areas, and the back. In addition, he had a low estimated Glasgow Coma Scale score (3 points) and weak respiration, so intubation and mechanical ventilation support were applied. The initial blood pressure was 88/46 mmHg. Laboratory tests showed leukocytosis, elevated hepatic enzymes (aspartate transaminase 310 U/L, alanine transaminase 184 U/L) and relatively normal levels of C-reactive protein (0.07 mg/dL) and procalcitonin (0.07 ng/dL). On the other hand, the level of serum interleukin 6 (IL-6) was markedly increased to 1328 pg/mL. The initial arterial blood gas (ABG) showed hypoxemia with a low partial pressure of oxygen (PaO2 37 mmHg) as well as metabolic acidosis with a serum lactate level of 12.6 mmol/L. The percentage of serum COHb was 59%, indicating severe CO poisoning. An initial chest X-ray showed diffuse bilateral infiltration, and chest computed tomography (CT) revealed diffuse ground-glass attenuation with an anterior–posterior density gradient by dense consolidation in dependent areas, which suggests an early state of ARDS (Figure 1). Therapeutic hypothermia was applied for prevention of hypoxic brain damage. Shock requiring infusion of norepinephrine exceeding the rate of 0.5 μg/kg/minute despite adequate fluid resuscitation was observed after sedation along with therapeutic hypothermia. Even with 100% of fraction of inspired oxygen (FiO2) and maximal positive end expiratory pressure, hypoxemia (PaO2 61 mmHg) as well as hypercapnia (partial pressure of carbon dioxide 58 mmHg) progressed. Prone position ventilation and application of inhaled nitric oxide were considered, but were not implemented due to concern for rapid progression of shock. Therefore, we decided to conduct veno-veno extracorporeal membranous oxygenator (V-V ECMO) via both right and left femoral venous cannulation. Despite V-V ECMO application, hypoxemia and shock progressed. Thus, direct hemoperfusion with polymyxin B-immobilized fiber (PMX-DHP) was indicated and conducted immediately to prevent further development of cytokine storm. PMX-DHP (TORAYMYXINTM PMX-20R, TorayMedical, Tokyo, Japan) was applied with continuous renal replacement therapy (CRRT) via a nontunneled, double-lumen catheter inserted in left jugular vein, with a starting blood flow rate of 150 mL/minute for 24 hours. The patient was transferred to the intensive care unit (ICU) with ECMO and PMX-DHP. In the ICU on post-burn day 1, flexible bronchoscopy was done to assess degree of inhalation injury and to toilet the airway. Bronchoscopy revealed severe edema and congestion in the bronchial wall with carbon soot deposition. (Figure 2) With V-V ECMO maintenance and 24 hours of PMX-DHP, serum COHb percentage and IL-6 level normalized, and dramatic improvement on chest X-ray was seen within 96 hours. (Figure 3) On the seventh and eighth ICU days, the patient was weaned from V-V ECMO and the ventilator, respectively. On the 11th ICU day, the patient was moved to the general ward with a plan for systematic rehabilitation including respiratory rehabilitation. Upon transfer, the patient was alert without cognitive dysfunction, and electroencephalogram along with diffusion magnetic resonance imaging showed no definitive signs of hypoxic brain damage. However, both sensory impairment and motor weakness were observed in the right lower extremity with an abnormal result on electromyography suggesting right lumbar plexopathy. The patient was discharged from hospital with the plan of further rehabilitation through the outpatient clinic in the rehabilitation medicine department of hospital in other city.
Discussion
Inhalation injury is a disastrous injury that occurs in one-third of all burn patients, and smoke inhalation injury contributes to increased mortality, up to 20 times higher than that of burn alone [5, 6]. Smoke inhalation injury can lead to not only long-term pulmonary dysfunction but also prompt respiratory complications such as pneumonia and acute respiratory distress syndrome. ARDS might be caused by contributing factors, including smoke toxicity, bronchorrhea, alveolar permeability, and inflammatory mediator expression. The incidence of ARDS in patients with burn and inhalation injuries who required mechanical ventilation was reported in the range of 34–43% [7]. In terms of ARDS, mortality is up to 40%; and intubation, fiberoptic bronchoscopy and mechanical ventilator support are currently used as initial treatments at the ED [8]. However, in cases of refractory, severe ARDS with maximal support of mechanical ventilation, ECMO should be considered as an additional option. Recently Dabras et al. suggested that ECMO is a viable therapeutic option and can contribute to improved survival rates in patients with ECMO for ARDS after inhalation injuries [4]. Cytokine storm, or cytokine storm syndrome, is caused by excessive circulating serum cytokines after inhalation injury and is also a significant complication. Progressive, widespread, systemic inflammation leads to low vascular permeability that is manifested as vasodilatory shock and progressive organ failure resulting in a poor prognosis [9]. PMX-DHP was originally developed to adsorb endotoxins released by Gram-negative bacteria during septic shock [10]. However, several studies recently reported that PMX-DHP might be useful for ARDS patients and for removal of cytokines [11,12,13]. Therefore, in patients with severe refractory ARDS and cytokine storm, early implication of PMX-DHP for removal of cytokines and improvement of oxygenation might be considered in addition to ECMO.
Conclusion
We strongly suggest that early initiation of ECMO along with PMX-DHP even at the ED should be considered as a treatment option for severe ARDS with cytokine storm following inhalation injury to prevent mortality and to promote a better prognosis in burn patients.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CO:
-
Carbon monoxide
- ARDS:
-
Acute respiratory distress syndrome
- ED:
-
Emergency department
- ECMO:
-
Extracorporeal membrane oxygenation
- PMX-DHP:
-
Direct hemoperfusion with polymyxin B-immobilized fiber
- COHb:
-
Carboxyhemoglobin
- IL-6:
-
Interleukin 6
- ABG:
-
Arterial blood gas
- PaO2:
-
Partial pressure of oxygen
- CT:
-
Computed tomography
- V-V ECMO:
-
Veno-veno extracorporeal membranous oxygenator
- CRRT:
-
Continuous renal replacement therapy
- ICU:
-
Intensive care unit
References
Deutsch CJ, Tan A, Smailes S, Dziewulski P. The diagnosis and management of inhalation injury: an evidence based approach. Burns. 2018;44(5):1040–51.
Kinoshita H, Turkan H, Vucinic S, Naqvi S, Bedair R, Rezaee R, et al. Carbon monoxide poisoning. Toxicol Rep. 2020;7:169–73.
Eltzschig HK, Carmeliet P. Hypoxia and inflammation. N Engl J Med. 2011;364(7):656–65.
Dadras M, Wagner JM, Wallner C, Huber J, Buchwald D, Strauch J, et al. Extracorporeal membrane oxygenation for acute respiratory distress syndrome in burn patients: a case series and literature update. Burns Trauma. 2019;7:28.
Kadri SS, Miller AC, Hohmann S, Bonne S, Nielsen C, Wells C, et al. Risk factors for in-hospital mortality in smoke inhalation-associated acute lung injury: data from 68 United States Hospitals. Chest. 2016;150(6):1260–8.
Enkhbaatar P, Pruitt BA Jr, Suman O, Mlcak R, Wolf SE, Sakurai H, et al. Pathophysiology, research challenges, and clinical management of smoke inhalation injury. Lancet. 2016;388(10052):1437–46.
Sine CR, Belenkiy SM, Buel AR, Waters JA, Lundy JB, Henderson JL, et al. Acute respiratory distress syndrome in burn patients: a comparison of the Berlin and American-European definitions. J Burn Care Res. 2016;37(5):e461–9.
Belenkiy SM, Buel AR, Cannon JW, Sine CR, Aden JK, Henderson JL, et al. Acute respiratory distress syndrome in wartime military burns: application of the Berlin criteria. J Trauma Acute Care Surg. 2014;76(3):821–7.
Clark IA, Vissel B. The meteorology of cytokine storms, and the clinical usefulness of this knowledge. Semin Immunopathol. 2017;39(5):505–16.
Shoji H. Extracorporeal endotoxin removal for the treatment of sepsis: endotoxin adsorption cartridge (Toraymyxin). Ther Apher Dial. 2003;7(1):108–14.
Tsushima K, Kubo K, Koizumi T, Yamamoto H, Fujimoto K, Hora K, et al. Direct hemoperfusion using a polymyxin B immobilized column improves acute respiratory distress syndrome. J Clin Apher. 2002;17(2):97–102.
Yokoyama T, Tateishi K, Tsushima K, Agatsuma T, Yamamoto H, Koizumi T, et al. A case of severe ARDS caused by novel swine-origin influenza (A/H1N1pdm) virus: a successful treatment with direct hemoperfusion with polymyxin B-immobilized fiber. J Clin Apher. 2010;25(6):350–3.
Ishiwari M, Togashi Y, Takoi H, Kikuchi R, Kono Y, Abe S. Polymyxin B haemoperfusion treatment for respiratory failure and hyperferritinaemia due to COVID-19. Respirol Case Rep. 2020;8(9):e00679.
Acknowledgements
Not applicable.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Haeundae Paik Hospital, Inje University College of Medicine does not require ethical approval for reporting individual cases or case series. Consent to participate was not applicable because of this article being a case report.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jang, J.H., Jang, H.J., Kim, HK. et al. Acute respiratory distress syndrome caused by carbon monoxide poisoning and inhalation injury recovered after extracorporeal membrane oxygenation along with direct hemoperfusion with polymyxin B-immobilized fiber column: a case report. J Med Case Reports 15, 456 (2021). https://doi.org/10.1186/s13256-021-03023-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-021-03023-w